Birth Control Requirements: What You Need to Know Before Starting
When you’re thinking about birth control requirements, the legal, medical, and insurance rules that determine how you can access hormonal or non-hormonal contraception. Also known as contraceptive access rules, these requirements vary by state, insurance plan, and even pharmacy. It’s not just about picking a pill or patch—it’s about knowing what paperwork, exams, or approvals stand between you and the method that works for your body.
Most hormonal contraception, methods like the pill, patch, ring, or IUD that use synthetic hormones to prevent pregnancy still need a prescription in the U.S., even if they’re available over-the-counter in other countries. Your doctor will check your blood pressure, ask about blood clot risks, and review your medical history—not to delay you, but to make sure you’re not at higher risk for side effects. For teens, some states allow access without parental consent, but others require it. Insurance coverage? That’s another layer. Under the Affordable Care Act, most plans must cover FDA-approved birth control with no copay—but not all brands are included, and some insurers push you toward generics first.
Birth control access, the ability to obtain contraception without unnecessary barriers like long waits, high costs, or invasive exams isn’t just about legality—it’s about practicality. If you’re on Medicaid, you might get full coverage. If you’re uninsured, you could qualify for free or low-cost options through Title X clinics. And while some methods like condoms or the copper IUD don’t need a prescription, others like the shot or implant require a clinic visit. Even if you’re buying online, you’ll still need a valid prescription from a licensed provider. The system isn’t perfect, but knowing the rules helps you navigate it faster.
You’ll find posts here that break down real-world scenarios: how insurance tricks can make your birth control cost more than it should, why some pharmacies refuse to fill prescriptions even when they’re legal, and how to talk to your doctor when you’re not sure what’s right for you. There’s no one-size-fits-all answer, but with the right info, you can cut through the confusion and get what you need—without waiting, without shame, and without overpaying.
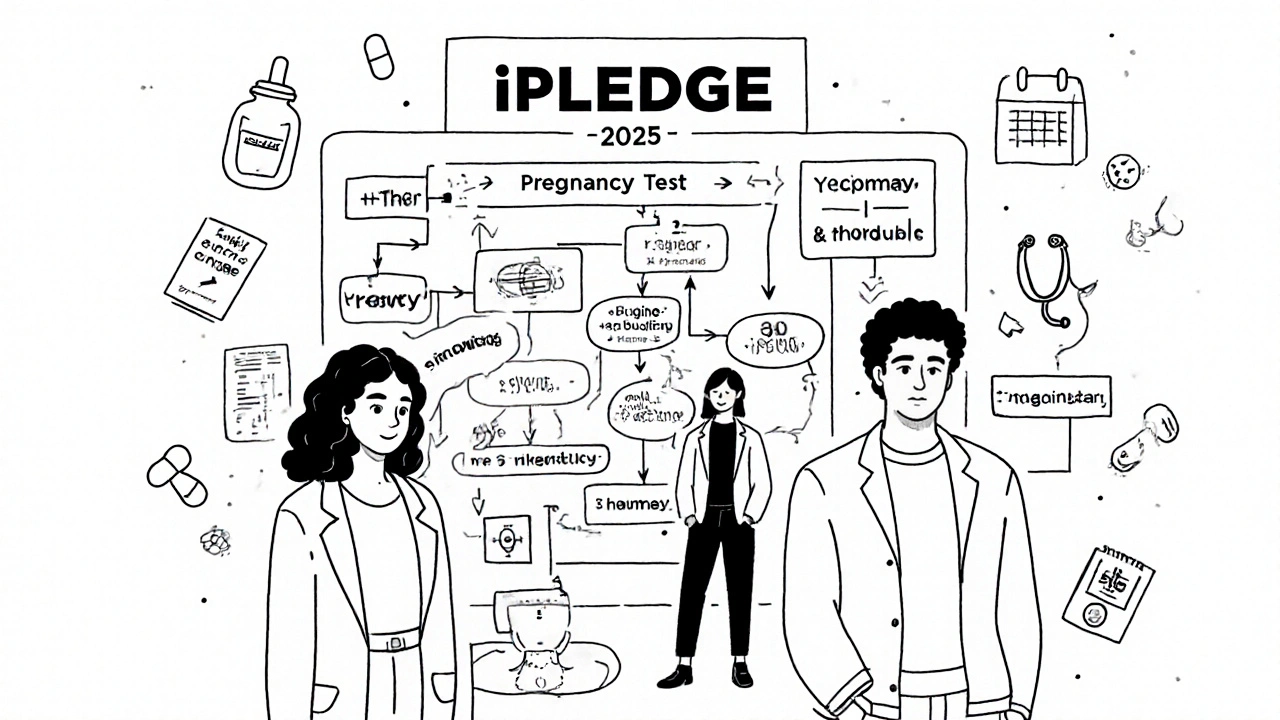
REMS for Isotretinoin: iPLEDGE Requirements and Safety in 2025
iPLEDGE is the FDA-mandated safety program for isotretinoin, designed to prevent birth defects by requiring strict pregnancy testing, birth control, and patient education. Learn the 2025 rules, changes, and how to navigate the system.
read more