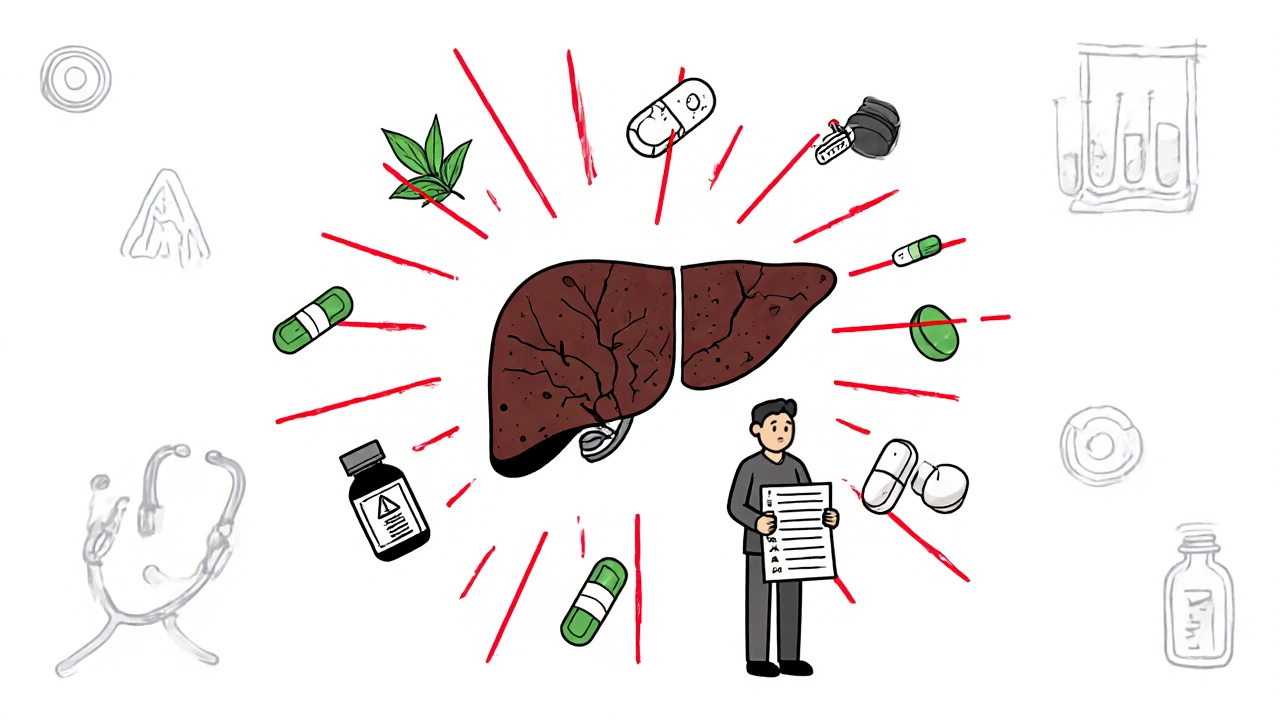
Every year, thousands of people end up in the hospital not because of a virus or bad diet, but because of something they took to feel better. Medication-related liver damage - also called drug-induced liver injury (DILI) - is one of the most dangerous and overlooked side effects of common drugs. It doesn’t always come with warning signs. By the time you feel sick, your liver might already be in serious trouble.
What Exactly Is Medication-Related Liver Damage?
It’s not just about overdosing on pills. Even normal doses of medications - including antibiotics, painkillers, and even herbal supplements - can harm your liver. The liver breaks down everything you take, and sometimes, it gets overwhelmed. That’s when toxic byproducts build up, and liver cells start to die.
According to the Drug-Induced Liver Injury Network (DILIN), this isn’t rare. About 13 to 19 out of every 100,000 people in Western countries experience it each year. Antibiotics like amoxicillin-clavulanate are the top culprits, followed by seizure medications and NSAIDs like ibuprofen. But here’s what most people don’t realize: herbal supplements and dietary products now cause 20% of all cases in the UK, and green tea extract alone is behind nearly 4 out of 10 supplement-related injuries.
