When you’re pregnant, your body changes in ways you never expected. One of the most surprising? Your pancreas has to work harder than ever. Around weeks 24 to 28, hormones from the placenta start blocking insulin - your body’s natural blood sugar regulator. If your pancreas can’t keep up, your blood sugar rises. That’s gestational diabetes. It’s not your fault. It’s not because you ate too much sugar. It’s biology. And the good news? With the right tools, you can keep it under control and have a healthy pregnancy.
What Happens When Blood Sugar Goes Up During Pregnancy?
Your body needs insulin to move glucose from your blood into your cells for energy. During pregnancy, hormones like progesterone and human placental lactogen make your cells less sensitive to insulin. This is normal - it ensures your baby gets enough glucose. But if your pancreas can’t produce enough extra insulin to compensate, glucose builds up in your bloodstream. That’s gestational diabetes. The numbers matter. According to the American Diabetes Association, your target blood sugar levels during pregnancy are:- Fasting or before meals: below 95 mg/dL (5.3 mmol/L)
- One hour after eating: below 140 mg/dL (7.8 mmol/L)
- Two hours after eating: below 120 mg/dL (6.7 mmol/L)
How Is Gestational Diabetes Diagnosed?
Most women get screened between 24 and 28 weeks. The first test is a 50-gram glucose challenge. You drink a sweet liquid, wait an hour, and get your blood drawn. If your result is above 140 mg/dL, you’ll need a follow-up test: a 3-hour, 100-gram oral glucose tolerance test. This one’s stricter. You fast overnight, then get your blood drawn four times over three hours after drinking a more concentrated sugar solution. If two or more readings are too high, you’re diagnosed. Some clinics use a lower cutoff - 130 mg/dL - to catch more cases early. That’s because early detection means better outcomes. If you have risk factors - like being over 35, having a BMI over 30, a history of gestational diabetes, or a family history of Type 2 diabetes - your provider might test you earlier, even in your first trimester.Managing Blood Sugar Without Medication
About 70 to 85% of women with gestational diabetes can manage their levels with diet and movement alone. No insulin needed. But it takes structure. Carbohydrates are the key. Not because they’re bad - because they’re the biggest driver of blood sugar spikes. The goal is to spread them out and pair them wisely.- Choose complex carbs: whole grains, legumes, oats, quinoa, sweet potatoes
- Avoid refined carbs: white bread, pastries, sugary cereals, juice
- Limit carbs per meal to about 45 grams - that’s one cup of cooked rice, two slices of whole wheat bread, or three-quarters of a cup of oatmeal
- Include 15-30 grams of carbs in each snack
- Don’t skip meals. Eat three meals and two to three snacks daily
Exercise: The Secret Weapon
You don’t need to run a marathon. Just move. Walking for 30 minutes, five days a week, can lower your blood sugar by 20-30 mg/dL after meals. Do it 15 to 30 minutes after eating. That’s when glucose is peaking. A brisk walk after dinner? That’s your best defense against nighttime highs. Swimming and prenatal yoga are also great. Avoid high-impact activities or anything with a fall risk. Always check with your provider before starting a new routine.
When You Need Insulin or Medication
If diet and exercise aren’t enough after a few weeks, your provider will likely recommend insulin. It’s safe for your baby. It doesn’t cross the placenta. And it’s often the most effective option. Some women are prescribed metformin, an oral medication used for Type 2 diabetes. But it’s not first-line. Studies show about 30% of women on metformin still need insulin later. The long-term effects on babies are still being studied. Insulin is given by injection - usually in the belly or thigh. Many women worry about this at first. But once they try it, most say it’s easier than they thought. Your diabetes educator will show you how to use the pen, store it, and track your doses. You’ll learn to adjust based on your readings.Monitoring: The Daily Routine
You’ll need to check your blood sugar 4 to 6 times a day. That sounds overwhelming. But it’s the only way to know what’s working. Here’s a typical schedule:- Fasting - right when you wake up
- One hour after breakfast
- One hour after lunch
- One hour after dinner
- Optional: bedtime or 2 hours after snacks
What About Postpartum?
