
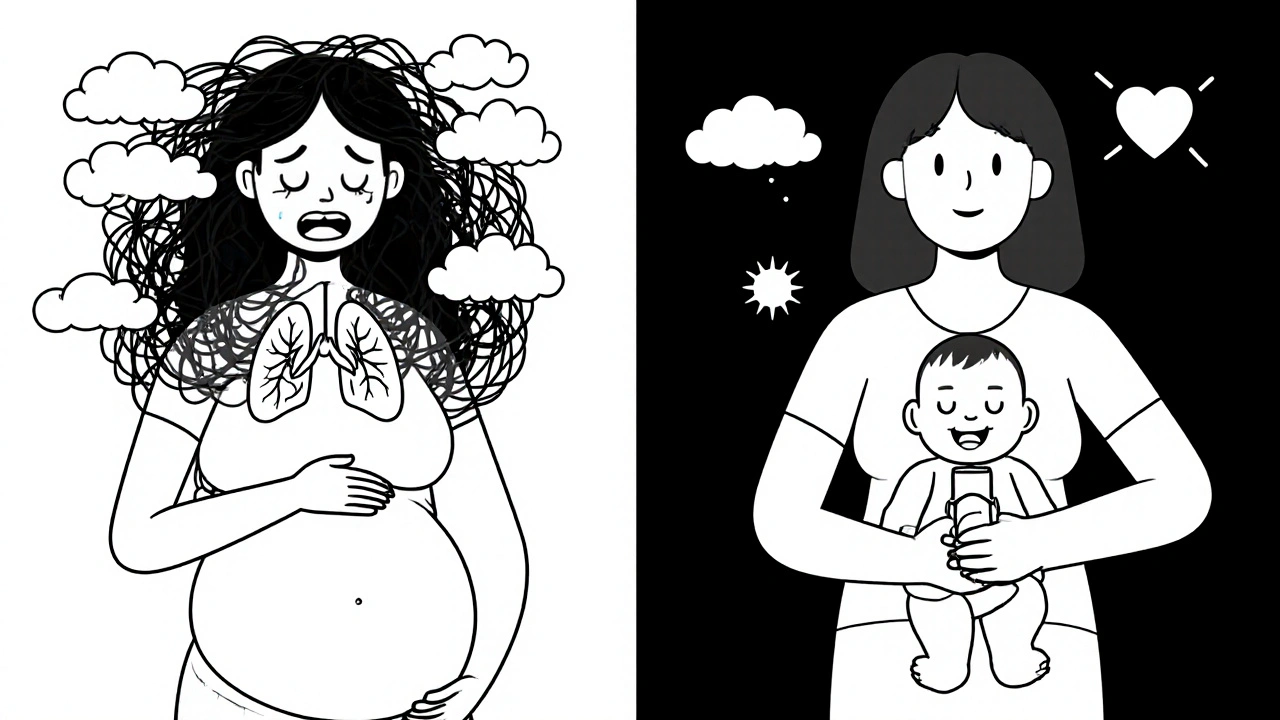
When you’re pregnant and have asthma, the biggest question isn’t just how to manage your symptoms-it’s whether the meds you need could harm your baby. It’s a fear that shows up in online forums, doctor’s offices, and late-night Google searches. But here’s the truth: not treating asthma is far riskier than using the right medications.
Uncontrolled asthma during pregnancy doesn’t just mean more wheezing. It means less oxygen for your baby. That can lead to preterm birth, low birth weight, preeclampsia, and even stillbirth. Studies show that women with poorly managed asthma are 30-60% more likely to have babies with complications. Meanwhile, the medications that keep your lungs open? They’ve been studied in over 100,000 pregnancies. And the data is clear: when used as directed, they’re safe.
What Medications Are Actually Safe?
The gold standard for asthma control during pregnancy is inhaled corticosteroids (ICS). These aren’t the same as oral steroids you might take for a flare-up. Inhaled versions like budesonide, beclomethasone, and fluticasone propionate deliver the medicine straight to your airways. Very little gets into your bloodstream-and even less reaches your baby.
Budesonide has the strongest safety record. Over 1,000 documented pregnancies show no increased risk of birth defects. A 2021 meta-analysis of more than 123,000 pregnancies found no link between budesonide and major congenital malformations. The adjusted odds ratio? 1.01. That’s basically the same as no medication at all.