Unlike viral hepatitis, DILI doesn’t spread. It’s not contagious. It’s not genetic. It’s caused by what you put into your body. And the scary part? Up to 70% of severe cases could be avoided if people knew the signs and acted fast.
How Do You Know If Your Liver Is Being Damaged?
The liver doesn’t scream. It whispers. Early signs are easy to miss because they look like the flu, stress, or just being tired.
- Unexplained fatigue that doesn’t go away
- Loss of appetite, even for food you normally love
- Nausea or vomiting that comes out of nowhere
- Dark yellow or brown urine
- Light-colored, clay-like stools
- Itching all over your skin, especially at night
These aren’t normal. If you started a new medication - even something you bought over the counter - and then these symptoms showed up, it’s not a coincidence.
The real red flags come later:
- Yellowing of the skin or eyes (jaundice)
- Pain or swelling in the upper right side of your belly
- Swelling in your legs or abdomen
- Confusion or difficulty thinking clearly
Jaundice plus any two of those other symptoms - especially if they appear within 8 weeks of starting a new drug - means you need emergency care now.
Which Medications Are Most Likely to Hurt Your Liver?
Not all drugs carry the same risk. Some are far more dangerous than others, and the timing matters just as much as the dose.
Antibiotics like amoxicillin-clavulanate (Augmentin) are the #1 cause. Injury usually shows up 1 to 8 weeks after starting them - often around day 15. People think it’s just a bad reaction to the infection, not the medicine.
Acetaminophen (Tylenol) is different. It’s safe at normal doses, but too much - even just a few extra pills - can cause rapid, life-threatening damage. Liver enzymes can spike within 24 hours. If you take more than 3,000 mg a day (or 2,000 mg if you have liver disease), you’re already in danger. Alcohol makes it worse - your risk jumps 3 to 5 times.
Anticonvulsants like valproic acid or carbamazepine take longer. Symptoms can appear after 45 days on average. People often don’t connect the dots because they’ve been on the drug for months.
Herbal supplements are the fastest-growing problem. Turmeric, green tea extract, kava, and weight-loss pills are all linked to liver failure. One Reddit user reported liver enzymes 15 times above normal from turmeric - and their naturopath told them it was just “detoxing.” That’s not detox. That’s your liver dying.
Even statins - often blamed for liver damage - are rarely the real culprit. The European Association for the Study of the Liver says fewer than 1 in 10,000 people on statins develop serious liver injury. But if you’re taking statins plus other meds or supplements, the risk goes up.

When Should You Go to the ER?
You don’t need to wait for a doctor’s appointment if you’re feeling worse. The American College of Gastroenterology gives a clear rule: If you have jaundice and any two of these - dark urine, pain in your upper right belly, or nausea/vomiting - and you started a new medication in the last 8 weeks, go to the ER immediately.
For acetaminophen overdose, time is everything. N-acetylcysteine, the antidote, works best if given within 8 hours. Every hour you wait, effectiveness drops by 10%. After 24 hours, it’s often too late to prevent permanent damage.
Don’t wait for your primary care doctor to call you back. Don’t assume it’s “just a virus.” If you’re taking a new drug and you feel off, get your liver checked. A simple blood test - ALT, AST, bilirubin, alkaline phosphatase - can tell you everything.
Why Do Doctors Miss This So Often?
Because DILI doesn’t have a single test that confirms it. It’s a diagnosis of exclusion. That means doctors have to rule out everything else - hepatitis, gallstones, autoimmune disease - before they even consider the medicine you’re taking.
A 2023 patient survey found that 68% of people with DILI were misdiagnosed at first. One woman spent three weeks being treated for “chronic fatigue” while her liver enzymes were climbing. She only got diagnosed after her skin turned yellow.
