Side Effect Comparison Tool
How This Tool Works
See how side effects reported in controlled clinical trials differ from those observed in real-world use. Based on real-world data from the FDA's FAERS and clinical trial data from typical Phase 3 studies.
Clinical Trial Data Small Sample Size
Typical Phase 3 clinical trial with 381 participants over 6 months
Real-World Data Millions of Users
Data from 300 million patient records and 2.1 million reports over 10+ years
Why This Matters
Remember: Clinical trials tell you what a drug can do under ideal conditions. Real-world data shows what it actually does when millions of people use it in real life.
As shown in the rosiglitazone case from the article: Clinical trials didn't detect a 43% higher risk of heart attacks. That's why the FDA now requires real-world evidence in 67% of new drug approvals (up from 29% in 2017).
When you take a new medication, you’re relying on two very different kinds of information to understand what might go wrong. One comes from tightly controlled clinical trials. The other comes from millions of real people using the drug every day. These aren’t just two sources of side effect data-they’re two different worlds. And knowing the difference can change how you think about your health.
What Clinical Trials Actually Show
Clinical trials are designed to answer one question: does this drug work under ideal conditions? To do that, they isolate variables. Participants are carefully selected. They’re monitored weekly. Every headache, rash, or dizziness is recorded using a standardized system called the Common Terminology Criteria for Adverse Events (CTCAE), which lists 790 specific side effects with clear severity levels-from mild (Grade 1) to fatal (Grade 5). But here’s the catch: these trials rarely include people who are most likely to use the drug in real life. Elderly patients with multiple conditions, pregnant women, children, and those on five or more medications are often excluded. The average Phase 3 trial for cancer drugs enrolls just 381 people. That’s not enough to catch side effects that happen in 1 in 1,000 or 1 in 10,000 patients. Take rosiglitazone, a diabetes drug approved in 1999. Clinical trials didn’t flag a major heart risk. But after millions of people started using it, real-world data revealed a 43% higher chance of heart attacks. The trial was too small, too clean, too short. It missed what happens when a drug meets the messy reality of human biology.What Real-World Data Reveals
