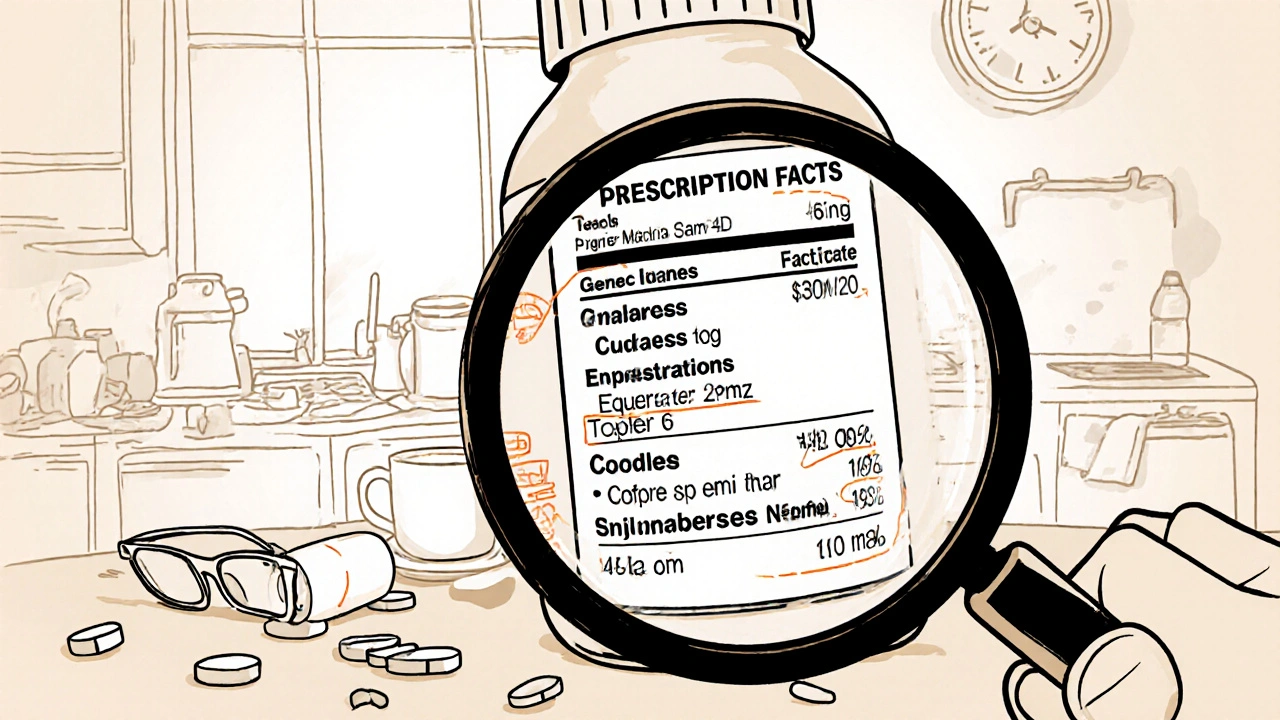
Every pill, injection, or inhaler you take comes with a label. But how many of you actually read it? Not just glance at it, but truly understand what it says? If you’ve ever taken medicine and wondered, Is this the right dose? or Why am I taking this? or even What happens if I take it with food? - you’re not alone. Millions of people struggle with drug labels every day. And the stakes? They’re life-or-death.
What’s Really on a Prescription Drug Label?
Prescription labels aren’t just stickers with a name and a number. They’re legal documents, regulated by the FDA, designed to guide healthcare providers. But they’re not built for patients. The full label, called the United States Prescribing Information (USPI), has 17 sections. Most of them are written in dense medical language meant for doctors and pharmacists. Here’s what you’ll actually see on the bottle or box:- Generic name - the active ingredient (e.g., metformin)
- Brand name - what the drug is sold as (e.g., Glucophage)
- Strength - how much medicine is in each unit (e.g., 500 mg per tablet)
- Form - tablet, capsule, liquid, patch
- Quantity - how many pills or units are in the bottle
- Manufacturer - who made it
- NDC number - a unique 10-digit code for tracking
- Expiration date - after this, the drug may not work as intended
- Storage instructions - Keep refrigerated, Store at room temperature
- Directions - how often and how much to take
- Pharmacy info - name, phone, address
- Patient name - your name, clearly printed
That’s the surface. But the real danger lies in what’s missing - or what’s buried.
