
When you’re pregnant, even a simple headache or stuffy nose can turn into a stressful decision. You don’t want to suffer, but you also don’t want to risk your baby’s health. That’s why so many women reach for over-the-counter (OTC) meds - they’re easy, fast, and seem harmless. But here’s the truth: OTC medications during pregnancy aren’t all safe, and not all are safe at every stage. What you think is harmless could carry hidden risks. The key isn’t avoiding all meds - it’s knowing what to ask before you take anything.
What’s Actually Safe? Start with Acetaminophen
Acetaminophen (Tylenol) is still the go-to pain reliever and fever reducer recommended by doctors during pregnancy. It’s been used by millions of pregnant women for decades, and current evidence shows it’s the safest option when used correctly. The standard dose is 650 to 1,000 mg every 4 to 6 hours, not exceeding 4,000 mg in 24 hours. That’s about six regular-strength tablets a day.
But even acetaminophen isn’t risk-free if misused. Long-term, high-dose use - especially in the second trimester - has been linked in some recent studies to possible effects on fetal brain development. These findings aren’t conclusive, but they’re enough to make experts urge caution. Don’t take it for weeks on end just because you can. Use the lowest dose for the shortest time possible. If you’re taking it more than a few days a week, talk to your provider.
Stay Away from NSAIDs After 20 Weeks - and Be Careful Earlier
Ibuprofen (Advil, Motrin) and naproxen (Aleve) are common painkillers, but they’re dangerous during pregnancy after 20 weeks. The FDA issued a clear warning in 2020: these drugs can cause serious kidney problems in the unborn baby, reduce amniotic fluid, and even lead to heart complications. That’s why you’ll see strong labels on every bottle.
But the risk doesn’t start at 20 weeks. Studies show that using NSAIDs in the first trimester may increase the chance of miscarriage by up to 60%. Even short-term use - like taking two pills for a bad headache - can pose a risk. If you’ve taken ibuprofen early in pregnancy, don’t panic. But do tell your provider. They’ll monitor your pregnancy more closely if needed.
Cold and Allergy Meds: Not All Are Created Equal
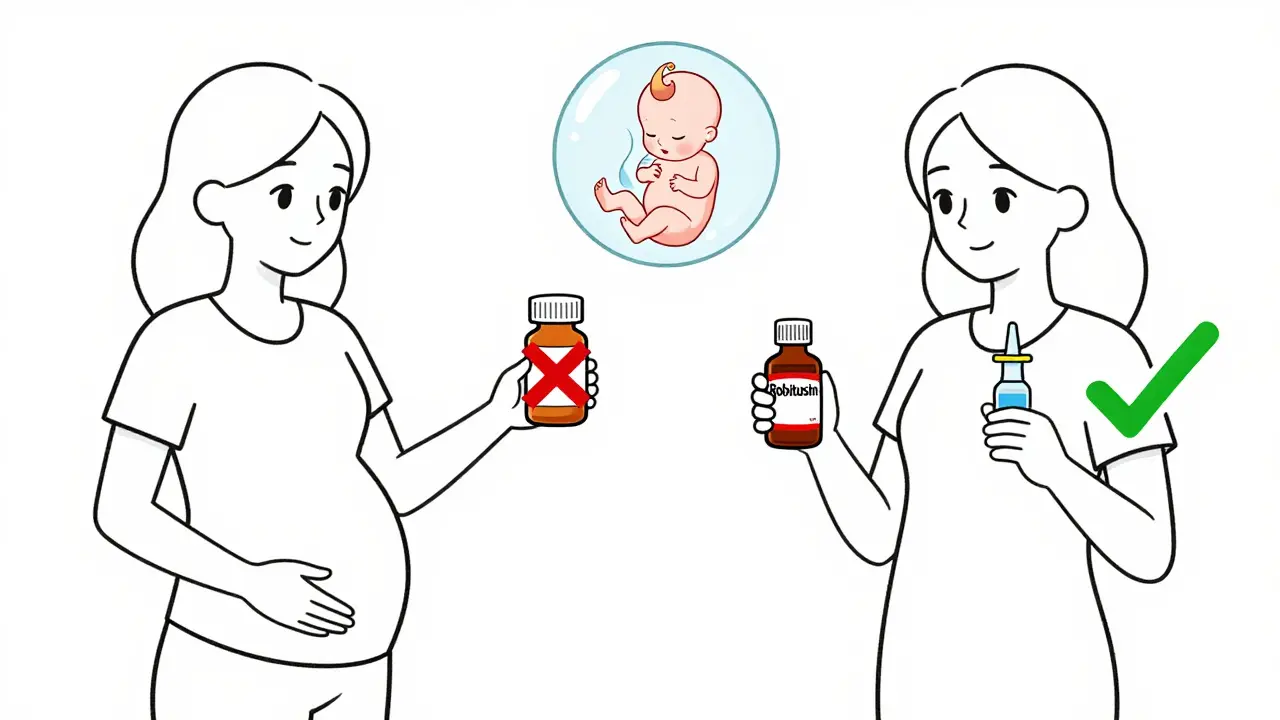
When you have a cold, you might grab a multi-symptom product because it’s convenient. But that’s exactly what you should avoid. Many cold medicines combine ingredients - some safe, some not. For example, plain Robitussin (just dextromethorphan) is okay for coughs. But Robitussin Multi-Symptom? That one has phenylephrine, which is linked to birth defects if taken in the first trimester.
