Every pill you take could be fake. It’s not science fiction - it’s happening right now. In 2023, the WHO estimated that 1 in 10 medicines in low- and middle-income countries are counterfeit. Even in places with strict regulations, fake drugs slip through. The difference between a life-saving treatment and a deadly placebo often comes down to two things: a lot number and a serial code.
What Lot Numbers and Serial Codes Actually Do
A lot number is like a birth certificate for a batch of medicine. It tells you when, where, and how that group of pills or vials was made. If the same machine, same ingredients, and same shift produced 10,000 bottles of blood pressure medicine, they all get the same lot number. It’s not about the individual bottle - it’s about the group. Serial codes are different. They’re unique to each single unit. Think of them like a fingerprint for each pill bottle. No two are the same. One bottle might have serial code A7B9X2, the next B8C1Y4. That level of detail matters when you need to find one bad unit out of millions. Together, these numbers form the backbone of track-and-trace systems. They let manufacturers, pharmacies, and regulators follow a drug from the factory floor all the way to your medicine cabinet. If something goes wrong - contamination, mislabeling, or outright fraud - you don’t have to pull every single bottle off the shelf. You just pull the ones with that one bad lot number or serial code.Why This Matters for Counterfeit Drugs
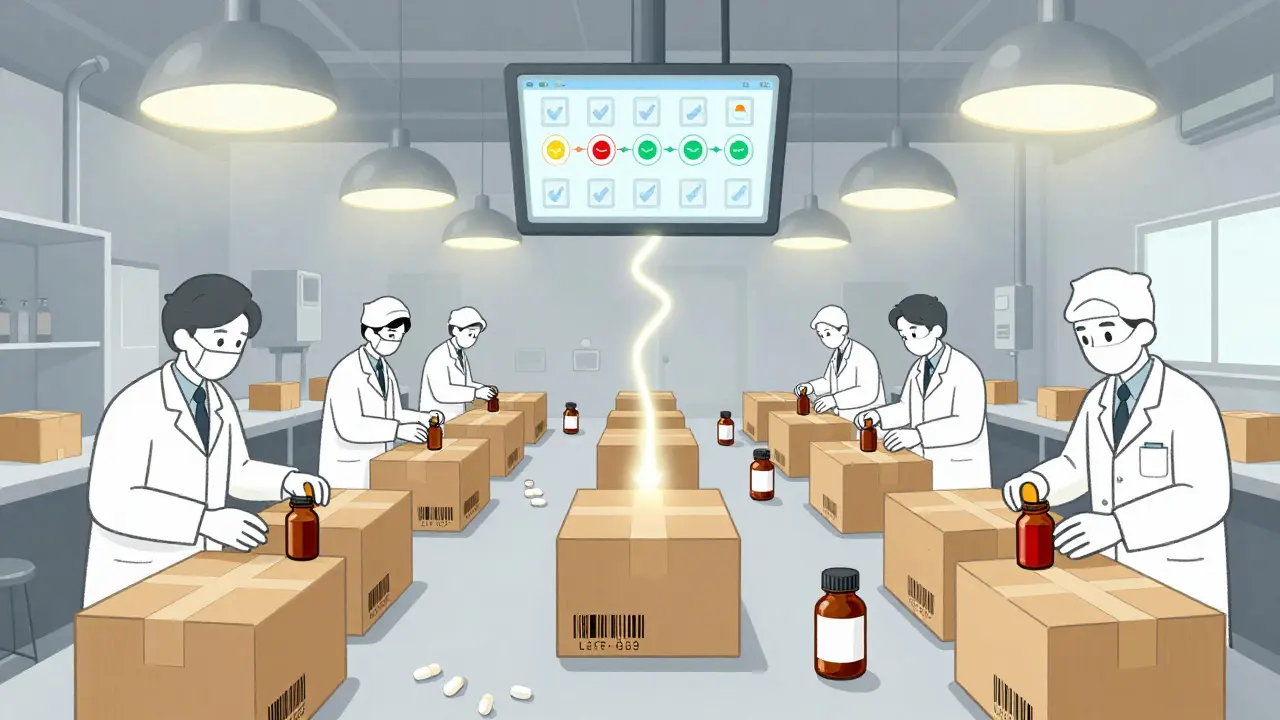
Counterfeiters don’t care about safety. They’re not making medicine. They’re making money. Fake insulin, fake cancer drugs, fake antibiotics - these aren’t harmless. They kill. In 2022, a fake version of a popular blood thinner was found in 14 countries. Over 200 people died before the recall even started. Without lot and serial tracking, those fake drugs could have stayed on shelves for months. Pharmacies wouldn’t know which batches were affected. Patients wouldn’t know if their pills were real. But with track-and-trace, it’s different. In 2023, a U.S. pharmacy chain used serial code scanning to flag 87 bottles of fake metformin in a single day. The system showed those bottles came from a distributor that wasn’t authorized. The entire shipment was quarantined. No one got sick. No recall. Just one bad batch, isolated and removed. That’s the power of serial tracking. Lot numbers catch big problems - like a contaminated batch of raw material. Serial codes catch the sneaky stuff - the one bottle that was swapped in at a warehouse, the one that was repackaged with fake labels.How the System Works in Real Life
It starts at the factory. Each batch gets a lot number printed on the box. Each bottle gets a unique serial code printed as a QR code or barcode. That code links to a secure database with details: production date, expiration date, location, and who shipped it. When the medicine arrives at a pharmacy, the pharmacist scans the barcode. The system checks:- Is this lot number authorized by the manufacturer?
