Switching from brand-name drugs to generic medications isn’t just a way to save money-it’s a smart, science-backed choice backed by decades of real-world use and strict federal oversight. If you’ve ever hesitated because you thought generics were "inferior" or "less effective," you’re not alone. But the truth? Generics work the same way, deliver the same results, and are held to the exact same standards as their expensive brand-name cousins.
They’re Not Cheaper Because They’re Weaker
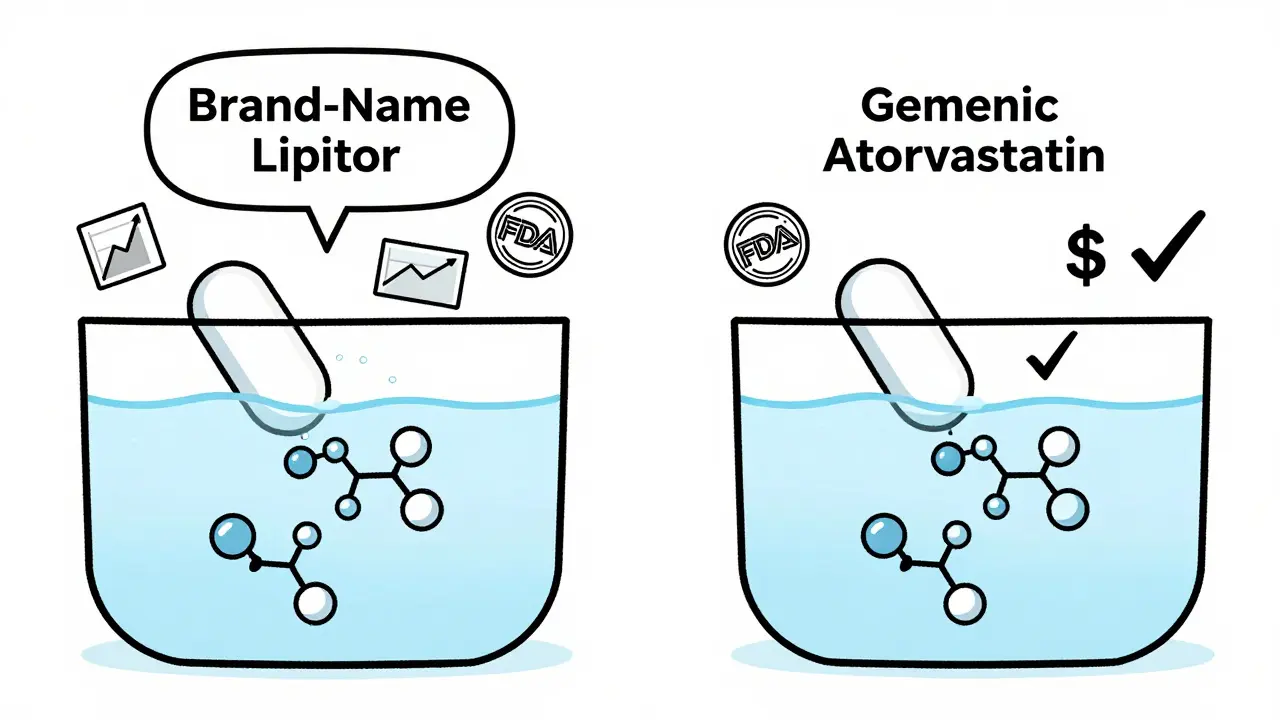
Generic drugs contain the same active ingredients, in the same strength, and in the same form as brand-name drugs. That means if your prescription is for 10 mg of lisinopril, the generic version has exactly 10 mg of lisinopril. No more, no less. The U.S. Food and Drug Administration (FDA) requires every generic drug to prove it delivers the same amount of medicine into your bloodstream at the same rate as the brand-name version. This is called bioequivalence, and it’s not a suggestion-it’s a legal requirement.The FDA doesn’t let generics skip testing. They run pharmacokinetic studies using blood samples from volunteers to compare how quickly and completely the drug is absorbed. The acceptable range? Between 80% and 125% of the brand-name drug’s performance. That’s a tight window. If a generic falls outside that range, it’s rejected. No exceptions.