Decongestants like pseudoephedrine (Sudafed) are especially risky early on. Research shows they can double the risk of a rare abdominal wall defect called gastroschisis if taken in the first 12 weeks. That’s why most doctors say: skip pseudoephedrine entirely in the first trimester. If you need relief later, use it only briefly and under supervision.
For allergies, loratadine (Claritin) and cetirizine (Zyrtec) are considered safe throughout pregnancy. Fexofenadine (Allegra) was added to the safe list in 2023 after a large study of over 12,000 pregnancies showed no increased risk of birth defects. But avoid diphenhydramine (Benadryl) unless your provider says it’s okay - it can cause drowsiness and may affect fetal heart rate in some cases.
Heartburn? Try Tums - But Watch the Dose
Heartburn is super common during pregnancy. Calcium carbonate (Tums) is one of the safest options. It works by neutralizing stomach acid and even gives you extra calcium, which you need. But don’t go overboard. Stick to under 2,000 mg per day. Too much calcium can cause constipation or kidney stones.
Other safe choices include aluminum and magnesium hydroxide combinations (like Maalox or Mylanta) and famotidine (Pepcid AC). These are fine for occasional use. Avoid ranitidine (Zantac) - it was pulled from the market in 2020 due to contamination concerns, and it’s still not available in most countries.
Diarrhea and Yeast Infections: What You Can and Can’t Use
Diarrhea might feel minor, but dehydration during pregnancy can be dangerous. Loperamide (Imodium) is generally safe if you don’t have a fever and you follow the label instructions. But if diarrhea lasts more than two days, call your provider - it could be an infection.
For yeast infections, topical antifungals like clotrimazole (Lotrimin) are safe. They’re applied directly to the skin or vaginal area and don’t enter your bloodstream in significant amounts. But oral antifungals like fluconazole? Avoid them. Even a single high dose has been linked to rare birth defects. Always check with your doctor before using any antifungal, even if it’s sold over the counter.
The 5 Questions You Must Ask Before Taking Anything
Don’t just assume it’s safe because it’s on the shelf. Use this simple checklist before you open any bottle:
- Is this medication absolutely necessary? Can you manage symptoms with rest, hydration, saltwater gargles, or a humidifier?
- What’s the lowest effective dose? Start with half the recommended dose if you’re unsure. Less is often better.
- How long will you use it? No more than 2-3 days unless your provider says otherwise.
- Are there non-drug options? Ginger for nausea, warm compresses for sinus pressure, and elevating your head at night for heartburn can all help.