Real-world side effect data doesn’t come from clinics with strict protocols. It comes from pharmacies, emergency rooms, patient apps, insurance claims, and doctors’ notes. The FDA’s Adverse Event Reporting System (FAERS) got over 2.1 million reports in 2022 alone. That’s up from 1.4 million in 2018. These aren’t perfect records. Many go unreported. Only 2-5% of actual side effects make it into official databases, according to the Agency for Healthcare Research and Quality. But scale compensates for noise. IBM MarketScan tracks 200 million lives annually. The FDA’s Sentinel Initiative monitors 300 million patient records in near real-time. That’s how they spotted the heart failure risk with pioglitazone-not in a trial, but after 10 years of real use across 190,000 patients. Real-world data also catches side effects that trials never see. A 2022 survey by the National Patient Advocate Foundation found that 63% of patients experienced side effects not listed in their drug’s official label. Nearly half of those were moderate to severe-fatigue, brain fog, nausea-that made daily life harder. Patients using apps like MyTherapy reported 27% more fatigue with immunotherapy than what trials recorded. Why? Because trials only asked about fatigue during office visits. Patients felt it worst at home, in the evenings, when no one was watching.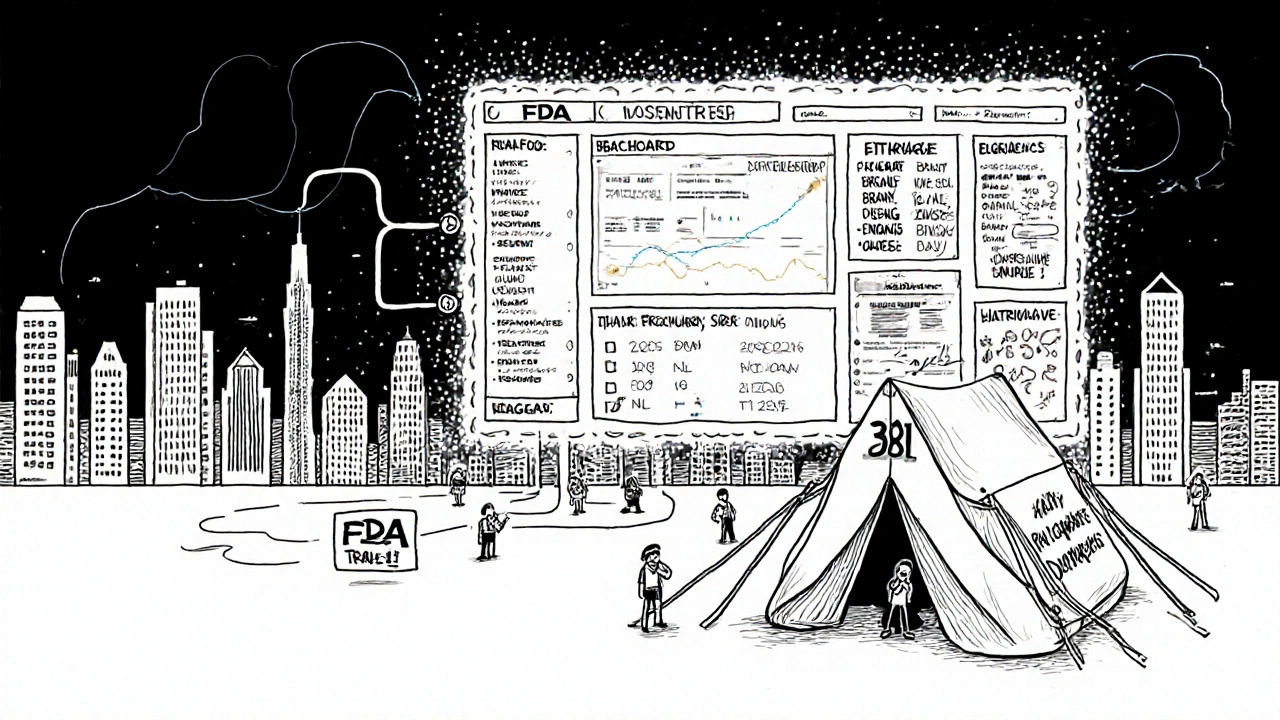
Why Both Systems Fail-And How They Complement Each Other
Clinical trials are great at proving cause and effect. If you give 500 people a drug and 10% get liver damage, and only 2% in the placebo group do, you can say the drug likely caused it. That’s hard to prove with real-world data, where people take other medications, have different diets, and live different lives. But real-world data is better at showing what happens when the drug leaves the lab. It finds rare side effects. It shows how side effects change over time. It reveals how side effects hit different groups-like older adults, people of color, or those with kidney disease-who were left out of trials. The problem? Real-world data is noisy. In 2018, a study suggested anticholinergic drugs caused dementia. But later analysis showed the real culprit was the underlying conditions-like depression or urinary problems-that led people to take those drugs in the first place. Without proper analysis, real-world data can point to fake dangers. That’s why the FDA now uses both. In 2022, 67% of new drug approvals included real-world evidence in their post-marketing safety plans. That’s up from 29% in 2017. Companies are even starting to collect real-world data during clinical trials. Pfizer, for example, now asks trial participants to use apps to track symptoms at home-not just during clinic visits.What This Means for You