What’s different? The color, shape, or flavor. Those are inactive ingredients-fillers, dyes, or coatings-that don’t affect how the drug works. A blue pill today might be white tomorrow, but the medicine inside? Identical. Many patients panic when the pill changes appearance, but that’s just a change in manufacturer, not quality.
Cost Savings That Actually Matter
Here’s where the numbers get real. Generic drugs cost, on average, 80% to 85% less than brand-name versions. That’s not a small discount. That’s life-changing.Take Lipitor, the cholesterol drug. When the brand-name version was still on the market, it cost around $130 a month. The generic, atorvastatin? As low as $4 at major pharmacies. That’s $1,500 a year saved. For someone on a fixed income, that’s groceries, rent, or heat.
Warfarin, a blood thinner, used to cost over $300 a month as Coumadin. The generic? Around $4. Fexofenadine (Allegra) dropped from $30 to $10. Metformin, the most common diabetes drug, went from $300 for Glucophage to $4 a month. These aren’t hypotheticals-they’re daily realities for millions.
Over the past decade, generic drugs saved the U.S. healthcare system more than $1.6 trillion. That’s not a guess-it’s from the Association for Accessible Medicines, using verified data from IMS Health. Every week, generics save the system $3 billion. That money stays in patients’ pockets, reduces insurance premiums, and keeps public programs like Medicare from collapsing under cost.
Same Results, Lower Risk of Skipping Doses
Cost isn’t just about what you pay at the pharmacy-it’s about whether you can afford to take your medicine every day.A 2023 study in Research in Social and Administrative Pharmacy looked at 5,000 patients and found that those taking generics were 68% less likely to skip doses because of cost. That’s huge. Skipping pills because you can’t afford them leads to hospitalizations, complications, and higher long-term costs. One diabetes patient on PatientsLikeMe wrote: "Metformin generics cost me $4/month versus $300 for Glucophage-this keeps me adherent to my treatment." That’s not an anecdote. That’s the difference between health and crisis.
Studies on heart medications show the same thing. A 2022 study in the Journal of the American Heart Association followed 186,000 patients on generic versus brand-name drugs for high blood pressure and heart failure. No difference in outcomes. No higher risk of heart attack or stroke. Just the same results at a fraction of the price.

Doctors and Regulators Are on Your Side
You might think this is just a pharmacy trick. It’s not. The American Medical Association explicitly recommends prescribing generics whenever possible. The FDA’s former director, Dr. Janet Woodcock, said: "Generic drugs undergo rigorous review to ensure they are as safe and effective as brand-name drugs."Even specialists who are cautious about certain drugs admit the evidence is strong. Dr. James Grogan, a neurologist at Mayo Clinic, noted that while a few antiepileptic drugs may need closer monitoring, "most generics are equivalent." The FDA’s own data shows adverse event reports for generics are proportional to their usage-meaning they’re not causing more side effects. They’re just being used far more often.
Hospitals and pharmacies have been switching to generics for years. 99% of hospitals and 98% of retail pharmacies prioritize generics when medically appropriate. Insurance companies push them too-copays for generics are typically $1 to $10, while brand-name drugs can cost $25 to $75. Some plans won’t cover brand-name drugs at all unless you prove the generic doesn’t work for you.
What About "Narrow Therapeutic Index" Drugs?
You’ve probably heard the warning: "Some drugs can’t be switched to generics because they’re too sensitive." That’s true for a very small group-drugs like warfarin, levothyroxine, and some seizure medications. These have a narrow therapeutic index, meaning small changes in blood levels can matter.But here’s the catch: the FDA still requires these generics to meet the same 80-125% bioequivalence standard. The agency doesn’t treat them differently. In fact, the FDA’s "Orange Book," which lists all approved generic drugs and their therapeutic equivalence ratings, clearly marks which ones are interchangeable.