For quick relief during an attack, albuterol (salbutamol) is your best friend. It’s been used safely in over 1.2 million pregnancies. No increase in birth defects. No need to panic. If you need long-term control beyond ICS, your doctor might add a long-acting beta-agonist like formoterol-but only in combination with an ICS. Studies tracking nearly 38,000 pregnancies found no increased risk of harm.
Montelukast (Singulair), a leukotriene modifier, also has reassuring data. A 2022 review from the European Network of Teratology Information Services looked at 1,045 pregnancies and found no significant rise in major malformations. It’s not first-line, but if you’ve been on it before pregnancy and it works, continuing is generally fine.
What Should You Avoid?
Oral corticosteroids like prednisone are a different story. While they’re life-saving during severe attacks, using them regularly in the first trimester increases the risk of cleft lip or palate by 56%. They also raise the chances of preterm birth and low birth weight. That’s why doctors try to avoid them unless absolutely necessary.
Some newer inhalers lack enough pregnancy data. Fluticasone furoate and ciclesonide? The FDA says there’s insufficient human data. Tiotropium (a LAMA inhaler)? Only 324 documented pregnancies exist. GINA recommends avoiding these as first-line options.
Theophylline, once common, is now rarely used. It requires blood tests to check levels, interacts with many other drugs, and has a narrow safety window. If you’re on it, talk to your doctor about switching to an inhaled option.
And while biologics like omalizumab have promising early data (715 pregnancies with no increased malformation risk), newer ones like mepolizumab or benralizumab? Almost no data. Experts agree: don’t start them during pregnancy unless you’re in a life-threatening situation and under close supervision.
Why Stopping Your Inhaler Is Dangerous
A lot of women stop their asthma meds out of fear. A 2021 Canadian registry found that 41% of women who stopped inhaled corticosteroids during pregnancy had at least one severe asthma attack requiring emergency care. That’s more than double the rate of women who kept taking them.
One mom from Melbourne, Sarah, stopped her budesonide after her first prenatal visit because her OB said, “Better safe than sorry.” Three weeks later, she ended up in the ER with oxygen saturation at 88%. Her baby was born two weeks early. She wasn’t alone. On Reddit’s r/asthma, 82% of comments from pregnant women described being told to reduce or stop their meds-even by doctors who weren’t asthma specialists.
Here’s the hard truth: if your asthma flares, your baby gets less oxygen. That’s not theoretical. It’s measurable. Babies of mothers with uncontrolled asthma have lower Apgar scores, higher NICU admission rates, and more respiratory issues in the first year of life.
The American Academy of Allergy, Asthma & Immunology says ICS use reduces asthma exacerbations by 30-50% during pregnancy-with no increase in birth defects. That’s not a small benefit. That’s the difference between a healthy pregnancy and a high-risk one.
How to Monitor Your Asthma During Pregnancy
It’s not just about taking meds-it’s about tracking how well they’re working. The Global Initiative for Asthma (GINA) recommends:
- Checking your peak expiratory flow (PEFR) daily. Aim to stay above 80% of your personal best.
- Using the Asthma Control Test (ACT). A score of 20 or higher means your asthma is under control.
- Keeping a symptom diary. Note wheezing, night awakenings, and rescue inhaler use.
If your peak flow drops below 70% of your best, or you’re using your rescue inhaler more than twice a week, it’s time to see your doctor. Don’t wait for an emergency.
Monthly visits with your pulmonologist or allergist are ideal, especially if your asthma is moderate to severe. Your OB should be in communication with them. Some clinics now offer joint prenatal asthma appointments at 8, 16, 24, and 32 weeks. That kind of coordination saves lives.
Non-Medication Strategies That Help
Medication isn’t the only tool. Environmental control matters too:
- Use allergen-proof mattress and pillow covers. They cut dust mite exposure by 83%.
- Keep indoor humidity between 30-50%. That reduces mold growth by 67%.
- Remove carpets. They trap allergens-removing them lowers exposure by 55-80%.
- Avoid smoke, strong perfumes, and air pollution. Use air purifiers with HEPA filters.
- Get the flu shot. Pregnant women with asthma are at higher risk for serious flu complications.
