Diabetes Medication: Types, Risks, and What Actually Works
When you have diabetes medication, drugs used to manage high blood sugar in people with type 1 or type 2 diabetes. Also known as antihyperglycemic agents, these aren’t just pills you take—they’re tools that change how your body handles sugar, and getting them wrong can be dangerous. Whether you’re on insulin, a hormone injection needed by type 1 diabetics and some type 2 patients to move glucose into cells, or metformin, the first-line oral drug that reduces liver sugar production and improves insulin sensitivity, each choice carries trade-offs. Insulin can cause life-threatening lows if dosed wrong. Metformin might give you stomach issues but rarely causes weight gain. And some newer drugs, like GLP-1 agonists, help you lose weight while lowering blood sugar—but they’re expensive and not for everyone.
What most people don’t realize is that diabetes medication doesn’t work in isolation. It interacts with other drugs you might be taking. For example, combining insulin with beta-blockers, medicines for high blood pressure or heart conditions can hide the warning signs of low blood sugar, like shaking or a fast heartbeat. You might not feel your blood sugar dropping until it’s too late. Or if you’re on NSAIDs for arthritis, those can mess with kidney function, which is already at risk if you’ve had diabetes for years. Even something as simple as skipping meals or drinking alcohol can turn a stable dose into an emergency. That’s why understanding your meds isn’t just about reading the label—it’s about knowing how they fit into your whole life.
There’s no one-size-fits-all fix. What works for your neighbor might make you sick. Some people do fine on metformin alone. Others need insulin, GLP-1 drugs, SGLT2 inhibitors, or even older options like sulfonylureas. The key is matching the drug to your body, your habits, and your risks—not just your A1C number. Below, you’ll find real-world breakdowns of how these drugs compare, what side effects actually happen in daily life, and how to spot the red flags most doctors don’t have time to explain.
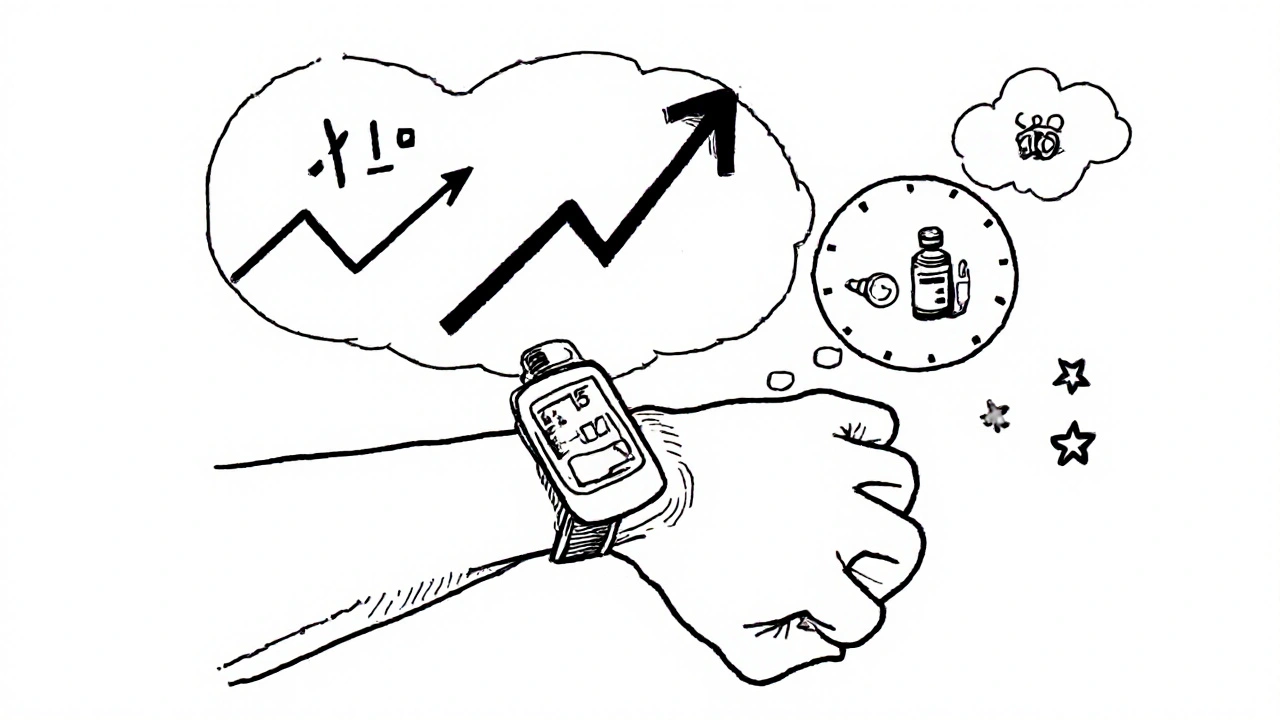
How to Adjust Diabetes Medication Doses Using CGM Trend Arrows to Prevent Low and High Blood Sugar
Learn how to use CGM trend arrows to adjust insulin and other diabetes medications in real time, preventing dangerous lows and highs with science-backed protocols. Reduce hypoglycemia, improve time-in-range, and take control of your diabetes management.
read more