Hatch-Waxman Act: How Generic Drugs Got Their Start and What It Means for You
When you pick up a generic pill at the pharmacy and pay a fraction of what the brand-name version costs, you’re seeing the result of the Hatch-Waxman Act, a 1984 U.S. law that balanced drug innovation with affordable access by creating a faster path for generic drugs to enter the market. Also known as the Drug Price Competition and Patent Term Restoration Act, it’s the reason you can buy generic versions of drugs like lisinopril, metformin, or sertraline for under $5.
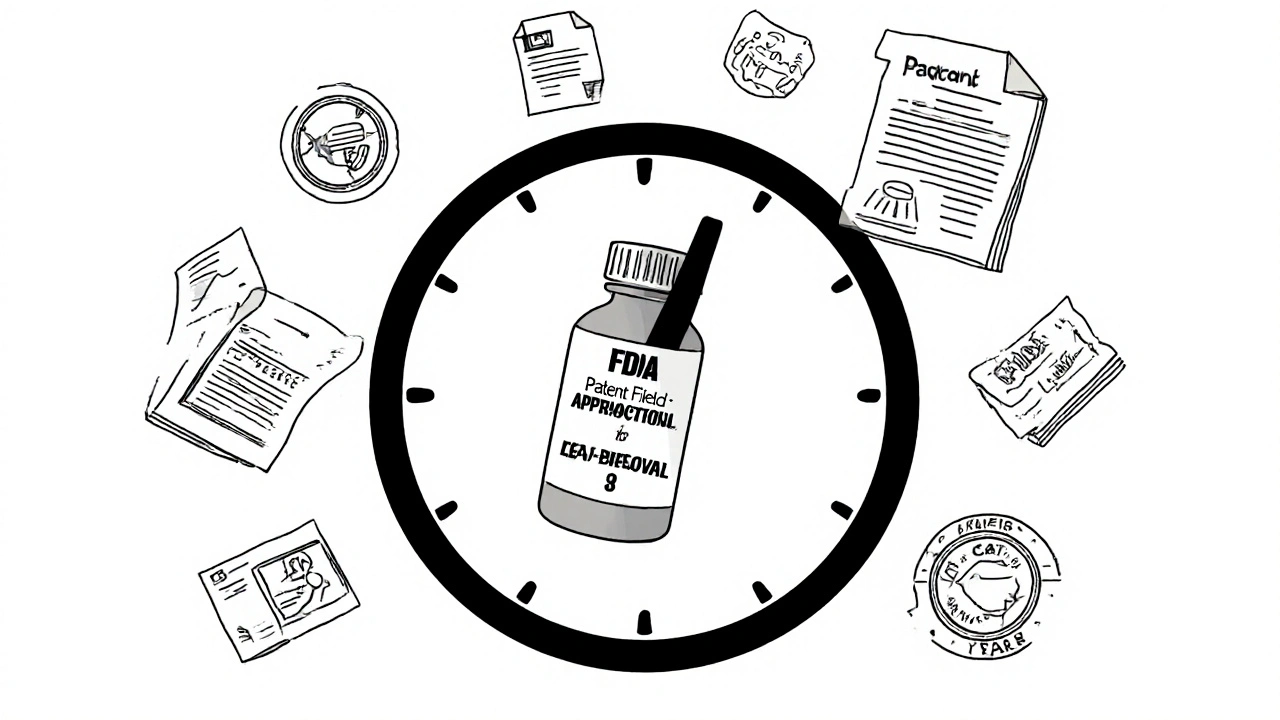
This law didn’t just make generics legal—it gave them a clear roadmap. Before 1984, companies had to run full clinical trials to prove a generic drug worked, even if the brand-name version had already been proven safe. That made generics too expensive to develop. The Hatch-Waxman Act let generic makers file an Abbreviated New Drug Application (ANDA) with the FDA, the U.S. agency responsible for approving drugs and ensuring their safety and effectiveness. Also known as Food and Drug Administration, it only needed to show their version was bioequivalent—not reinvent the wheel. At the same time, it gave brand-name drugmakers up to five extra years of patent protection to make up for time lost during FDA review. That trade-off kept innovation alive while opening the door to competition.
That balance still shapes how drugs are priced and prescribed today. If you’ve ever wondered why your doctor switches you from a brand-name drug to a generic, or why some generics cost more than others depending on your state, it’s because of the Hatch-Waxman Act’s ripple effects. It’s also why companies like those making isotretinoin, a powerful acne drug with strict safety rules under the iPLEDGE program or baclofen, a muscle relaxant used for spasticity still have patents that delay generics—because the law lets them. And when generics finally do arrive, prices often drop by 80% or more.
But it’s not just about cost. The Hatch-Waxman Act changed how we think about drug safety. It forced the FDA to build systems like REMS, Risk Evaluation and Mitigation Strategies, which are safety programs required for high-risk drugs like isotretinoin to protect patients even after generics enter the market. It also set the stage for today’s debates around drug pricing, patent evergreening, and why some medications still have no affordable alternatives years after their patent expires.
What you’ll find below are real-world examples of how this law touches your life: from the labels on your pills to the cost of your prescriptions, from how the FDA handles safety alerts to why some drugs take forever to go generic. Whether you’re managing asthma during pregnancy, adjusting insulin doses, or trying to afford your thyroid meds, the Hatch-Waxman Act is quietly in the background—making some drugs cheaper, some harder to access, and all of it more understandable once you know how it works.
How Brand Manufacturers Produce Their Own Generic Versions
Brand manufacturers create their own generic versions to keep market share after patents expire. These authorized generics are identical to the brand drug but sold at lower prices - with complex impacts on cost, competition, and patient trust.
read moreWhen Do Drug Patents Expire? Understanding the 20-Year Term and Real-World Timelines
Drug patents are legally 20 years long, but most expire in 7-12 years due to R&D delays. Learn how patent extensions, regulatory exclusivity, and legal strategies affect when generics become available.
read more