Some doctors may still prefer brand-name for these drugs out of habit or caution, but that’s not based on evidence. A 2023 review in the Journal of Managed Care & Specialty Pharmacy found no clinical difference in outcomes between generic and brand-name versions of these drugs in real-world settings. If your doctor says you can’t switch, ask: "Is this based on data, or just tradition?"

How to Switch Without Stress
Switching is simple. You don’t need a new prescription. When your refill comes up, your pharmacist can legally substitute a generic unless your doctor wrote "dispense as written" or "no substitution."Here’s how to make it smooth:
- Check your prescription label. If it says "brand necessary," ask your doctor if they’re open to generics.
- Ask your pharmacist: "Is there a generic version?" They’re trained to know.
- Don’t panic if the pill looks different. Call your doctor or pharmacist if you’re unsure-it’s not dangerous, but peace of mind matters.
- Use the FDA’s Orange Book online to verify therapeutic equivalence. It’s free and updated monthly.
Most people switch without any issue. A Kaiser Permanente survey in late 2023 found 87% of members were satisfied with generics. The top reason? Affordability. The bottom line? No drop in effectiveness.
The Bigger Picture: Why This Matters
This isn’t just about your wallet. It’s about the entire healthcare system. When people can afford their meds, fewer end up in the ER. Fewer get sicker. Fewer need surgeries or long-term care. Generics keep people out of hospitals.The Congressional Budget Office estimates that if generic use keeps growing, the U.S. could save another $1.2 trillion over the next decade. That’s money that could fund research, expand access, or lower premiums for everyone.
And it’s not slowing down. Biosimilars-generic versions of complex biologic drugs like Humira and Enbrel-are now approved and rolling out. They’re expected to save Medicare $50 billion a year by 2030. The FDA is speeding up approvals. More manufacturers are entering the market. Prices keep falling.
Brand-name drug prices are still rising at over 5% a year. Generics? Only 1.8%. The trend is clear: generics are the future of affordable, effective care.
Are generic medications as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict safety and quality standards as brand-name drugs. They’re made in the same type of facilities, inspected just as often, and held to identical manufacturing rules. Adverse event reports for generics are proportional to how often they’re used-meaning they’re not causing more side effects than brand-name drugs.
Why do generic pills look different?
The difference in color, shape, or size is due to inactive ingredients like dyes or fillers, which don’t affect how the medicine works. These are changed to avoid trademark issues with the brand-name version. The active ingredient-the part that treats your condition-is identical.
Can I switch to generics for any medication?
Almost all medications have generic versions, especially common ones like blood pressure, cholesterol, diabetes, and antidepressants. A few drugs with very narrow therapeutic windows (like warfarin or levothyroxine) may require closer monitoring, but even those generics are proven safe and effective. Always check with your doctor or pharmacist if you’re unsure.
Will my insurance cover generics?
Yes, and they usually pay much less. Most insurance plans have tiered formularies where generics are in the lowest cost tier-often $1 to $10 per prescription. Brand-name drugs can cost $25 to $75 or more. Some plans won’t cover brand-name drugs at all unless you get prior authorization.
Do generics take longer to work?
No. The FDA requires generics to be bioequivalent, meaning they enter your bloodstream at the same rate and to the same extent as the brand-name drug. If you feel a difference, it’s likely psychological or due to other factors-not the medication itself.
What to Do Next
If you’re on a brand-name drug and paying more than $20 a month, ask your pharmacist: "Is there a generic?" It takes 30 seconds. If you’re on a chronic condition-high blood pressure, diabetes, cholesterol, depression-switching could save you hundreds, maybe thousands, a year. And you won’t lose anything in effectiveness.Don’t let appearance, myths, or outdated fears stop you. The science is clear. The savings are real. And the people who benefit the most? The ones who just ask the question.


Comments
Meghan Hammack
OMG I switched my blood pressure med to generic last year and my copay dropped from $45 to $3. I thought I’d feel weird or weak, but nope-I’m more energetic now because I’m not stressing over bills. This post made me cry happy tears.