The Hidden Danger: Why Labels Confuse Patients
A 2022 survey by the American Pharmacists Association found that 68% of patients had trouble understanding their prescription labels. And 41% admitted they’d taken their medicine wrong because of it. Why? Because labels are cluttered, inconsistent, and full of abbreviations. Take this common direction: "Take 1 tab PO q6h PRN". What does that mean? If you don’t know medical shorthand:- PO = by mouth
- q6h = every 6 hours
- PRN = as needed
That’s three potential points of confusion right there. The Institute for Safe Medication Practices says confusing abbreviations cause about 15% of all medication errors. And it’s not just abbreviations. Similar-sounding names trip people up - hydroxyzine vs. hydralazine, clonazepam vs. clonidine. One letter off, and you could be taking a completely different drug.
Older adults face even bigger hurdles. The Medicare Rights Center reported that 54% of seniors over 65 struggle with small print. For someone with poor eyesight or arthritis, reading a tiny label isn’t just hard - it’s dangerous. That’s why medication errors are 22% higher in this group.
Over-the-Counter Labels Are Different - and Simpler
If you’re buying pain relievers, allergy meds, or cold syrup off the shelf, you’re looking at a Drug Facts label. This is the FDA’s attempt to make things clearer for regular people. Here’s what’s on every OTC label:- Active ingredient - the medicine that works (e.g., acetaminophen)
- Purpose - what it does (e.g., pain reliever/fever reducer)
- Uses - what symptoms it treats (e.g., headache, fever, sore throat)
- Warnings - when NOT to use it (e.g., do not use if you have liver disease)
- Directions - how much and how often to take
- Inactive ingredients - fillers, dyes, flavorings
- Other information - storage, expiration
- Questions? Call... - manufacturer’s contact info
This format is standardized. It’s easier to scan. But even here, people get confused. A 2017 study by Nationwide Children’s Hospital found that parents often mix up dosing instructions - especially with liquid medicines. They use kitchen spoons instead of dosing cups. That’s a recipe for overdose.
What You Should Always Check - Five Critical Elements
Before you take any medicine, stop. Look. Confirm. These five things are non-negotiable:- Your name - Is it spelled right? Is it even your name?
- The drug name - Does it match what your doctor told you? If it’s a new pill, look it up.
- Dosage - Is it what your doctor prescribed? A 10 mg tablet isn’t the same as a 50 mg one.
- Directions - How many times a day? With food? On an empty stomach?
- Expiration date - If it’s past that date, don’t risk it.
These checks take 30 seconds. But they prevent hospital visits. The Cleveland Clinic says understanding your label can reduce unnecessary ER trips and hospital readmissions. That’s not just savings - it’s safety.
What’s Missing - And Why It Matters
