Opioid-Alcohol Risk Calculator
How This Tool Works
Based on scientific data from the article: 20mg oxycodone causes 28% breathing reduction. Adding alcohol to reach 0.1% BAC increases this by 19%. The combined effect is multiplicative, not additive.
Risk Assessment
Combined breathing reduction: 0%
Increased risk of respiratory depression: 0%
When you take an opioid for pain - whether it’s oxycodone, hydrocodone, or fentanyl - your body is already under stress. These drugs slow your breathing, dull your senses, and can make you drowsy. Now add alcohol. Just one drink. Maybe two. It doesn’t take much. And suddenly, what was a manageable side effect becomes a life-threatening emergency.
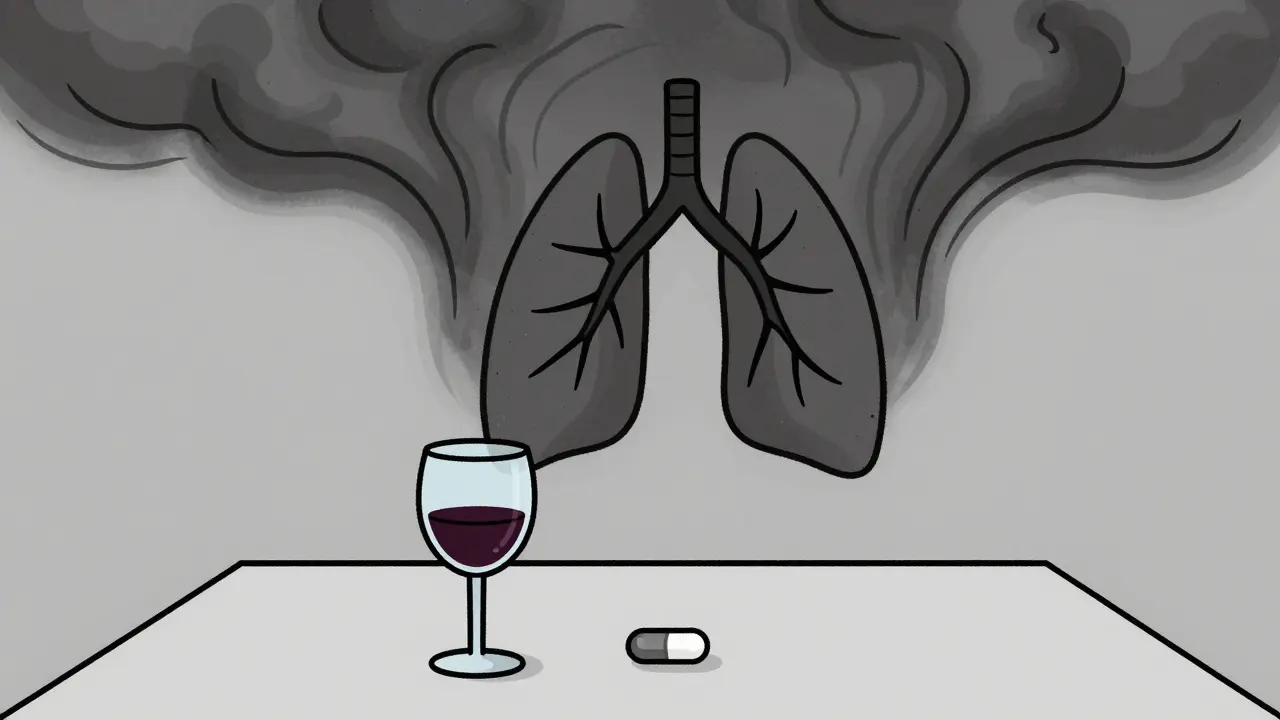
Why Mixing Alcohol and Opioids Is a Silent Killer
Alcohol and opioids don’t just add up - they multiply. Both are central nervous system depressants. That means they slow down your brain’s control over breathing, heart rate, and consciousness. When taken together, they don’t just work side by side. They team up. And that teamwork can shut down your lungs before you even realize something’s wrong.
The U.S. Food and Drug Administration (FDA) put out a black-box warning in 2016 - the strongest possible alert - telling doctors and patients: do not mix alcohol with opioids. Why? Because the data didn’t lie. In 2022 alone, over 107,000 people in the U.S. died from drug overdoses. More than 80% of those involved multiple substances. And alcohol was in nearly half of all opioid-related deaths.
