CGM Trend Arrow Dose Calculator
Adjust Insulin Dose Based on Trend Arrows
Calculate the correct insulin adjustment using the Endocrine Society guidelines based on your current glucose level, trend arrow, and correction factor.
When your blood sugar is dropping fast and you’re about to eat, should you take your full insulin dose? What if your glucose is climbing even though you took your usual correction? These aren’t hypotheticals-they’re daily decisions for people using CGM systems. The real power of continuous glucose monitoring isn’t just seeing your number. It’s knowing where it’s headed. And that changes everything about how you take your diabetes meds.
Why Trend Arrows Matter More Than Your Current Number
A single glucose reading tells you where you are right now. But it doesn’t tell you what’s coming. That’s where trend arrows come in. On Dexcom, Abbott Libre, and other modern CGMs, you’ll see arrows pointing up, down, or flat. These aren’t decorative. They’re signals. A double-up arrow means your glucose is rising more than 2 mg/dL per minute. A double-down means it’s falling just as fast. That’s not a coincidence-it’s your body telling you what’s happening right now, and what’s likely to happen in the next 15 to 30 minutes. Traditional blood glucose meters give you snapshots. CGMs give you a movie. And when you’re on insulin, that movie is your best tool for avoiding crashes and spikes before they happen. A 2017 study in Diabetes Technology & Therapeutics showed people using trend arrows had 28% fewer low blood sugar events and spent 17% more time in target range. That’s not a small gain. That’s life-changing.The Endocrine Society’s Proven Dose Adjustment Rules
In 2017, the Endocrine Society released clear, science-backed guidelines for adjusting insulin based on trend arrows. These aren’t suggestions. They’re protocols backed by clinical data and used by diabetes centers across the U.S. and Australia. The key? They use specific unit adjustments, not vague percentages. Here’s how it works for adults with a correction factor of 1:50 (meaning 1 unit of insulin lowers glucose by 50 mg/dL):- Double-up arrow (fast rising): Add 1.2 units to your pre-meal or correction dose
- Single-up arrow (rising): Add 0.8 units
- Flat arrow (stable): No adjustment needed
- Single-down arrow (falling): Subtract 0.8 units
- Double-down arrow (fast falling): Subtract 1.2 units
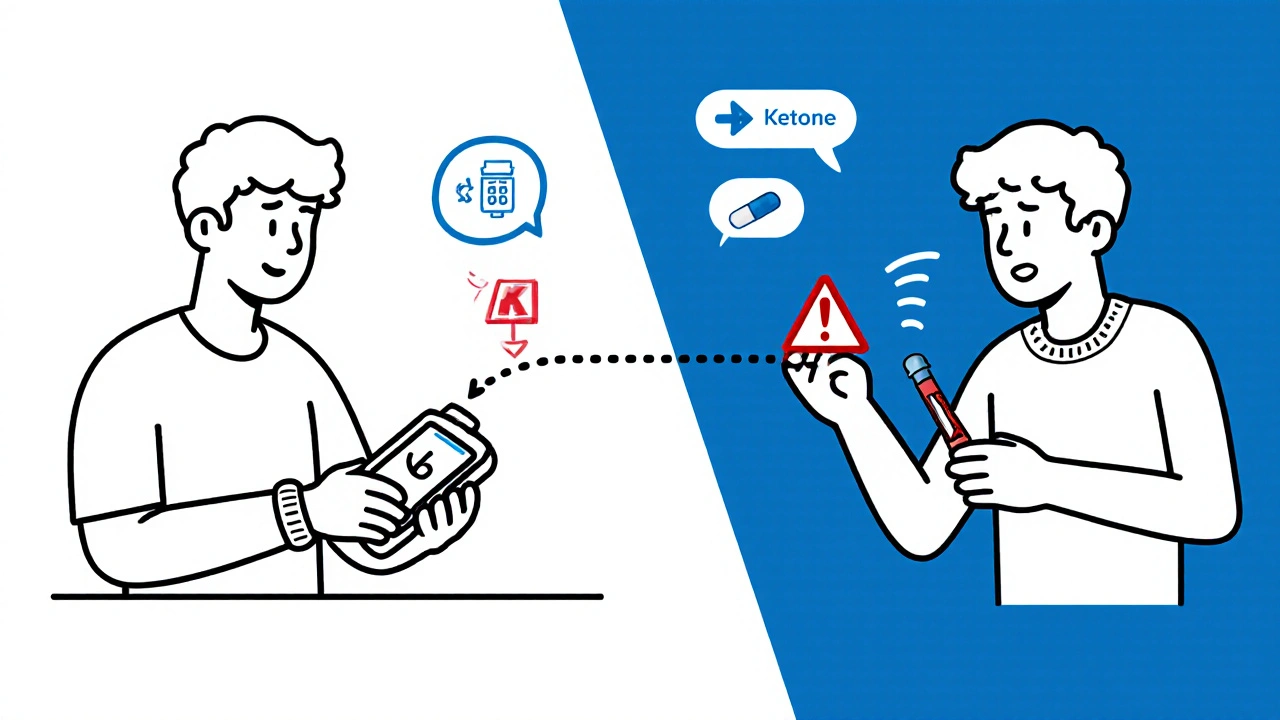
What About Non-Insulin Medications?