Here’s the biggest gap: Why you’re taking this drug. Most labels don’t say. You get a pill for high blood pressure, but the label doesn’t tell you it’s for hypertension. You’re told to take it daily, but not why. A 2020 University of Florida study found that when labels included the indication - like "for high blood pressure" - medication errors dropped by 42%. Think about that. Just adding one line cuts nearly half the mistakes. Doctors and pharmacists know this. But the FDA’s official stance is that labels are for professionals, not patients. That’s why some pharmacies are stepping in. A 2022 survey by the National Community Pharmacists Association found that 63% of independent pharmacies now add a simple line like "For high cholesterol" to the label. Chain pharmacies? Only 41% do it.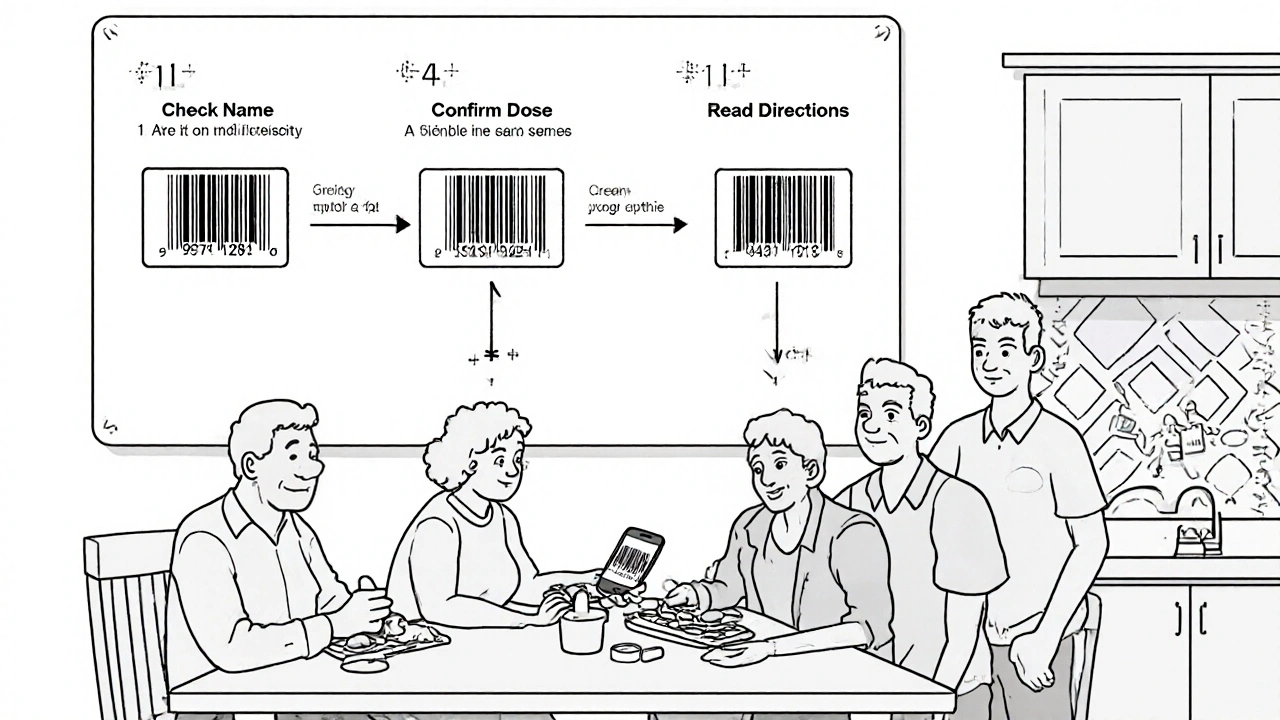
What’s Coming: Better Labels Are on the Way
The FDA is finally listening. Their 2023-2027 strategic plan includes a major push for clearer patient labeling. They’re developing something called Patient Medication Information (PMI) - a one-page, standardized document that will replace the confusing, multi-page prescribing guides. Here’s what PMI will include:- What the drug is for (in plain language)
- How to take it (with clear timing)
- What side effects to watch for
- When to call your doctor
- What to avoid (food, alcohol, other meds)
- How to store it
First versions are expected by 2026. And they’ll be mandatory for high-risk drugs first - things like blood thinners, insulin, and chemotherapy agents.
They’re also rolling out Instructions for Use (IFU) - step-by-step guides with pictures for complex meds like inhalers, injectables, or infusions. Imagine a label that shows you how to use your EpiPen with drawings. That’s the future.
What You Can Do Today
You don’t have to wait for better labels. Here’s what you can do right now:- Ask your pharmacist - They’re trained to explain labels. Say: "Can you walk me through this? I want to make sure I’m taking it right."
- Use a pill organizer - Especially if you take multiple meds. It reduces confusion.
- Take a photo - Snap a picture of the label when you get your prescription. Compare it later.
- Use apps - Apps like Medisafe or MyTherapy let you scan barcodes and get plain-language explanations.
- Don’t be shy - If something looks off, ask. Even if you’ve taken the drug before. Formulations change. Doses change. Always double-check.
And if you’re helping an older relative? Sit with them. Read the label out loud. Point to each part. Make sure they know why they’re taking it.
Final Thought: Your Label Is Your Lifeline
Medication errors cause about 7,000 deaths in the U.S. every year. Most of them are preventable. The label isn’t just paper. It’s your protection. It’s your warning system. It’s the one thing standing between you and a dangerous mistake.Don’t treat it like a nuisance. Treat it like your life depends on it - because it does.
What’s the difference between generic and brand name on a drug label?