These aren’t just nice-to-haves. They’re part of a complete plan. And they work best alongside your prescribed meds-not instead of them.

The Bigger Picture: Why This Matters
For years, asthma in pregnancy was treated like a problem to be minimized-not a condition to be managed. Doctors were afraid to prescribe. Patients were afraid to take. But the science has caught up.
Only 12.7% of asthma drug trials between 2010 and 2022 included pregnant women. That’s changing. The NIH just launched a $15.2 million study tracking 2,500 children born to asthmatic mothers to see how asthma meds affect long-term brain development. That’s progress.
Telemedicine has made follow-ups easier. In 2023, 47% of asthma patients in the U.S. used virtual visits during pregnancy-up from just 5% before the pandemic. That means more consistent monitoring, fewer flare-ups.
And while the FDA replaced the old pregnancy categories (A, B, C, D, X) with the Pregnancy and Lactation Labeling Rule in 2015, many providers still don’t know how to interpret the new format. That’s why you need to be your own advocate. Ask: “What’s the data on this drug in pregnancy? How many women have used it safely?”
What to Do Right Now
If you’re pregnant and have asthma:
- Don’t stop your inhaler. Not without talking to your asthma specialist.
- Get your peak flow meter and start tracking daily.
- Ask your OB to coordinate care with your allergist or pulmonologist.
- Use your rescue inhaler when needed-no guilt.
- Remove carpets, use mattress covers, control humidity.
- Get the flu shot and COVID booster if eligible.
You’re not choosing between your health and your baby’s. You’re choosing to protect both. The safest thing you can do for your baby right now is to keep your asthma under control-with the right meds, the right habits, and the right support.
Is it safe to use an inhaler while pregnant?
Yes, most inhalers are safe during pregnancy. Inhaled corticosteroids like budesonide and rescue inhalers like albuterol have been studied in over 100,000 pregnancies and show no increased risk of birth defects. The real danger is uncontrolled asthma, which can reduce oxygen flow to your baby and lead to serious complications.
Can asthma medication cause birth defects?
The most commonly prescribed asthma medications-inhaled corticosteroids and short-acting beta-agonists-do not increase the risk of birth defects. A 2021 study of more than 123,000 pregnancies found no link between budesonide and major malformations. Oral steroids, however, used in the first trimester, carry a higher risk and should be avoided unless necessary.
What happens if I stop my asthma medication during pregnancy?
Stopping asthma medication can lead to uncontrolled symptoms, which increases the risk of preterm birth, low birth weight, preeclampsia, and even stillbirth. One study found that 41% of women who stopped inhaled steroids had at least one severe asthma attack requiring emergency care-compared to only 17% of those who continued.
Are newer asthma biologics safe during pregnancy?
Omalizumab has data from over 700 pregnancies showing no increased risk of birth defects, so it may be continued if you were already using it. But newer biologics like mepolizumab or benralizumab have almost no safety data in pregnancy. Experts recommend avoiding them unless you’re in a life-threatening situation and under close supervision.
How often should I see a doctor for asthma during pregnancy?
If your asthma is mild and well-controlled, monthly check-ins are usually enough. For moderate to severe asthma, experts recommend joint visits with your OB and asthma specialist at 8, 16, 24, and 32 weeks. Daily peak flow monitoring and an Asthma Control Test score above 20 are key indicators you’re on track.


Comments
Corra Hathaway
OMG I stopped my inhaler bc my OB said 'better safe than sorry'... 3 weeks later I was in the ER with O2 at 88%. My baby was born early. 🤦♀️ Why do doctors say that? Like, we’re not talking about a glass of wine here-we’re talking about oxygen deprivation. Stop the fear-mongering and start the science.