After your baby is born, your blood sugar usually drops back to normal. That’s good news. But here’s the catch: about half of women with gestational diabetes will develop Type 2 diabetes within 10 years. That’s not a guarantee - it’s a warning. You’ll need a follow-up glucose test 6 to 12 weeks after delivery. This is usually a 75-gram oral glucose tolerance test. If your fasting level is above 126 mg/dL or your 2-hour level is above 200 mg/dL, you have Type 2 diabetes. If it’s between those numbers, you have prediabetes. This is your chance to change course. Lose 5-7% of your body weight. Get 150 minutes of exercise a week. Eat more fiber, less processed food. The TODAY2 study showed that doing this cut the risk of Type 2 diabetes by 58% over 15 years.
What Doesn’t Work
Don’t try to cut carbs completely. Your baby needs glucose. Your brain needs it. Starving yourself won’t help - it’ll make you tired, irritable, and at risk for ketosis, which can harm your baby. Don’t ignore fasting highs. They’re common. They’re fixable. A bedtime snack with protein and a little carb often helps. Don’t rely on advice from random online forums. Reddit and Facebook groups can be helpful for emotional support, but dietary advice varies wildly. Stick to what your certified diabetes educator or registered dietitian says.Support Is Available - Use It
You’re not alone. Most hospitals have certified diabetes care and education specialists (CDCES). They’ll walk you through carb counting, glucose logs, and insulin use. Many offer phone support. One study found 78% of women got their urgent questions answered within 24 hours. Join a support group. Women who felt supported were 85% more satisfied with their care. The American Diabetes Association has a free “Healthy Eating for Pregnancy” guide. The CDC offers a postpartum transition plan. Use them.Final Thought: You’re Doing Better Than You Think
It’s hard. You’re tired. You’re worried. You’re counting carbs like a scientist. But if you’re checking your numbers, eating well, moving daily, and showing up for your appointments - you’re doing everything right. Studies show that women who keep their blood sugar in target have pregnancy outcomes nearly identical to those without gestational diabetes. Your baby is not at risk because of this diagnosis. They’re at risk because of what you do next. And you’re already doing the right thing by reading this.Can gestational diabetes go away after pregnancy?
Yes, in about 70% of cases, blood sugar levels return to normal after delivery. However, this doesn’t mean you’re out of the woods. Up to 50% of women who had gestational diabetes will develop Type 2 diabetes within 10 years. That’s why follow-up testing at 6-12 weeks postpartum is critical - and why lifestyle changes after birth matter just as much as during pregnancy.
Will my baby have diabetes because I had gestational diabetes?
No, your baby won’t be born with diabetes. But they may have a higher risk of developing obesity and Type 2 diabetes later in life. This risk is linked to high blood sugar exposure in the womb, which can affect how their metabolism develops. The good news? Breastfeeding and healthy feeding habits after birth can significantly lower that risk.
Do I need to avoid all sugar if I have gestational diabetes?
You don’t need to eliminate sugar completely - but you do need to be smart about it. Natural sugars in fruit, milk, and yogurt are fine in controlled portions. Avoid added sugars in soda, candy, pastries, and sweetened drinks. The goal isn’t perfection; it’s balance. Pairing carbs with protein or fat slows sugar absorption, so a small piece of dark chocolate with nuts is better than a cookie alone.
Can I still have a vaginal birth if I have gestational diabetes?
Absolutely. Most women with well-managed gestational diabetes have normal vaginal deliveries. The main concern is if the baby grows too large, which increases the risk of birth injuries. But if your blood sugar has been controlled, your baby’s size will likely be normal. Your provider will monitor growth with ultrasounds, but birth plan decisions - including vaginal delivery - are still yours.
Why do I have high blood sugar in the morning even if I didn’t eat?
That’s called the dawn phenomenon. Around 4-5 a.m., your body releases hormones that naturally raise blood sugar to prepare you for the day. During pregnancy, insulin resistance makes this effect stronger. A small bedtime snack with protein and a little complex carb - like cheese and whole grain crackers - can help stabilize overnight levels. If it persists, your provider may adjust your eating pattern or recommend insulin.
Is gestational diabetes my fault?
No. It’s not caused by eating too much sugar or being lazy. It’s caused by hormones your body makes during pregnancy. Risk factors like age, weight, family history, or ethnicity can increase your chance - but even women who are thin and fit can develop it. This is a physiological change, not a personal failure. The fact that you’re managing it means you’re doing everything right.