- Is this serial code already in the system? (If yes, it’s been reported stolen or duplicated.)
- Is the expiration date still valid?
- Has this item been flagged in any recall?

Regulations Made This Necessary
This isn’t optional. It’s law. In the U.S., the Drug Supply Chain Security Act (DSCSA) requires all prescription drugs to have serialized identifiers by 2023. That means every bottle, every box, every vial must have a unique code. The same rules are rolling out in the EU, Canada, Australia, and parts of Asia. The FDA started issuing warning letters to companies that didn’t comply. In 2023 alone, 147 pharmaceutical firms got flagged for incomplete or inconsistent tracking. Some were forced to halt shipments. Others paid millions in fines. Why? Because the old system didn’t work. In 2012, a batch of contaminated heparin killed 81 people. The manufacturer didn’t know where the bad ingredient came from. They couldn’t trace it. Today, that kind of failure is nearly impossible.What Happens When the System Fails
Track-and-trace isn’t magic. It only works if people use it right. In 2023, a hospital in Melbourne reported a spike in adverse reactions to a common antibiotic. The lot number matched a batch from a trusted supplier. But when investigators dug deeper, they found the pharmacy had been manually entering serial codes - not scanning them. Someone had typed in a fake code. The system trusted the input. No one checked. The fix? Mandatory scanning. No more typing. No exceptions. Within two weeks, the error rate dropped from 12% to 0.3%. Another failure case: a small online pharmacy in Eastern Europe sold fake cancer drugs with copied serial codes. They were using codes from real bottles - but reusing them. The system didn’t catch it because it only checked if the code existed, not if it had been used before. Now, systems are updating to flag duplicate serials in real time. The lesson? Technology only helps if you enforce the rules.


Comments
Neela Sharma
Every time I see a pill bottle now I stare at that barcode like it's a sacred text. In India we don't always have access to real meds but when we do that serial code is the only thing standing between us and disaster. No fancy tech needed just a phone and a database. Simple but life saving.
Michael Burgess
This is the kind of stuff that actually matters. I work in a clinic and we scan every script now. Used to be a hassle now it's second nature. One time we caught a fake antiviral because the QR code led to a dead link. No one got hurt because the system worked. Tech isn't magic but when it's used right? It's everything.
Tiffany Channell
Let's be real the entire pharmaceutical industry is a pyramid scheme built on fear and patents. These 'track-and-trace' systems are just PR tools to make you feel safe while they keep jacking up prices. The real problem isn't counterfeit drugs it's corporate greed.