Swati Jain
Let’s cut through the noise: ICS like budesonide have a Class A safety profile in pregnancy per GINA 2023. The odds ratio for congenital malformations is 1.01-statistically indistinguishable from baseline. Meanwhile, uncontrolled asthma increases preterm birth risk by 45%. This isn’t opinion-it’s meta-analysis. Stop listening to anecdotal OBs and consult an allergist. #AsthmaIsNotAnOption
Florian Moser
The data is overwhelming: inhaled corticosteroids reduce exacerbations by 30–50% during pregnancy with no increase in birth defects. The American Academy of Allergy, Asthma & Immunology has clear guidelines. It’s not just safe-it’s medically necessary. Discontinuing treatment is a preventable risk, not a precaution. Please, for your baby’s sake, don’t stop.
jim cerqua
YOU THINK THIS IS ABOUT ASTHMA? NO. THIS IS ABOUT THE PHARMA INDUSTRY PUSHING INHALERS ON PREGNANT WOMEN WHILE THE FDA LOOKS THE OTHER WAY. I read a blog once that said budesonide was developed in a lab that also made Agent Orange. I don’t trust anything that’s ‘been studied in 100,000 pregnancies’-that’s just how they make you feel safe before they take your baby’s future. 🤬
My cousin’s friend’s neighbor’s daughter had a kid with a cleft palate and they said it was ‘probably genetic’-but guess what? She was on ‘safe’ meds. Coincidence? I think not.
Donald Frantz
Where’s the raw data? You cite meta-analyses but don’t link to the studies. Who funded them? How many of the 123,000 pregnancies were in the U.S.? What’s the control group? And why is fluticasone furoate listed as ‘insufficient data’ but budesonide is gold standard? If this is evidence-based medicine, show me the PubMed IDs. Otherwise, it’s just marketing.
Sammy Williams
My OB didn’t know squat about asthma. My pulmonologist said ‘keep using your inhaler’ and I did. Baby’s 2 now, no issues, no NICU. I also got rid of my carpet and used those mattress covers-best $30 I ever spent. Honestly, the combo of meds + clean air = peace of mind. You’re not choosing between you and the baby. You’re choosing to be a better mom. Simple.
Julia Strothers
They’re lying to you. All of them. The ‘100,000 pregnancies’? That’s a lie cooked up by Big Pharma to sell more inhalers. The FDA didn’t approve budesonide for pregnancy-they just let it slide. And now they’re pushing ‘joint appointments’? That’s a trap. You think your OB cares? They get paid per visit, not per healthy baby. You’re being groomed to be a drone on the pharmaceutical conveyor belt. Wake up.
Erika Sta. Maria
But what if the real danger is the *medication* and not the asthma? Like, maybe the body knows better? Maybe the inflammation is a *spiritual signal*? I read on a forum that in ancient Vedic texts, asthma was called ‘the breath of the soul being tested’-and if you suppress it with chemicals, you’re blocking your karma. Also, I think the word ‘budesonide’ is an anagram for ‘dumb science’… just saying.
Elaina Cronin
It is with profound concern that I must address the alarming prevalence of misinformation surrounding asthma management in pregnancy. The empirical evidence, as presented in peer-reviewed literature from the Journal of Allergy and Clinical Immunology, unequivocally supports the continued use of inhaled corticosteroids. To suggest otherwise constitutes a dereliction of medical duty. I implore all expectant mothers to seek care from certified allergists, not general practitioners who lack subspecialty training. The consequences of inaction are not hypothetical-they are statistically significant and ethically indefensible.
Willie Doherty
The cited meta-analyses are methodologically flawed. Selection bias is evident in the exclusion of low-income populations where environmental triggers dominate. Furthermore, the use of ‘adjusted odds ratio’ obscures absolute risk. A 1.01 OR is meaningless without baseline incidence. Until longitudinal data from underrepresented demographics is published, clinical recommendations remain premature. I remain unconvinced.
Darragh McNulty
Just want to say-your baby can feel your stress. If you’re terrified of your inhaler, that’s worse than the med. I used my albuterol like a lifeline. My son is 4 now, runs circles around me. 🤗 Stay calm. Stay medicated. Stay alive. You got this.
Cooper Long
As a father of two asthmatic children born to a mother who used budesonide throughout pregnancy, I can attest that the real danger is ignorance. The science is clear. The fear is manufactured. The choice is simple: control or suffer. I’ve seen both outcomes. Choose wisely.
Franck Emma
I stopped my inhaler. My baby died at 36 weeks. They told me it was ‘unexplained.’ Now I know. I should’ve listened to the asthma specialist. Not the OB. Not the internet. Not the ‘better safe than sorry’ idiots. I’m still not okay.
Sheldon Bazinga
bro i got a 300k dollar bill for my kid’s NICU stay bc i listened to my doctor and kept my inhaler. now im broke and my baby has asthma. so… who’s the real villain here? 🤡