Urinary Incontinence: What It Is and How to Take Control
If you’ve ever felt a sudden urge to pee that ends in a leak, you’re not alone. Urinary incontinence affects millions of people worldwide, yet most folks keep it hidden because they think it’s just part of aging. The truth is, many everyday habits and treatable conditions can trigger leaks, and knowing the why makes fixing it much easier.
What Triggers Urinary Incontinence?
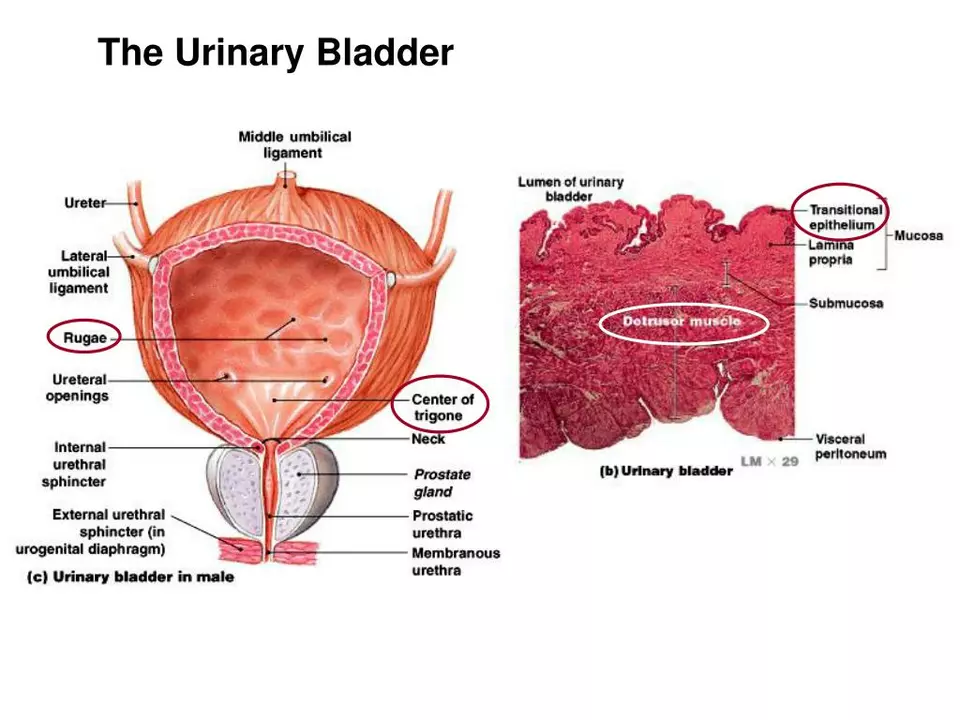
The bladder works like a balloon – it fills, signals you, then empties when you relax your pelvic muscles. When any part of that system goes off‑track, leaks happen. Common culprits include weak pelvic floor muscles (especially after pregnancy or surgery), an overactive bladder that contracts too often, and lifestyle factors such as caffeine, alcohol, or heavy lifting.
Medical conditions also play a big role. Diabetes can damage nerves that control the bladder, while prostate issues in men or uterine prolapse in women can press on the urinary tract. Certain medicines – like diuretics or antihistamines – increase urine output or dry out the tissues, making it harder to hold.
Practical Ways to Manage Leaks
The good news is that most types of incontinence improve with simple steps. Start by strengthening your pelvic floor. A quick daily routine of Kegels – squeezing the muscles you’d use to stop a stream of urine – can boost strength within weeks. Aim for three sets of ten squeezes, holding each squeeze for five seconds.
Watch what you drink. Cutting back on coffee, tea, and soda reduces bladder irritation, while staying hydrated with water helps avoid concentrated urine that can sting. If you’re prone to leaks at night, try limiting fluids two hours before bed and emptying your bladder right before you sleep.
Weight loss can be a game‑changer too. Extra pounds push on the abdomen and weaken pelvic support, so shedding even five to ten pounds often lessens urgency. Wear breathable cotton underwear instead of tight synthetic fabrics; it helps keep the area dry and reduces irritation that can trigger urges.
If home tricks aren’t enough, talk to a doctor about medical options. Prescription drugs like anticholinergics calm an overactive bladder, while topical estrogen creams help post‑menopausal women restore tissue elasticity. In more severe cases, minimally invasive procedures such as sling surgery or nerve stimulation can offer lasting relief.
Don’t forget to check out our related articles for deeper guidance: “Best Salbutamol Alternatives Worldwide” gives insight on medication safety, and “Cheap Flagyl Alternatives” shows how to compare drug costs – both useful when you’re budgeting your health care.
Living with urinary incontinence doesn’t have to hold you back. By pinpointing triggers, building stronger muscles, and using the right treatments, you can regain confidence and enjoy everyday activities without fear of a surprise leak.
The impact of bladder and urinary incontinence symptoms on exercise and physical activity
In my recent blog post, I discussed the impact of bladder and urinary incontinence symptoms on exercise and physical activity. It's surprising to know that these symptoms can significantly affect a person's confidence and willingness to participate in physical activities. As a result, many individuals experiencing incontinence tend to avoid exercises, which in turn, can lead to a decline in overall health and well-being. Fortunately, there are ways to manage these symptoms, such as using appropriate incontinence products and seeking professional help. By addressing this issue, we can help individuals regain control of their lives and stay active in spite of their bladder challenges.
read more