Joy F
The ontological weight of serialization in pharmacopeia is staggering. We are no longer merely consuming substances we are participating in a distributed ledger of biological sovereignty. Each QR code is a micro-narrative of industrial discipline and epistemic control. The very notion of 'lot' implies a Cartesian fracture between the individual and the collective. The serial code? That is the Cartesian point of medical identity. We are not patients we are data points in a post-pharmaceutical phenomenology.
Haley Parizo
You think this is about safety? It's about control. Big Pharma wants you dependent on their scanning apps their databases their certifications. They don't want you to trust your own instincts. They want you to need permission from a machine to know if your medicine is real. That's not progress that's submission. And don't even get me started on blockchain - it's just a digital altar for corporate idols.
Angela Fisher
EVERYTHING IS A LIE. The FDA? Controlled by the same people who make the fake drugs. The lot numbers? Fake too. They put the real serial codes in the cloud but the ones on the bottle? Scanned by AI that's been hacked by the Chinese. I know a guy who works at a warehouse and he says they reuse codes from expired pills and the system doesn't catch it because the algorithm is trained on corrupted data. And the apps? They're spyware. They track your heartbeat when you scan. They know when you're sick. They know when you're dying. And they're selling it to insurers. You think you're safe? You're a lab rat with a barcode on your chest.
Vincent Sunio
While the intent behind serialization is laudable, the implementation remains fraught with systemic inefficiencies. The DSCSA mandates unique identifiers, yet compliance is uneven across tiers of the supply chain. Moreover, the absence of standardized cryptographic authentication renders many codes vulnerable to spoofing. One must question the epistemological reliability of a system predicated on human-operated scanning protocols - a paradigm that reintroduces the very human error it purports to eliminate.
erica yabut
Of course the system works in the U.S. - because we have standards. In places like India or Nigeria? They're still using handwritten labels and hope. This isn't about medicine - it's about civilization. If you can't even track a pill properly, what hope do you have for anything else? You don't get to be a modern country if you're still playing with fake barcodes and wishful thinking.
Kerry Howarth
Good piece. The Melbourne case is a perfect example of why we need to stop letting humans type in codes. Scanners aren't perfect but they're way better than tired nurses typing A7B9X2 when it's actually A7B9X3. Simple fix. Big impact.
Liam Tanner
Just want to say thank you for writing this. I'm a nurse and I used to roll my eyes at the barcode scanners. Now I see them as the quiet heroes of the ER. One scan stopped a deadly mix-up last month. No fanfare. No headlines. Just a green light. That's enough.
Hank Pannell
It's fascinating how this mirrors broader societal shifts. We've moved from trusting institutions to trusting algorithms. The lot number becomes a proxy for truth. The serial code becomes proof of authenticity. But what happens when the algorithm is wrong? Or when the database is corrupted? We've outsourced our epistemic responsibility to machines. And yet - we still need them. The tension between faith in technology and fear of its failure is the real story here.
Angela Goree
USA has the BEST system. Period. Other countries? They can't even spell 'pharmaceutical' right. We spent billions on this. We have the best tech. The best laws. The best enforcement. And you know what? We don't need your help. We don't need your 'apps' or your 'blockchain' - we've already fixed it. You just need to catch up. America made this work. Again. Because we're better.
Shanahan Crowell
Look - I used to think this was all corporate BS. Then my mom got fake chemo. She didn't die. But she spent six months in the hospital because the serial code didn't match. That barcode? It saved her life. Don't overthink it. Just scan it. Trust the system. It's not perfect - but it's the best thing we've got.
Shruti Badhwar
As a pharmacist in Mumbai I can confirm this system is not perfect but it is necessary. We have cases where counterfeiters copy serial codes from expired batches. The system flags the code as valid - but not if it's been used twice. We now manually cross-check with manufacturer logs weekly. It's extra work but lives are at stake. This isn't about compliance - it's about duty.