The generic name is the active ingredient - the chemical that makes the drug work (e.g., ibuprofen). The brand name is what the company calls it for marketing (e.g., Advil). Both have the same active ingredient, so they work the same way. Generic versions are cheaper because they don’t include the cost of branding or advertising. Always check the generic name to avoid accidentally doubling up on the same drug.
Why do some drug labels have a black box warning?
A black box warning is the strongest safety alert the FDA requires. It’s printed in a black border around the text to highlight serious, potentially life-threatening risks - like liver failure, suicidal thoughts, or severe allergic reactions. It doesn’t mean you can’t take the drug, but it means you need to be closely monitored by your doctor. Never ignore a black box warning.
Can I take medicine after the expiration date?
Most medicines are still safe for a year or two past their expiration date, but they may lose potency. For critical drugs like insulin, epinephrine, or antibiotics, don’t risk it. Expired insulin won’t control your blood sugar. Expired epinephrine might not save your life during an allergic reaction. When in doubt, throw it out and get a new prescription.
What should I do if my label doesn’t match what my doctor told me?
Stop. Don’t take it. Call your pharmacy immediately. Mistakes happen - a wrong dose, the wrong drug, a misread script. Pharmacists are trained to catch these. If they say it’s correct, ask them to call your doctor to confirm. Never guess. A mismatch could be deadly.
Are there apps that help me understand my medication labels?
Yes. Apps like Medisafe, MyTherapy, and Drugs.com let you scan your pill’s barcode or enter the name to get plain-language explanations. They’ll tell you what the drug is for, how to take it, possible side effects, and interactions with other meds or food. Some even send reminders. These are especially helpful if you’re on multiple medications or have trouble reading small print.


Comments
Scott Macfadyen
Just got my new script and stared at the label like it was ancient hieroglyphs. PO? Q6H? PRN? I thought I was taking medicine, not decoding a spy novel. Someone explain this to me like I’m five.
Denise Cauchon
OMG YES. I once took my grandma’s blood pressure med because I thought it looked like mine. She ended up in the ER. I’m not even kidding. These labels are a trap. 🤯
Andrea Johnston
It’s not just poor labeling-it’s systemic negligence. The FDA prioritizes corporate liability over patient comprehension. They’d rather bury you in 17-section USPI documents than admit that 70% of the population reads at a 6th-grade level. This isn’t incompetence. It’s institutional contempt.
Alex Czartoryski
Bro, I’ve been taking metformin for 8 years and I still don’t know if I’m supposed to take it before or after tacos. The pharmacy just shrugs and says ‘follow the arrow.’ I think the arrow points to ‘hope for the best.’
Victoria Malloy
My mom’s 72 and she uses a magnifying glass just to read the tiny print. I started printing out her labels in 24pt font and laminating them. It’s dumb, but it saved her from a mix-up last month. Small fixes matter.
malik recoba
i always take a pic of my label when i get it. then i compare it when i pick it up again. sometimes they give me the wrong thing and i catch it before i take it. just a little habit but it saved me twice.
Gizela Cardoso
My pharmacist actually wrote ‘for cholesterol’ on my label last time. I cried. No one’s ever done that before. It’s such a small thing, but it made me feel seen. Maybe change is starting.
Chloe Sevigny
One might argue that the current labeling paradigm is a perfect exemplar of technocratic paternalism: the assumption that laypersons are incapable of processing complex medical information, and thus must be subjected to obfuscation as a form of ‘protection.’ The irony? The obfuscation itself is the primary vector of harm. The FDA’s PMI initiative, while long overdue, remains a half-measure unless it mandates plain-language indications as a non-negotiable component. Anything less is performative reform.
Sarbjit Singh
Bro, use Medisafe app! Scan your pill, it tells you in simple words what it's for, side effects, even warns if you're mixing with other meds. I taught my uncle in Punjab how to use it. He’s 70, no smartphone before. Now he never misses a dose. 💪
Angela J
Have you noticed how all the big pharma labels look exactly the same? Coincidence? Or are they trying to make us confused so we don’t ask questions? I swear, the black box warnings are getting bigger every year… and the instructions are getting smaller. They want you scared, but too lost to fight back.
Sameer Tawde
Read the label. Ask questions. Use apps. Don’t guess. It’s that simple. Your life isn’t a gamble.