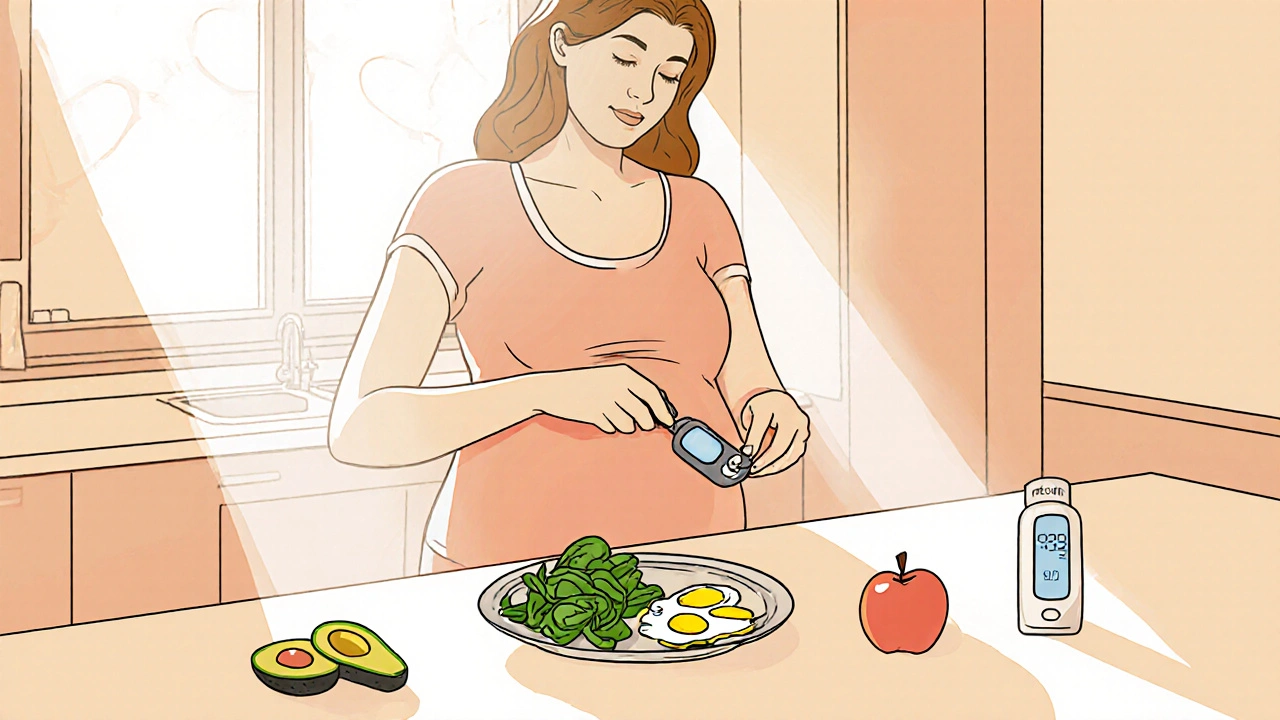
What should I eat for breakfast if I have gestational diabetes?
Skip the cereal and toast. Instead, aim for protein and healthy fats to keep blood sugar steady. Good options: scrambled eggs with spinach and avocado, Greek yogurt with chia seeds and berries, or cottage cheese with sliced almonds. Include about 15-30 grams of carbs total. A small apple with peanut butter works too. Avoid fruit juice, muffins, and sugary cereals - they spike sugar fast.
Can I use a fitness tracker or app to help manage gestational diabetes?
Yes. Apps like MyFitnessPal or MySugr can help track carbs, meals, and glucose readings. Many women find them useful for spotting patterns. But don’t rely on them alone. Always cross-check with your glucose meter and your healthcare team. Apps can’t replace professional guidance - but they’re great tools when used correctly.


Comments
Elizabeth Choi
Just got diagnosed last week. Honestly? I thought I was eating healthy. Turns out my 'healthy' oatmeal with banana was a sugar bomb. Now I'm doing protein-first meals and walking after dinner. Blood sugar dropped 40 points in three days. Still terrifying, but at least I feel like I'm not helpless.
Also, the dawn phenomenon is real. Woke up at 135 this morning. Ate cheese and crackers before bed. Down to 98. Small wins.
Allison Turner
Ugh. More guilt-tripping from the medical industrial complex. You’re not a lab rat. Just eat real food and stop obsessing over numbers. I had two kids with no testing and they’re fine.