It’s not just about heavy drinking. Even a single glass of wine or a beer can be enough. A 2017 study showed that taking 20mg of oxycodone reduced breathing by 28%. Add alcohol to reach a blood alcohol level of just 0.1% - the legal limit for driving in most places - and breathing dropped another 19%. That’s not a small risk. That’s a tipping point.
Who’s Most at Risk?
You might think this only happens to people with addiction. It doesn’t. Many people who mix alcohol and opioids are taking them exactly as prescribed. They have chronic pain. They take their opioid pills. They have a glass of wine with dinner. Or a few beers after work. They don’t see it as dangerous. But the science says otherwise.
Older adults are especially vulnerable. Their bodies process alcohol and opioids slower. Their lungs are less resilient. A 2017 study found that older patients on opioids had more frequent and longer pauses in breathing when they drank - even small amounts.
People on methadone for opioid use disorder are also at high risk. Research shows they’re 4.6 times more likely to die from an overdose if they drink alcohol. That’s not a typo. That’s more than four times the danger.
And it’s not just prescription opioids. Fentanyl, whether prescribed or bought illegally, is especially deadly when mixed with alcohol. From 2010 to 2019, alcohol was involved in 9% of fentanyl deaths. By 2019, that number jumped to 17%. Heroin deaths showed similar spikes. Meanwhile, deaths from prescription opioids with alcohol stayed steady at 10-15% - still far too high.
The Science Behind the Danger
Here’s how it works inside your body:
- Opioids bind to receptors in your brainstem that control breathing.
- Alcohol enhances the effect of those same receptors.
- Together, they silence the signal that tells your body to breathe.
- Your breathing becomes shallow, then stops.
- Without oxygen, your brain and organs begin to shut down.
- You may fall into a deep sleep - and never wake up.
Post-mortem studies show that alcohol lowers the amount of opioid needed to cause death. For example, researchers found that 30% of people who died from buprenorphine overdoses also had alcohol in their system. That means the same dose of medication that might be safe alone becomes deadly with even a small amount of alcohol.
The World Health Organization calls respiratory depression the #1 cause of opioid death. And alcohol is one of the most common triggers.

It’s Not Just Alcohol - The Triple Threat
Many people don’t realize that alcohol isn’t the only dangerous mix. Benzodiazepines - like Xanax or Valium - are often taken with opioids and alcohol. In 2021, nearly 14% of opioid overdose deaths involved benzodiazepines. Add alcohol to that mix, and the risk skyrockets.
Doctors now screen patients for alcohol use disorder before prescribing opioids. Why? Because people with alcohol use disorder are 3.2 times more likely to overdose on opioids. It’s not about willpower. It’s about biology. The brain chemistry changes. The tolerance shifts. The margin for error disappears.
What’s Being Done?
Health agencies are trying to catch up. In January 2023, the Substance Abuse and Mental Health Services Administration (SAMHSA) launched the “Don’t Mix” campaign with $15 million in funding. Their goal? Reduce alcohol-opioid overdose deaths by 10% by 2025.
The FDA now requires all opioid manufacturers to include clear warnings about alcohol in patient education materials. Pharmacies must hand out these warnings when you pick up your prescription. But warnings alone aren’t enough.
In Massachusetts, naloxone - the overdose reversal drug - was used in 23% of cases in 2022 where alcohol was involved. That’s a lifeline. But naloxone doesn’t fix the problem. It just buys time. The real fix is stopping the mix before it starts.
What Should You Do?
If you’re taking opioids - even once a day - don’t drink alcohol. Not even a sip. Not even on special occasions. The risk isn’t worth it.
If you’re helping someone who takes opioids, learn the signs of overdose:
- Slow or stopped breathing
- Blue or gray lips and fingernails
- Unresponsiveness - shaking or shouting won’t wake them
- Slow or erratic heartbeat
Keep naloxone on hand. It’s available without a prescription in most places. Know how to use it. Call 911 immediately - even after giving naloxone. The effects of alcohol and opioids can return after naloxone wears off.
If you’re struggling with alcohol use and opioids, talk to your doctor. There are treatment options. There’s help. You don’t have to do this alone.
The Bottom Line
Mixing alcohol and opioids isn’t a gamble. It’s a guaranteed risk. The numbers don’t lie. The science doesn’t lie. The deaths don’t lie.
You don’t need to be an addict. You don’t need to be using drugs recreationally. You just need to be human. And humans forget - until it’s too late.
One drink. One pill. One night. That’s all it takes.