RAJAT KD
Generics are not inferior. They are mathematically equivalent. The FDA bioequivalence standard is 80–125% AUC and Cmax-statistically indistinguishable in clinical outcomes. Stop believing marketing.
Angela Stanton
Let’s be real-pharma’s whole business model is built on patent cliffs and FUD. 🤡 Generic manufacturers don’t spend $2B on ads telling you your pill looks different. They just make the damn drug. And yes, I’ve seen the FDA Orange Book. It’s all there.
Drew Pearlman
I used to be skeptical too-until my dad had a stroke and we couldn’t afford his meds. We switched him to generic clopidogrel and he’s been stable for 3 years. Same pill, same results. The real tragedy isn’t the pill color-it’s that people still think generics are risky. That’s corporate propaganda working. Don’t let fear cost you your health.
Chris Kauwe
Let’s not pretend this is about science. This is about economic nationalism. The U.S. government has been subsidizing generic manufacturing since the 1980s to break Big Pharma’s monopoly. It’s not about patient care-it’s about control. We import 80% of our API from China and India. That’s not freedom. That’s dependency dressed up as savings.
Pooja Kumari
I just want to say… I’ve been on generic metformin for 7 years now. The first time I got a different-looking pill, I panicked. I cried. I thought my body would reject it. I called my doctor three times. But then I read the label again. The active ingredient was the same. And I realized… I’d been afraid of a color. Not the medicine. Not the science. Just… a shade of blue. That’s when I knew I’d been manipulated. And I’m still healing from that fear. Thank you for this post. I needed to hear this.
Matthew Maxwell
It is a moral failing to refuse generics when they are available. The cost differential is not a coincidence-it is a consequence of profit-driven medicine. To choose brand over generic when financially feasible is to prioritize vanity over virtue. Your insurance company knows this. Your doctor knows this. You should too.
Ian Long
I get why people are nervous. I used to be too. But I sat down with my pharmacist and asked him to walk me through the FDA’s bioequivalence data. He showed me the studies. The graphs. The confidence intervals. It wasn’t magic. It was math. And math doesn’t lie. If you’re still scared, ask for the data. Don’t ask for reassurance. Ask for evidence.
Catherine Scutt
I hate generics. They make me feel like I’m on welfare. Like I’m not worthy of the real stuff. And yeah, I know it’s dumb. But I still do it. My Lipitor was $130. The generic was $4. I paid the $130 anyway. Don’t judge me.
Darren McGuff
As a pharmacist in rural England, I’ve seen this play out for decades. Patients cry when their brand changes. Then they thank me two weeks later when they can afford groceries again. The science is rock-solid. The fear? That’s all marketing. You’re not getting a lesser drug-you’re getting the same drug, without the branding tax.
Alicia Hasö
You are not alone if you’ve been scared. But here’s the truth: your body doesn’t care what color the pill is. Your heart doesn’t care if it’s called Lipitor or atorvastatin. Your bank account? It cares a LOT. Switching isn’t a compromise-it’s a win. And you deserve to win. You’ve earned this peace of mind. Go ahead. Ask your pharmacist. You’ve got this.
Aron Veldhuizen
Wait-you’re telling me the FDA approves generics based on 80–125% bioequivalence? That’s a 45% variance. That’s not equivalence. That’s a range. If I took 80% of my insulin dose, I’d die. So why is this acceptable? This isn’t science-it’s bureaucratic convenience. And now you’re telling me to trust it? No thanks.
Heather Wilson
Studies show 68% fewer skipped doses? That’s not because generics are better. It’s because people are desperate. When you’re choosing between insulin and rent, you don’t care about bioequivalence-you care about survival. This post is just guilt-tripping people into accepting systemic failure as normal.
Jeffrey Hu
Actually, the 80–125% bioequivalence range is based on log-transformed data and geometric mean ratios-standard in pharmacokinetics. The 90% CI must fall within those bounds. It’s not a 45% variance. It’s a 20% allowable deviation in Cmax and AUC, with 90% confidence. The FDA’s standard is actually more rigorous than most countries’. You’re misreading the data.