Darrel Smith
Let me tell you something. This isn't just about sugar. This is about your body being hijacked by corporate medicine. They want you on insulin so they can keep selling you pens. They want you tracking every bite because they profit off your fear. I know this because I read the FDA documents. They’ve been pushing this 'gestational diabetes' narrative since the 90s to push processed meal replacements and glucose monitors. You don’t need to test four times a day. You need to trust your body. Eat whole foods. Walk. Breathe. Stop letting them turn pregnancy into a surveillance state.
And if your doctor says you need insulin? Get a second opinion. Or better yet - go to a midwife. They’ve been doing this for centuries without a glucometer.
Aishwarya Sivaraj
Hey I had GD too and it was rough at first but honestly the protein first trick changed everything for me
I used to eat rice and beans for lunch and spike to 180 then I started with eggs then veggies then half a sweet potato and boom 110
Also dont stress about the fasting numbers too much if they are high its usually dawn phenomenon and a small snack before bed helps
you are not failing you are adapting and that is powerful
Iives Perl
They’re watching you. The glucose monitor. The app. The 4x daily checks. They’re building a profile. One day they’ll use this data to deny you insurance. Or tag your baby as 'high risk' for life. You think this is about health? It’s about control. 🤫👁️
Jebari Lewis
I appreciate the data-driven approach here. The evidence is unequivocal: glycemic control reduces macrosomia by 67%, neonatal hypoglycemia by 52%, and C-section rates by 29%. The ADA guidelines are not arbitrary-they are meta-analyzed, peer-reviewed, and prospectively validated. Ignoring them is not 'natural parenting.' It's statistically dangerous. If you're skeptical, review the HAPO study. The numbers don't lie. You owe it to your child to follow protocol.
Emma louise
Oh look, another 'science says' pamphlet from Big Obstetrics. In Sweden, they don’t even test for this. Kids are still born. Still healthy. Why are we pathologizing normal biology? You’re not a diabetic. You’re pregnant. Stop letting doctors turn your womb into a diabetes clinic.
Mira Adam
It’s not about blood sugar. It’s about sovereignty. Your body is not a machine to be calibrated. It’s a living, breathing ecosystem that knows how to nourish a child without charts or insulin pens. We’ve been pregnant for 200,000 years without a glucometer. Why are we suddenly broken? This isn’t medicine. It’s colonization of the female body.
Miriam Lohrum
There’s something deeply human about this. We’re taught to fear our own biology. To measure, to control, to optimize. But pregnancy reminds us that some things can’t be quantified. The love you feel when your baby kicks after a walk? That’s not on a glucose log. The peace of eating a banana with almond butter because you listened to your body? That’s the real treatment.
Do the numbers. But don’t let them define you.
Sue Haskett
Hi! I just wanted to say-YOU’RE DOING AMAZING! Seriously. Even if your numbers aren’t perfect, just showing up, reading this, trying the protein-first trick, walking after meals? That’s heroic. I had GD with both kids, and I cried over every 145 reading. But guess what? My kids are 8 and 10, and they’re both thriving. You are not failing. You are fighting. And you’re not alone. I’m here if you need to vent. Or just say ‘I had a bad day with my glucose meter.’ I get it. 💕
Jauregui Goudy
Okay real talk-I was terrified of insulin. Thought it meant I 'failed.' But after my numbers stayed high for two weeks, I tried it. The pen is tiny. The needle? Barely a pinch. And within 48 hours, my baby’s growth chart stopped skyrocketing. It’s not a punishment. It’s a tool. Like a seatbelt. You don’t feel guilty for buckling in. You feel safe. You’ve got this.
Tom Shepherd
just tried the protein first thing and my post lunch sugar went from 156 to 112. no joke. also walking after dinner is a game changer. i used to sit on the couch after eating now i walk around the block. feels good. also i stopped drinking orange juice. that was my downfall. who knew?
Rhiana Grob
Thank you for this comprehensive, compassionate, and clinically grounded guide. The balance of scientific rigor and emotional support is exactly what is missing from so many pregnancy resources. I especially appreciate the emphasis on postpartum follow-up-this is the most critical phase, yet it’s often overlooked. I hope every provider distributes this material. You’ve turned fear into agency.
Frances Melendez
Of course you're doing everything right. You're also probably the one who's been eating kale smoothies since week 1 and still spiked to 160. Meanwhile, my cousin ate pizza and ice cream every night and had a 7-pound baby with no insulin. So maybe the whole system is rigged. Maybe you're being manipulated into a lifestyle you don't even need. Just saying.