If you’re prescribed a new drug, the label you get is based on clinical trials. But that label doesn’t tell the full story. Side effects listed there might be common ones-nausea, dizziness, headache. But what about the ones that only show up after six months? Or the ones that hit harder in people over 70? Or the ones that only appear when you’re stressed, sleeping poorly, or taking another medication? That’s where real-world data fills the gap. If you notice something strange-like unexplained fatigue, memory lapses, or mood swings-you’re not imagining it. You’re seeing what clinical trials couldn’t catch. And you’re not alone. On Reddit’s r/Pharmacy, 78% of pharmacists say the side effects they see in real life don’t match what’s in the trial data, especially with newer drugs like GLP-1 agonists for weight loss. Don’t wait for your doctor to ask. Track your own symptoms. Use a simple app or notebook. Note when they happen, how bad they are, and what else you’re taking. That data matters. It’s not just personal-it’s public. Every report you make helps improve safety for everyone.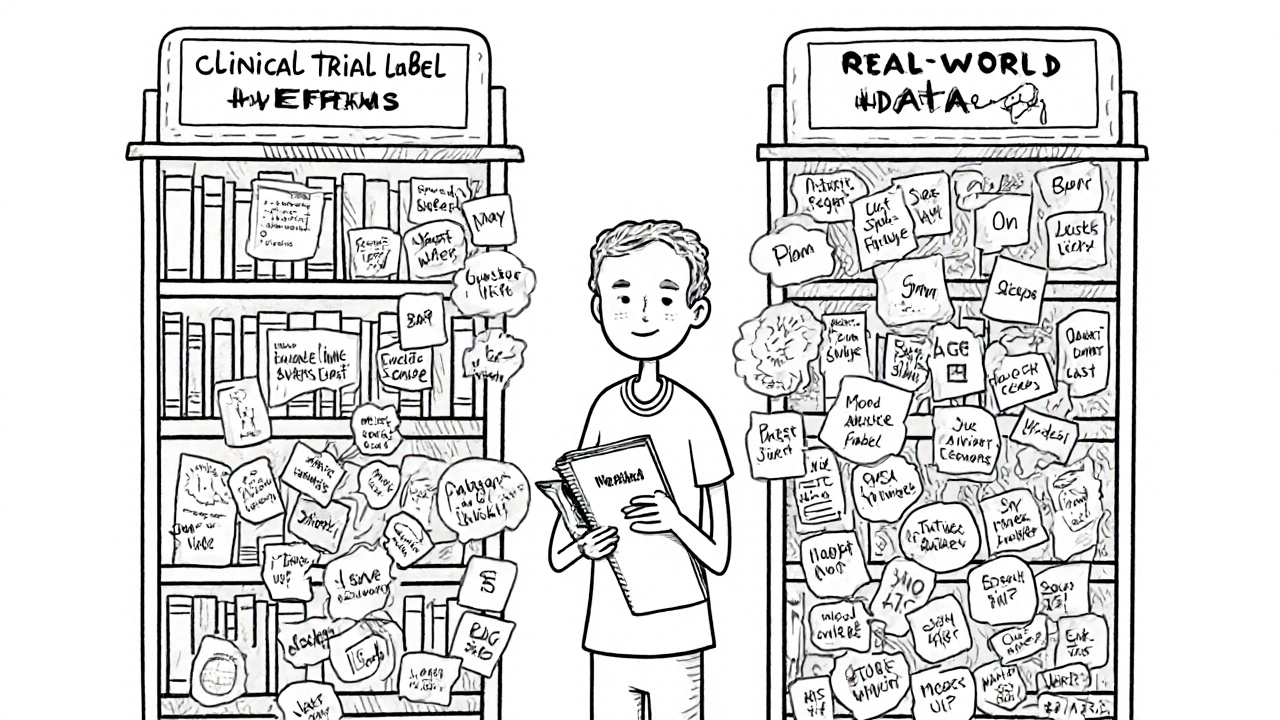
What’s Changing Right Now
The FDA’s 2023 Real-World Evidence Framework says every new drug application must now include a plan for monitoring side effects after launch. That’s huge. It means drug companies can’t just rely on trials anymore. They have to watch what happens in the real world. Technology is accelerating this. Apple’s Heart Study used smartwatches to track irregular heart rhythms in 419,000 people-larger than most clinical trials. Google Health’s AI analyzed 216 million clinical notes and found 23% more drug-side effect links than traditional methods. These aren’t science fiction. They’re tools being used right now. But there’s still a gap. Only 15% of U.S. medical schools teach real-world evidence analysis. Only 38% of doctors feel confident interpreting it. That means you might be the most informed person in the room. If your doctor says, “That side effect isn’t listed,” ask: “Was it seen in real-world data?”Bottom Line
Clinical trials tell you what a drug can do under perfect conditions. Real-world data tells you what it actually does when millions of people use it-flaws, quirks, and all. Neither is perfect. Together, they’re the best tool we have. Don’t trust one over the other. Trust both. And if you notice something unusual after starting a new medication-don’t ignore it. Document it. Report it. You’re not just protecting yourself. You’re helping improve medicine for everyone.Why are side effects in clinical trials different from real-world reports?