Another issue? Many doctors don’t ask about supplements. Patients assume “natural” means safe. But the FDA doesn’t regulate herbs like drugs. No safety testing. No dosage limits. No warnings. And yet, 68% of supplement users have no idea they could be hurting their liver.
Doctors are busy. But if you’re on multiple medications or supplements, you need to be the one pushing for answers. Bring a list. Ask: “Could any of these hurt my liver?”

How to Protect Yourself - Before It’s Too Late
Prevention isn’t about avoiding medicine. It’s about using it wisely.
- Know your limits. Never exceed 3,000 mg of acetaminophen per day. If you have liver disease, cut that to 2,000 mg.
- Avoid alcohol. Never mix alcohol with painkillers, antibiotics, or seizure meds. The combo is deadly.
- Track everything. Write down every pill, capsule, tea, or powder you take - even if it’s “just a supplement.” Include the dose and start date.
- Ask for liver tests. If you’re on high-risk drugs like isoniazid (used for tuberculosis), get liver enzymes checked every 4 weeks. Ten percent of users develop abnormal levels within 3 months.
- Don’t trust “natural” claims. Just because it’s sold in a health food store doesn’t mean it’s safe. Green tea extract, kava, and black cohosh have all caused liver failure.
There’s a new tool called DILI-Alert - a smartphone app that checks your meds against a database of 1,200 liver-toxic substances. It’s not perfect, but it gives you a heads-up before you start something risky.
The Bigger Picture: Why This Is Getting Worse
The number of DILI cases has jumped 27% in Europe since 2015. In the U.S., hospitalizations for liver damage from drugs rose from 8.5 to 12.3 per 100,000 people between 2010 and 2020. The cost? Around $18,500 per hospital stay.
Why? Because more people are taking supplements. More people are self-medicating. More people are ignoring warnings.
And while AI tools are now helping doctors spot DILI faster - cutting diagnosis time by 35% in early trials - most people still don’t know the signs. Only 42% of primary care doctors can correctly identify the most dangerous medications.
This isn’t just a medical problem. It’s a cultural one. We treat pills like candy. We trust marketing over science. We think if it’s sold in a bottle labeled “organic,” it can’t hurt us.
It can. And it does.
Every year, DILI causes more acute liver failure than viral hepatitis. It’s not a footnote. It’s a leading cause. And it’s entirely preventable.
Can over-the-counter painkillers cause liver damage?
Yes. Acetaminophen (Tylenol) is the most common cause of drug-related liver failure in the U.S. Taking more than 3,000 mg per day - even spread out over several doses - can damage your liver. Alcohol, existing liver disease, or taking multiple products that contain acetaminophen (like cold medicines) increase the risk. Never exceed the label dose.
Are herbal supplements safer than prescription drugs for the liver?
No. Herbal and dietary supplements cause 20% of all medication-related liver injuries in the UK, and green tea extract alone accounts for nearly 40% of those cases. Unlike prescription drugs, supplements aren’t tested for liver safety before being sold. Labels often don’t list ingredients accurately. “Natural” doesn’t mean safe.
How long does it take for liver damage to show up after starting a new medication?
It varies. Antibiotics like amoxicillin-clavulanate usually cause damage within 1 to 8 weeks, often around day 15. Anticonvulsants can take 45 days on average. Herbal supplements are the most unpredictable - symptoms can appear anywhere from 1 day to a year later. Acetaminophen overdose shows up within 24 hours. Always monitor your body for changes in the first 8 weeks after starting a new drug.
If I stop the medication, will my liver heal?
In most cases, yes - if you catch it early. Stopping the offending drug is the most important step. Many people recover fully within weeks or months. But if damage is severe or ignored, it can lead to permanent scarring (cirrhosis), liver failure, or even death. Early detection saves lives.
Should I get my liver checked before starting a new medication?
