REMS: What It Is, Why It Matters, and How It Protects You
When you take a powerful medication—like one that can cause liver damage, birth defects, or severe allergic reactions—there’s a system in place to make sure you don’t get hurt. That system is called REMS, a Risk Evaluation and Mitigation Strategy mandated by the U.S. Food and Drug Administration to manage serious risks of certain medications. Also known as Risk Evaluation and Mitigation Strategy, it’s not just paperwork. It’s a real-world safety net that can mean the difference between life and death. REMS isn’t about keeping drugs off the market. It’s about letting them stay on the market, but only if you and your doctor follow specific rules to stay safe.
REMS programs show up in different forms. Some require you to sign a form before getting your prescription. Others force pharmacies to track every dose. Some even demand regular blood tests or pregnancy checks. For example, if you’re prescribed isotretinoin (Accutane), you’re enrolled in a REMS program that tracks your monthly lab results and birth control use. The same goes for thalidomide—a drug that once caused terrible birth defects and now can’t be dispensed without strict enrollment. These aren’t arbitrary rules. They’re based on real data from patients who’ve been harmed because the risks weren’t properly managed.
REMS also involves healthcare providers, doctors, pharmacists, and nurses who must be certified to prescribe or dispense certain high-risk medications. They don’t just hand out pills. They complete training, log patient info, and sometimes even verify that you’ve received counseling. And it’s not just about the patient. pharmacies, the places you pick up your meds, must also be certified under REMS to handle restricted drugs. This isn’t bureaucracy—it’s a chain of responsibility. If one link fails, the system catches it.
You might wonder why this matters to you if you’re not taking a high-risk drug. The truth is, REMS is changing how all medications are monitored. The FDA now uses REMS-like tools for more drugs every year. The same logic that protects people from thalidomide is now being applied to painkillers, antibiotics, and even diabetes meds. What you’re seeing is the future of drug safety: not just warnings on labels, but active, ongoing control. And it’s working. Studies show REMS programs have reduced serious side effects by up to 40% for some drugs.
Below, you’ll find real stories and guides from people who’ve dealt with REMS firsthand. You’ll learn how to navigate the paperwork, what to ask your doctor, how to avoid delays, and when a REMS requirement might be unnecessary. Whether you’re managing a chronic condition, helping an elderly parent, or just trying to understand why your prescription came with extra steps—this collection gives you the clarity you need to stay safe without being scared.
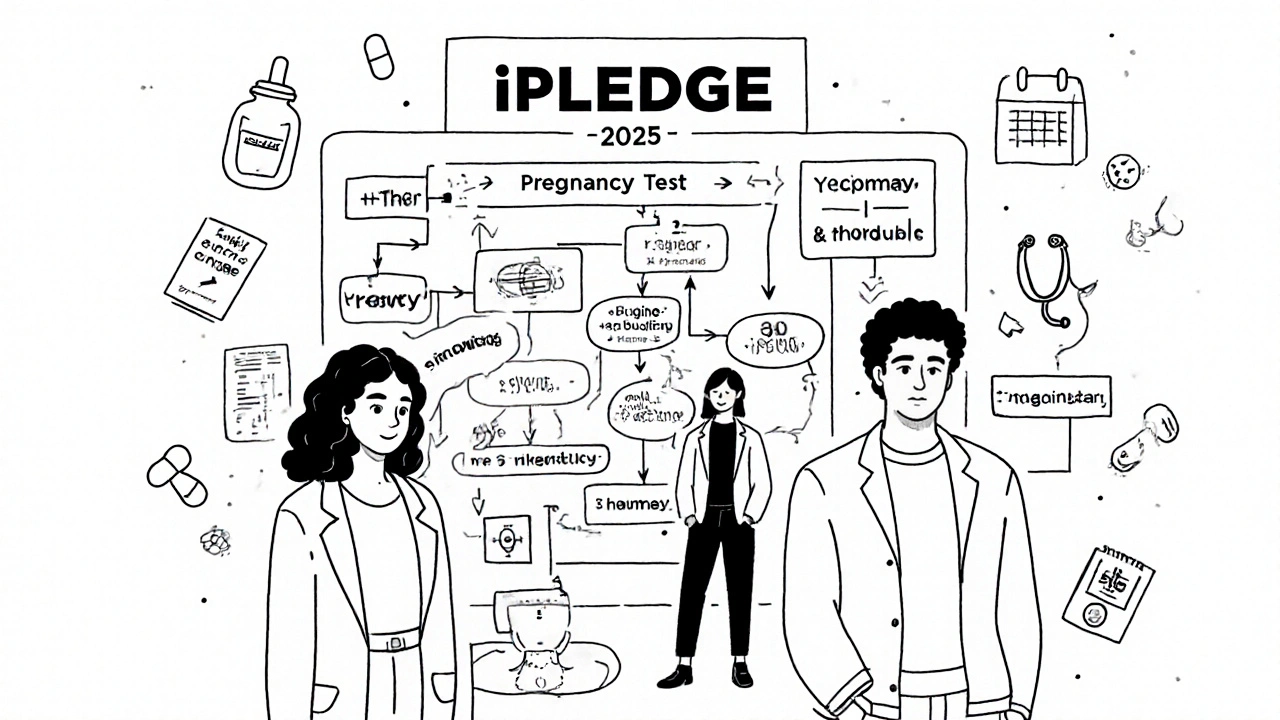
REMS for Isotretinoin: iPLEDGE Requirements and Safety in 2025
iPLEDGE is the FDA-mandated safety program for isotretinoin, designed to prevent birth defects by requiring strict pregnancy testing, birth control, and patient education. Learn the 2025 rules, changes, and how to navigate the system.
read more