- Has your provider approved this exact product? Brand names matter. A cough syrup labeled "alcohol-free" might still contain 5-10% ethanol. Check the full ingredient list.
Many women don’t realize that two products with the same active ingredient can have different inactive ingredients. One might contain alcohol, artificial sweeteners, or dyes that aren’t recommended during pregnancy. Always read the full label - not just the front.
What You Should Do Before You Get Pregnant
Waiting until you’re pregnant to think about meds is too late. If you’re planning a pregnancy, schedule a preconception visit. Bring a list of everything you take - prescription, OTC, supplements, and herbal remedies. Your provider can help you switch to safer options before conception.
Women with chronic conditions like asthma, depression, or high blood pressure are especially at risk if they stop meds abruptly. Stopping your seizure medication or antidepressant without guidance can be more dangerous than continuing a safe one. Work with your doctor to create a pregnancy-safe plan ahead of time.

Why So Many Women Get It Wrong
One study found that 32% of pregnant women start taking OTC meds without telling their provider. The most common reasons? They think it’s harmless, they’re in a hurry, or they don’t want to bother their doctor.
But here’s what most don’t know: 18% of medication-related pregnancy complications come from "innocent-looking" OTC drugs - especially decongestants and herbal products labeled "natural." Just because something is herbal doesn’t mean it’s safe. Black cohosh, dong quai, and goldenseal can trigger contractions or affect fetal development.
Another issue? Label confusion. Only 37% of multi-symptom cold products clearly state pregnancy risks on the label. Meanwhile, 89% of acetaminophen and antacid labels do. That means you can’t rely on the packaging - you need to ask.
What’s Changing in 2025
Research is evolving. The Acetaminophen Use in Pregnancy (AUP) Study, tracking 50,000 pregnancies, is expected to release final results in late 2025. This could change how we view acetaminophen long-term.
Also, new genetic research shows that 23% of pregnant women have a gene variant (CYP2E1) that changes how their body breaks down acetaminophen. This means standard doses might be too high for some, increasing the risk of liver stress. In the future, doctors may test for this before recommending doses.
For now, stick to the basics: use the least amount for the shortest time. And when in doubt - ask.
Is Tylenol safe during pregnancy?
Yes, acetaminophen (Tylenol) is the safest pain reliever and fever reducer during pregnancy when used as directed - no more than 4,000 mg per day. But avoid long-term or high-dose use, as emerging research suggests possible links to neurodevelopmental effects. Always use the lowest dose for the shortest time.
Can I take ibuprofen while pregnant?
No, avoid ibuprofen and other NSAIDs after 20 weeks of pregnancy. They can cause serious kidney problems in the baby and reduce amniotic fluid. Even before 20 weeks, they may increase miscarriage risk. Use acetaminophen instead for pain or fever.
What cold medicine is safe during pregnancy?
Stick to single-ingredient products: plain Robitussin (dextromethorphan only) for cough, loratadine (Claritin) or cetirizine (Zyrtec) for allergies, and saline nasal sprays for congestion. Avoid multi-symptom formulas - they often contain unsafe ingredients like phenylephrine or pseudoephedrine.
Are herbal remedies safe during pregnancy?
No. Many herbal products marketed as "natural" or "safe" can be dangerous. Black cohosh, goldenseal, and dong quai may trigger contractions or affect fetal development. Always check with your provider before using any supplement or herb.
Should I stop all medications when I find out I’m pregnant?
No. Stopping necessary medications - like those for asthma, seizures, or depression - can be more harmful than continuing them. Work with your provider to switch to pregnancy-safe options before or as soon as you find out you’re pregnant. Never stop a prescription without medical advice.
How do I know if a product contains unsafe ingredients?
Always read the "Active Ingredients" and "Inactive Ingredients" list on the label. Avoid products with pseudoephedrine, phenylephrine, alcohol, or unlisted herbs. When in doubt, take the bottle to your pharmacist or provider and ask: "Is this safe during pregnancy?"