It’s a good idea if you’re taking high-risk drugs like isoniazid, certain seizure meds, or high-dose statins - especially if you drink alcohol or already have liver disease. A simple blood test for ALT and AST levels can give you a baseline. If your levels are normal before starting, and then rise sharply after, it’s a strong sign the drug is the cause.
Can I take supplements if I have liver disease?
Be extremely cautious. Many supplements - including milk thistle, turmeric, and green tea extract - can worsen liver disease. Even “supportive” herbs can be toxic when your liver is already damaged. Always talk to your hepatologist before taking anything new. What’s safe for a healthy liver may be dangerous for yours.
What to Do Next
If you’re on any medication - especially antibiotics, painkillers, or supplements - and you’ve noticed any unusual symptoms, don’t wait. Make a list of everything you take. Write down when you started each one. Then call your doctor or go to an urgent care clinic. Ask for a liver panel.
If you’ve taken too much acetaminophen - even if you feel fine - call poison control or go to the ER immediately. Don’t wait for symptoms. Time is your liver’s best friend.
Most importantly: stop assuming. Stop trusting marketing. Stop thinking supplements are harmless. Your liver doesn’t have a voice. You have to speak for it.


Comments
Sonia Festa
So let me get this straight - you’re telling me my turmeric latte is slowly turning my liver into a sad, greasy pancake? 🤯 I’ve been drinking that stuff like it’s holy water from a wellness guru. Guess I’ll be switching to… coffee. Again.
John Rendek
This is vital information that needs to be more widely known. Many people assume that because something is labeled 'natural' or 'herbal,' it’s automatically safe. That’s a dangerous myth. Always consult your doctor before starting new supplements, especially if you’re on other medications.
Ryan Tanner
My grandma took Tylenol for her arthritis and never knew it was stressing her liver. She’s fine now - caught it early because she mentioned her urine looked like cola. Don’t ignore the small signs. They’re your body’s way of whispering, 'Hey, maybe stop doing that.' 😊
Amina Kmiha
THEY KNOW. THEY KNOW what they’re doing. 🕵️♀️ The FDA, Big Pharma, the supplement industry - they’re all in cahoots. Why? Because if people knew how many 'natural' products were poisoning their livers, the multibillion-dollar wellness scam would collapse overnight. Green tea extract? A covert chemical weapon disguised as a 'detox' tea. I’ve seen the documents. They’re hiding this on purpose.
And don’t get me started on how they make you feel crazy for asking questions. 'Oh, it’s just stress.' No. It’s poison. They want you to keep buying. They want your liver to fail so they can sell you the next 'miracle cure.' Wake up.
I stopped all supplements. Went cold turkey. My enzymes dropped in 3 weeks. Coincidence? I think not.
Sara Allen
why do all these articles sound like they were written by a robot who read 500 medical journals and then got drunk on kale smoothies??
my aunt took some 'immune booster' from gnc and got sick. they said it was 'liver damage' but she swears it was the wifi in her new apartment. i mean... she’s 72. she thinks microwaves are government spies. but what if she’s right??
also i think the government puts stuff in the water to make us need more meds. that’s why we need more liver checks. it’s not the pills. it’s the water. they’re testing us.
Rebecca Parkos
I’ve been reading this entire post with tears in my eyes. My sister died from DILI after taking an herbal weight-loss pill she bought online. No one told her it could kill her. No one asked what supplements she was taking. She was 31. She had two kids. This isn’t just medical info - it’s a life-or-death wake-up call. Please, if you’re taking anything labeled 'natural,' stop. Just stop. And get tested.
Emily Barfield
What does it mean, really, when we treat our bodies as machines we can upgrade with pills and powders? We’ve outsourced our intuition to marketing slogans and Instagram influencers. We’ve forgotten that the liver isn’t a filter - it’s a living, breathing, silent witness to every choice we make. It doesn’t scream. It doesn’t beg. It just… stops. And then we wonder why we’re tired. Why we’re jaundiced. Why we’re gone.