Most people think CGM adjustments only apply to insulin. That’s outdated. The 2024 ADA/EASD consensus report now recommends dose adjustments for other drugs too-especially SGLT2 inhibitors like dapagliflozin or empagliflozin. These drugs lower blood sugar by making your kidneys flush out glucose. But if your CGM shows persistent euglycemic ketosis (glucose under 180 mg/dL with ketones above 0.6 mmol/L), you’re at risk for diabetic ketoacidosis even without high sugar. In those cases, reducing your SGLT2 inhibitor dose-sometimes by half-is the safest move. This isn’t theoretical. Emergency rooms in Melbourne and Sydney have seen cases where patients on SGLT2 inhibitors developed ketoacidosis because their glucose stayed normal, but their ketones climbed unnoticed. CGM trend patterns, combined with ketone testing, are now part of standard safety protocols.
Common Mistakes and How to Avoid Them
Using trend arrows sounds simple. But people mess it up-often in the same ways.- Ignoring insulin-on-board (IOB): One user on Diabetes Daily doubled their insulin for a double-up arrow… but forgot they’d taken a correction 90 minutes earlier. Result? A 45 mg/dL low. Always check your pump or app for active insulin before adjusting.
- Adjusting during sensor lag: If you just ate, exercised, or your sensor just started, the trend arrow might be wrong. Wait 15 minutes and check again.
- Over-correcting for fast drops: If your glucose is falling fast but you’re not on insulin, you don’t need to eat. The arrow is showing a natural drop, not a crash. Eat only if you’re below 70 mg/dL.
- Not verifying with a fingerstick: If the arrow is pointing down and you feel shaky, do a fingerstick. Sensors can be off during rapid changes. Trust your body, not just the screen.
How to Get Started-Step by Step
If you’re new to this, here’s how to begin:- Know your correction factor: Ask your endocrinologist. It’s usually calculated as 1800 divided by your total daily insulin dose (for rapid-acting). If you take 30 units a day, your CF is 1:60.
- Download the official Endocrine Society reference card: Dexcom’s provider portal has printable versions. Keep one on your fridge or phone.
- Track for 7 days: Write down your glucose, trend arrow, insulin dose, and what you ate. Look for patterns. Do you always spike after lunch? Do you drop after walks?
- Start small: Only adjust one dose per day. Maybe your breakfast bolus. Once you’re confident, move to corrections.
- Check in with your diabetes educator: Even 15 minutes every two weeks helps. They can spot errors you miss.
What’s Changing in 2025?