Next Steps: What to Do Today
If you’re pregnant and taking any OTC meds - even just once a week - make a list. Write down every product, brand, dose, and reason you’re taking it. Bring it to your next appointment. If you’re planning pregnancy, do the same now. Don’t wait for symptoms to appear.
Keep a small notebook or use your phone to track what you take. Over time, you’ll notice patterns - and you’ll be better prepared to make smart choices. Your body is doing something incredible. The least you can do is give it the safest support possible.


Comments
ANA MARIE VALENZUELA
Let’s be real - if you’re taking Tylenol like it’s candy because ‘it’s safe,’ you’re already doing it wrong. I’ve seen women pop 10 tablets a day for weeks because ‘it’s just acetaminophen.’ Newsflash: it’s not a vitamin. That ‘emerging neurodevelopmental risk’? It’s not hypothetical. I’m a nurse. I’ve seen the charts. Stop self-medicating like you’re at a rave.
Samantha Hobbs
omg i took ibuprofen at 8 weeks and now i’m terrified 😭 i didn’t know!! my doctor never said anything. is my baby gonna be ok??
Vu L
Acetaminophen is fine. The real danger is the medical-industrial complex turning every pregnancy into a liability lawsuit waiting to happen. You’re not a lab rat. If you feel fine, take the pill. Stop listening to fearmongering studies funded by pharma.
James Hilton
So let me get this straight - you’d rather suffer through a migraine than take a pill that’s been used by 10 million moms? 🤦♂️ Welcome to the ‘natural’ cult where ‘harmless’ means ‘I’m gonna cry in the bathroom for 3 hours.’
Teresa Marzo Lostalé
i just sat here reading this and thought… we’ve turned pregnancy into a full-time job of risk assessment. every cough, every headache, every sneeze - now it’s a decision tree with footnotes. i miss when we just took a pill and trusted our bodies. 🤷♀️
Celia McTighe
thank you for this. i’ve been so scared to even take a tums 😅 i just wanted to say - you’re not alone. i’ve been using zyrtec and plain robitussin and it feels like a win. also, ginger tea is my new best friend 🌿💛
Ryan Touhill
It’s not merely about pharmacokinetics - it’s about epistemological authority. The FDA’s 2020 advisory is a symptom of a broader regulatory capture by Big Pharma, wherein safety thresholds are deliberately obfuscated to maintain market viability. The 23% CYP2E1 polymorphism data? That’s not ‘emerging research’ - it’s a systemic failure in personalized medicine. If you’re not genotyping before dosing, you’re not practicing medicine. You’re gambling.
Gran Badshah
in india we just take paracetamol and call it a day. no one reads labels. if it's in the pharmacy, it's fine. why are you making it so complicated?
Ellen-Cathryn Nash
you people are disgusting. you treat your bodies like vending machines - pop a pill, get relief. but this isn’t about convenience. this is about sanctity. if you can’t endure a headache without poisoning your child, maybe you shouldn’t have gotten pregnant. 🙄
Nicole Beasley
wait so is fexofenadine really safe? i saw a study from 2023 but i can’t find the link anymore 😅 can someone send it? also, what about peppermint tea for nausea?
sonam gupta
western medicine is overrated. in india we use hing water for gas and neem oil for rashes. why are you scared of natural things? you are all addicted to chemicals
Julius Hader
I’ve been taking Tums daily since week 6. I know I’m not supposed to, but I just feel better. I don’t want to be one of those ‘perfect pregnant women’ who eats kale and meditates through contractions. I’m just trying to survive.
Mimi Bos
just wanted to say i accidentally took two motrin at 12 weeks and now i’m crying in the shower. i feel like such a bad mom. i didn’t even know it was bad until i read this. thank you for writing this. i’m gonna take my list to my appt tomorrow.
Payton Daily
look. the real truth? pregnancy isn’t about safety. it’s about control. they want you to be scared. they want you to ask permission for every sneeze. they want you to feel guilty for breathing too hard. you’re not a lab. you’re a woman. take the damn pill. live your life. the world doesn’t need more anxious moms.