Comments
Anthony Capunong
Y’all in the US act like this is some new revelation. In Nigeria, we’ve been seeing this shit for years - people popping oxycodone like candy and chugging gin like it’s water. No one’s surprised when they don’t wake up. We don’t need a federal warning. We need better access to rehab, not more pamphlets.
And stop acting like it’s only ‘prescribed’ users. Half the people mixing this shit are just trying to numb their trauma. You can’t scare people with data if you don’t give them a way out.
Ayodeji Williams
Bro… I just had a beer and took my tramadol for my back. 😅 Not a big deal right? I’m fine. I’ve done it for years. You people are drama queens. 🤷♂️
Also, why is everyone so scared of death? It’s gonna happen anyway. Might as well go out with a buzz and no pain. 🍻💊
Emma Addison Thomas
Thank you for writing this with such clarity. I work in palliative care in London, and I’ve seen too many elderly patients - all compliant, all kind - slip away because they thought ‘just one glass’ wouldn’t hurt.
It’s heartbreaking how easily we normalize risk when it’s wrapped in routine. A wine with dinner. A pill after yoga. No one imagines it ends in silence.
I wish these warnings came with more compassion, not just fear.
Christine Joy Chicano
The pharmacokinetics here are chillingly elegant in their lethality. Opioids bind mu-opioid receptors in the pre-Bötzinger complex - the very neural pacemaker for respiration. Alcohol potentiates GABA-A receptor activity, which hyperpolarizes those same neurons, further suppressing respiratory drive. The synergy isn’t additive; it’s multiplicative, and the margin for error collapses into a single-digit milliliter of ethanol.
And yet, we treat this like a moral failing. It’s neurobiology. It’s physiology. It’s not ‘stupid’ - it’s tragically predictable. We need harm reduction infrastructure, not shaming.
Also, why are we still calling it ‘alcohol-opioid’ deaths? That implies two separate agents. In reality, it’s a single, synergistic toxin. We need new terminology. New framing. New urgency.
Adam Gainski
As a pharmacist, I’ve handed out those FDA warning sheets for years. Most patients glance at them and say ‘I know, I know.’
But here’s what actually works: when I sit down with them and say, ‘Let me show you what happens in your body.’ I pull up the study data - the 28% drop in breathing, then the extra 19% with alcohol. I show them the graphs. I ask, ‘Would you drive with your brakes half-broken?’
That’s when it clicks. Not because I yelled. Because I helped them see it.
Education > fearmongering. Always.
Anastasia Novak
Oh my god. I just read this and I’m crying. Not because I’m dramatic (okay maybe I am) but because I lost my cousin last year. He was 42. Took his hydrocodone for his back. Had one glass of Pinot with his pasta. Went to bed. Never woke up.
His wife found him with the wine glass still in his hand. Like he was just… tired.
They didn’t even know he was on opioids. He never told anyone. Thought he was being ‘responsible.’
Now I tell everyone. EVERYONE. Don’t mix. Don’t even think about it. One drink. One pill. One night. And you’re gone. I’m not okay. I’m not okay at all.
Elen Pihlap
I’m so mad. I hate this. I hate that people think it’s safe. I hate that doctors don’t tell you. I hate that you can just buy this stuff. I hate it. I hate it. I hate it.
Sai Ganesh
In India, we don’t have easy access to opioids, so most people don’t even know this risk. But when they do - like those with cancer pain - alcohol is often used to ‘enhance’ the effect. No one warns them. No one explains.
What we need is community health workers, not FDA pamphlets. People trust their neighbors more than government warnings.
And yes - this is deadly. But the real tragedy is how little we do about it in places where pain is invisible and help is far away.
Paul Mason
Look, I’ve been a GP for 20 years. I’ve seen this a hundred times. The worst part? It’s not the addicts. It’s the nice old lady who takes her pain meds and has a glass of sherry every night. She’s got no idea she’s playing Russian roulette.
And here’s the kicker - most of them don’t even drink daily. Just weekends. Just holidays. Just ‘one time.’
That’s the killer. The ‘just once.’
Don’t be that person. Just don’t.
Aparna karwande
This is why America is collapsing. You let people turn medicine into a party. You let them mix poison like it’s a cocktail. You have laws for everything - but not for common sense.
My grandmother in Delhi would never dream of mixing painkillers with alcohol. She’d rather suffer than risk her life. But here? You turn death into a meme.
Stop pretending this is about ‘education.’ It’s about culture. And your culture is broken.