The game is evolving. Dexcom G7 and Abbott Libre 3 now have faster sensors and better trend accuracy. The Endocrine Society is updating its guidelines to include these devices. Newer apps like DAFNE+ (cleared by the FDA in 2023) now automate the math-enter your glucose and trend, and the app tells you exactly how many units to give. In trials, user error dropped by 62%. AI is coming too. Verily’s Onduo platform used machine learning to predict glucose changes 45 minutes ahead-beyond what arrows can show. In a 2022 NEJM pilot, it cut hypoglycemic events by 38%. These tools won’t replace your judgment. But they’ll make your decisions faster and safer.When to Call Your Doctor
You don’t have to figure this out alone. If you’re:- Having frequent lows or highs despite following the rules
- Feeling confused about your trend arrows
- On SGLT2 inhibitors and seeing ketones on your CGM
- Using an insulin pump or hybrid closed-loop system
Real Results, Real People
On Reddit’s r/typeonegriit, a user named InsulinWizard42 cut their weekly hypoglycemic events from 3.2 to 0.7 after using the Endocrine Society rules. “It took the guesswork out,” they wrote. “I didn’t have to calculate percentages anymore.” In Melbourne, a mother of a 10-year-old with Type 1 diabetes started using the pediatric adjustment table after her son had two nighttime lows in one week. She now reduces his bedtime insulin when she sees a double-down arrow at 11 p.m. No more panic. No more juice boxes at 2 a.m. This isn’t about being perfect. It’s about being proactive. CGM isn’t just a monitor. It’s your early warning system. And when you use it right-with the right rules-you don’t just manage diabetes. You take back control.Can I use trend arrows if I’m not on insulin?
Yes. While most adjustments focus on insulin, trend arrows also help guide non-insulin medications. For example, if you’re on an SGLT2 inhibitor and your CGM shows persistent euglycemic ketosis (glucose under 180 mg/dL with ketones above 0.6 mmol/L), your doctor may advise reducing your dose to prevent ketoacidosis. Trend arrows help you spot these patterns early.
What if my CGM shows a double-down arrow but I feel fine?
Don’t assume you’re safe. CGM sensors can lag during rapid drops. Check your blood sugar with a fingerstick. If it’s below 70 mg/dL, treat it. If it’s above 70 but falling fast, reduce your next insulin dose by 0.8-1.2 units (depending on your correction factor). Even if you feel okay, a fast fall can lead to a crash in 15-30 minutes.
Do I need to adjust for every trend arrow?
No. Only adjust if the trend is consistent and you’re not in the middle of insulin action. For example, if you just took a correction 45 minutes ago and your glucose is still rising, that’s likely the insulin working. Wait. If you’re about to eat and your glucose is rising fast, that’s when you adjust. Use your judgment. If unsure, stick to your standard dose.
Are trend arrows the same on all CGMs?
Not exactly. Dexcom defines a double-up arrow as a rise over 2 mg/dL per minute. Abbott Libre 3 uses a threshold of 3 mg/dL per minute. That means the same glucose change might show as a single-up on Libre but a double-up on Dexcom. Always check your device’s manual. The Endocrine Society guidelines were based on Dexcom, but the principles apply. Adjust your numbers based on your device’s definition.
How long does it take to get good at using trend arrows?
Most people get comfortable in 2-4 weeks with consistent use. The first week is usually the hardest-you’re learning to read patterns and trust the data. Keep a log. Review it weekly. After a month, you’ll start seeing which trends mean what for your body. You don’t need to be perfect. You just need to be consistent.
Can my doctor automate these adjustments?
Yes. Apps like DAFNE+ (FDA-cleared in 2023) now automate the Endocrine Society calculations using your CGM data. They factor in your correction factor, insulin-on-board, and trend arrows to suggest exact dose changes. In clinical trials, these apps reduced dosing errors by 62%. Talk to your provider about whether one is right for you.


Comments
Alexis Hernandez
Man, I used to think my CGM was just a fancy pedometer for blood sugar. Then I started paying attention to those arrows. One time I saw a double-down after lunch and held off on my insulin-saved myself from a 52 low at 3 a.m. No juice boxes, no panic. Just trust the trend.
It’s like your body’s texting you. You just gotta learn the slang.
brajagopal debbarma
So let me get this straight. You’re telling me we’re supposed to trust a machine that sometimes thinks my toe is a glucose sensor? I once had a double-up arrow while I was in the shower. The sensor was wet. I didn’t adjust. My sugar went to 320. The machine lied. Again.
Stop treating gadgets like oracles.
Carly Smith
Oh wow look at this 12-page essay on how to not die from your own insulin
Did you forget to mention that half the people using this don’t even know what a correction factor is?