Clinical trials use small, carefully selected groups under strict conditions, so they only catch common or severe side effects that appear quickly. Real-world data comes from millions of diverse people using the drug daily, which reveals rare, delayed, or context-dependent side effects-like those triggered by stress, other medications, or lifestyle factors-that trials miss.
Can real-world data replace clinical trials for drug safety?
No. Clinical trials are still the gold standard for proving whether a drug causes a side effect because they control variables and use randomization. Real-world data can’t prove causation as clearly-it shows patterns and signals. But it’s essential for spotting rare or long-term risks that trials can’t detect due to small sample sizes and short durations.
How accurate is the FDA’s adverse event reporting system?
The FDA’s FAERS system receives over 2 million reports yearly, but experts estimate only 2-5% of actual side effects are reported. Many go unreported because doctors are too busy, patients don’t realize it’s important, or symptoms are mild. Still, when a pattern emerges across thousands of reports, it becomes a red flag for regulators to investigate further.
Why do some side effects only appear years after a drug is approved?
Clinical trials usually last months to a few years. But some side effects take much longer to develop-like certain cancers, heart damage, or neurological issues. Real-world data, collected over decades through electronic records and patient reports, is the only way to catch these delayed reactions. For example, the heart failure risk with pioglitazone wasn’t clear until 10 years of real-world use.
Should I stop taking my medication if I experience a side effect not listed on the label?
Never stop a prescribed medication without talking to your doctor. But if you notice a new or unusual symptom-especially if it’s persistent or worsening-document it and report it. Many side effects not on the label are rare or mild, but some can be serious. Your report helps regulators and researchers understand the full safety picture.
How can I report a side effect I experienced?
You can report directly to the FDA through MedWatch, their online portal for adverse event reporting. You can also ask your pharmacist or doctor to file a report on your behalf. Even if you’re unsure whether it’s related to the drug, report it. The FDA looks for patterns-so your single report could be part of a bigger picture that leads to safer use guidelines.


Comments
edgar popa
just started that new weight loss pill and my brain feels like mush. not on the label. but i’ve been napping at my desk. glad i’m not alone.
Eve Miller
It is profoundly irresponsible to suggest that anecdotal reports from unverified sources can supersede the rigorous, controlled methodology of clinical trials. The very foundation of evidence-based medicine is being eroded by this casual dismissal of scientific standards.
Chrisna Bronkhorst
clinical trials are a marketing tool disguised as science. 381 people? that’s a focus group. real world data is the only truth. 2 million faers reports and you’re still acting like it’s noise? you’re either paid by pharma or you’re stupid. pick one.
Amie Wilde
i’ve been tracking my fatigue since starting the GLP-1. it’s way worse than the trial said. my dr shrugged. so i reported it. if you’re feeling weird, don’t second-guess it. write it down. send it in.
Gary Hattis
as someone who’s lived in 7 countries, i’ve seen how drug safety plays out differently everywhere. in india, people just live with side effects. in germany, they report everything. here? we’re stuck in the middle. real-world data isn’t just useful-it’s a global justice issue. if your grandma’s not in the trial, her side effects still matter.
Esperanza Decor
why do we still treat clinical trials like gospel? they’re not. they’re a starting point. i’ve been in three trials. they don’t ask about sleep quality at 2am. they don’t ask if you cried because you forgot your kid’s name. those aren’t ‘side effects’-they’re life. and life isn’t controlled. we need to stop pretending it is.
Deepa Lakshminarasimhan
they’re hiding the real side effects. the ones that make you forget your own birthday. the ones that make your bones ache at night. you think faers is full? it’s not. they’re deleting reports. the same people who made the drug are the ones analyzing the data. you’re being watched. you’re being manipulated. don’t trust the label. don’t trust the doctor. trust your body. and burn your pill bottle.
Erica Cruz
so we’re celebrating patient anecdotes as science now? how cute. next you’ll be citing TikTok influencers as clinical reviewers. if your fatigue is ‘worse than the trial,’ maybe you’re just lazy. or maybe you’re one of the 98% of people who don’t read the label and then blame the drug for their poor lifestyle choices. real-world data doesn’t mean ‘my weird feeling.’ it means statistically significant signals across millions. and no, your nap schedule isn’t a dataset.