Perhaps the real question isn’t 'Which drug is toxic?' - but 'Why do we believe we can outsmart our biology?'
And why, in a world of infinite information, do we still choose ignorance over awareness?
Ted Carr
So the solution to pharmaceutical-induced liver failure is… more pharmaceuticals? A smartphone app called DILI-Alert? That’s like putting a Band-Aid on a bullet wound and calling it innovation.
Meanwhile, in India, people have been using turmeric for 4,000 years without apps. Maybe the real problem isn’t the supplements - it’s that we’ve lost the ability to trust anything that doesn’t come with a barcode and a disclaimer.
Vrinda Bali
Let me be perfectly clear: this is not about individual negligence. This is about systemic corporate malfeasance. The entire supplement industry is built on the exploitation of Western anxiety, the commodification of wellness, and the deliberate suppression of clinical data. The FDA’s 'regulatory gap' is not an accident - it is a policy choice designed to maximize profit.
And let us not forget the role of Big Pharma: they profit from both the drugs that cause the damage AND the transplants that treat it. The cycle is engineered. The statistics? Manufactured. The warnings? Buried in footnotes.
Who benefits? Not you. Not me. The shareholders. The CEOs. The lobbyists. The ones who fund your 'educational' content.
Until we dismantle this system, no app, no blood test, no 'awareness campaign' will save you.
Albert Schueller
It's interesting how this article focuses on supplements, but completely ignores the fact that the pharmaceutical industry has been quietly lobbying for decades to keep liver toxicity data out of public view. I've reviewed several FDA whistleblower reports - many drugs with known hepatotoxic potential were approved with minimal testing. The real culprit? Regulatory capture. And yes, I'm a former lab technician. I've seen the data. It's worse than they let on.
Also, the claim that statins are 'rarely' the cause? That's statistically misleading. The studies are funded by the manufacturers. Always check the funding source.
Rahul hossain
One must question the cultural arrogance of this narrative - as if the West alone has discovered the concept of 'drug-induced liver injury.' In Ayurveda, for centuries, we have known that even 'natural' substances like aconite, kushtha, and certain forms of turmeric require precise preparation, dosage, and contraindications. The danger lies not in the herb - but in the modern ignorance of context.
Our ancestors understood that medicine is not a commodity. It is a ritual. A balance. A relationship. We have replaced wisdom with convenience - and now we are paying the price.
Perhaps the answer is not more apps - but a return to humility.
Bradley Mulliner
Everyone’s acting like this is some new revelation. Newsflash: liver damage from meds has been documented since the 1950s. The only thing that’s changed is that now people are too lazy to read labels. You think your 'clean' green tea extract is safe? You didn’t even check the label for 'standardized to 98% EGCG.' That’s like drinking battery acid and calling it 'detox.' And now you want a medal for being 'aware'?
Stop pretending you’re a victim. You made the choice. You ignored the warnings. Now you get to live with the consequences - or die. Either way, it’s on you.
Sai Ahmed
They’re watching. The liver test results. The supplement purchases. The ER visits. The data is being sold. Your health isn’t yours anymore. It’s a product. The app? A trap. It’s not helping you - it’s collecting your data so they can sell you more 'solutions.' You think they want you healthy? No. They want you dependent. The more liver damage, the more pills they sell. The more pills, the more data. The more data, the more money. It’s not a conspiracy. It’s capitalism.
Jessica Adelle
It is both a moral and civic duty to ensure that all pharmaceutical and nutraceutical agents are subject to the same rigorous pre-market scrutiny as prescription medications. The current regulatory framework is not merely inadequate - it is an abdication of the state’s responsibility to protect its citizens. The FDA’s classification of dietary supplements as 'food' rather than 'drugs' constitutes a dangerous legal fiction that endangers public health. This must be rectified through immediate legislative action. To permit the sale of untested, unregulated, and potentially lethal substances under the guise of 'personal freedom' is not liberty - it is negligence.