Also your ‘pediatric adjustments’ are useless if your kid’s school won’t let them check their CGM during math class
And why are you ignoring the fact that most people can’t afford these devices in the first place?
Just saying. You’re preaching to the choir with a gold-plated pump.
Kurt Stallings
Endocrine Society guidelines? Cute.
Real clinicians use pharmacokinetic modeling and real-time adaptive algorithms.
This is like teaching someone to ride a bike with a training wheel made of duct tape.
And don’t get me started on SGLT2 inhibitors. You’re still treating symptoms, not pathophysiology.
CGM arrows are just noisy signals in a chaotic system.
But sure, keep adjusting by 0.8 units. That’ll fix everything.
Angie Creed
You say ‘take back control’ like it’s some spiritual awakening.
But what if your control is just a series of calculated risks wrapped in a false sense of security?
What if the real problem isn’t the dose adjustment-it’s the fact that we’ve turned a chronic illness into a spreadsheet?
Are we healing people-or just optimizing their suffering?
And why does every post about diabetes end with a ‘you can do it!’ pep talk?
Some of us aren’t looking for motivation. We’re looking for mercy.
Michael Ferguson
I’ve been doing this for 27 years and I’ve never once followed any of these rules-and I’ve never had a single serious hypo or hyper event.
You people are overcomplicating the hell out of this. My doctor gave me a number. I take it. I eat when I’m hungry. I move when I feel like it. That’s it.
And I’ve been stable since 1997.
So why are we treating this like a math competition?
Some of us don’t need algorithms. We need peace.
And honestly? If your CGM is making you anxious, maybe you need to unplug for a week and just breathe.
I’m not saying you’re wrong. I’m saying you’re wasting your life over numbers that don’t even matter in the grand scheme.
My HbA1c is 5.9. I’m 54. I run marathons. I don’t even own a pump.
What’s your excuse again?
Patrick Klepek
Okay but the part about SGLT2 inhibitors and euglycemic ketoacidosis? That’s terrifying and also totally under-discussed.
I had a friend in Dublin who ended up in the ER with ketones at 1.8 and glucose at 150. They thought she was fine because her sugar wasn’t high.
Turns out her CGM was showing a flat arrow but her ketone meter was screaming.
So yeah-this isn’t just about insulin. It’s about listening to your whole body, not just one number.
Also, props to the author for mentioning sensor lag. That’s the silent killer.
Caden Little
Y’all need to stop overthinking this 😊
Start with one meal. Pick breakfast. Track your arrow + dose + food for 3 days.
Then adjust your insulin by 0.8 if you see a single-up.
That’s it.
No spreadsheets. No panic.
Just one small change.
Then next week, try corrections.
You don’t need to be perfect-you just need to be consistent.
And if you’re unsure? Text your diabetes educator. They’re there to help.
I’ve helped 30+ people do this in the last year. Everyone says the same thing: ‘Why didn’t I start sooner?’
You got this 💪
Sebastian Brice
Look, I get it. Trend arrows feel like magic.
But sometimes they’re just… noise.
I used to adjust every time I saw a double-down. Ended up eating snacks I didn’t need. Got fat. Got frustrated.
Then I realized: if I’m not on insulin, and I’m not feeling low, and my fingerstick says 85? I just wait.
My body knows what it’s doing.
Not every arrow needs a response.
Some days, the best thing you can do is nothing.
And that’s okay.
It’s not weakness. It’s wisdom.
Jim Aondongu
This whole thing is just western medicine overcomplicating a simple thing
Back home in Nigeria we just eat balanced meals and check sugar once a day
If it's high we skip rice
If it's low we drink juice
No arrows no apps no formulas
And we live longer than most of you with your fancy pumps
Maybe the problem isn't the dose
Maybe the problem is you're too attached to your gadgets
Stop listening to machines and start listening to your hunger
Michael Schaller
I was skeptical at first. But after two weeks of tracking my arrows and meals, I noticed something: my afternoon crashes always happened after pasta.
So I started reducing my lunch bolus by 0.6 units on pasta days.
Now I don’t need a snack at 4 p.m.
It’s not magic. It’s pattern recognition.
And honestly? The most powerful thing here isn’t the numbers.
It’s the fact that you’re paying attention.
That’s what changes everything.