Fluoroquinolone & NSAID Risk Calculator
Medication Risk Assessment
This tool helps you understand the combined risk of taking fluoroquinolone antibiotics and NSAIDs. Based on your age, kidney function (eGFR), and medication use, it assesses your risk of kidney damage or neurological complications.
Risk Assessment Results
When you’re dealing with a bad infection and painful inflammation, it’s tempting to grab a fluoroquinolone antibiotic like ciprofloxacin or levofloxacin along with an over-the-counter NSAID like ibuprofen or naproxen. It seems logical-kill the bacteria and calm the pain at the same time. But what looks like a smart shortcut could actually be a dangerous combo. The truth is, mixing these two drug classes doesn’t just raise the risk of side effects-it can trigger fluoroquinolone antibiotics and NSAIDs to team up in ways that seriously harm your nerves and kidneys.
How Fluoroquinolones Work-and What They Can Break
Fluoroquinolones, including ciprofloxacin, levofloxacin, and moxifloxacin, are powerful antibiotics used for stubborn infections like urinary tract infections, pneumonia, and certain types of gastrointestinal illness. They work by blocking bacterial DNA replication, which is why they’re so effective. But they don’t just target bacteria. These drugs also interfere with human enzymes involved in DNA repair and mitochondrial function. That’s where things go wrong.Over time, evidence has piled up showing that fluoroquinolones can cause long-term damage to tendons, nerves, and the central nervous system. Health Canada, the European Medicines Agency, and the U.S. FDA have all issued strong warnings. In 2017, Health Canada concluded that side effects like tendon rupture, peripheral neuropathy, and brain fog could be persistent and disabling-even after stopping the drug. The UK’s MHRA followed suit in 2019, restricting these antibiotics to cases where no other treatment works.
One of the most alarming findings? Up to 78% of patients surveyed by the Fluoroquinolone Effects Research Foundation reported symptoms lasting more than six months after treatment. Some never fully recover. This isn’t rare. It’s underreported.
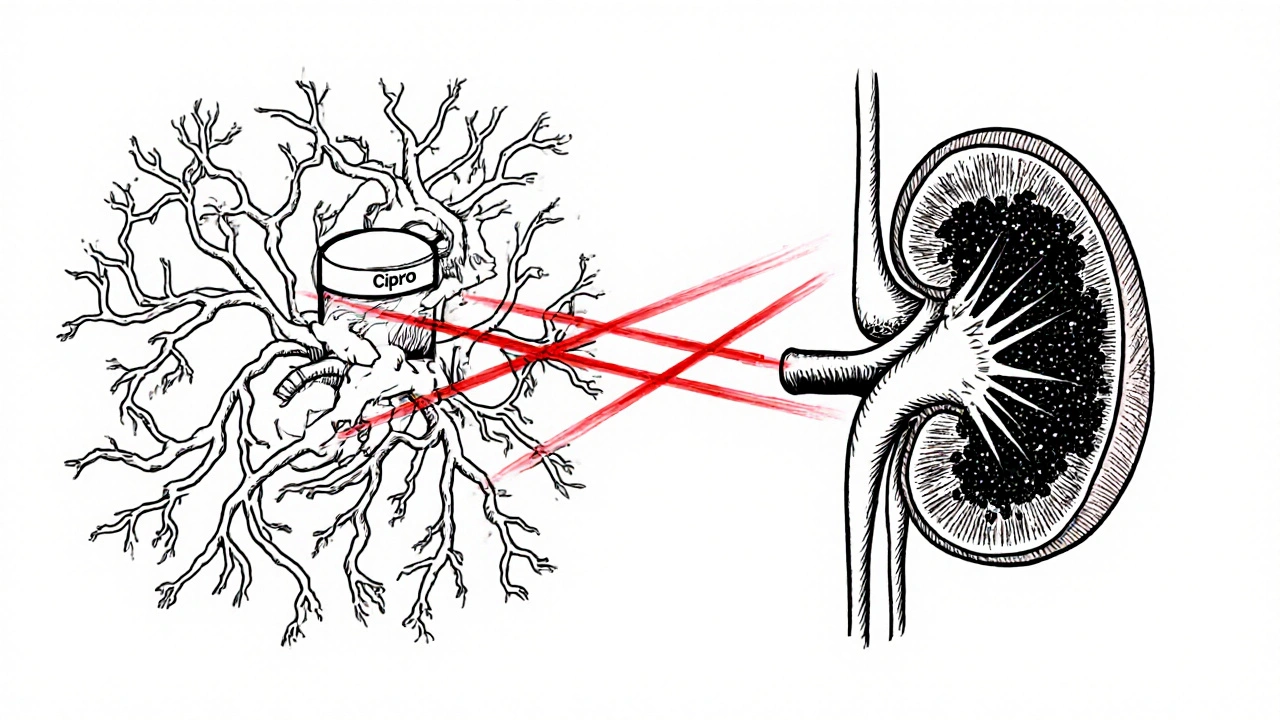
NSAIDs and the Kidney Connection
NSAIDs like ibuprofen, naproxen, and diclofenac are everywhere. They’re used for headaches, arthritis, menstrual cramps, and fever. But they’re not harmless. These drugs block prostaglandins, chemicals your kidneys need to maintain blood flow and filter waste. In healthy people, that’s usually fine. But in older adults, those with existing kidney issues, or anyone who’s dehydrated, NSAIDs can quickly reduce kidney function.Studies show that NSAIDs alone can increase the risk of acute kidney injury (AKI) by 20-40% in vulnerable populations. The risk jumps even higher in people over 60, where kidney function naturally declines by about 1% per year after age 40. And when you add a fluoroquinolone into the mix? The danger multiplies.
The Perfect Storm: Fluoroquinolones + NSAIDs
There’s no direct clinical trial proving this combo causes more kidney damage than either drug alone-but real-world data doesn’t lie. A landmark 2013 study in JAMA Internal Medicine found that patients taking both a fluoroquinolone and an NSAID had up to a 3.5-fold higher risk of hospitalization for acute kidney injury compared to those taking neither.Here’s why: Fluoroquinolones are cleared by the kidneys. When kidney function dips-even slightly-drug levels in the blood rise. That’s bad news. Fluoroquinolone concentrations can spike by 50-100% in people with moderate kidney impairment (eGFR 30-59 mL/min/1.73m²). At the same time, NSAIDs reduce blood flow to the kidneys, making it harder for the body to flush out the antibiotic. The result? Toxic buildup.
Case reports back this up. One UK patient, a 58-year-old man, developed acute kidney injury (creatinine jumped from 82 to 287 μmol/L) and severe nerve pain after taking ciprofloxacin and ibuprofen together for a UTI. Eighteen months later, he still had symptoms. His case was logged in the UK’s Yellow Card system-proof this isn’t theoretical.
Neurological Risks: When Your Brain Gets Caught in the Crossfire
Fluoroquinolones don’t just mess with your kidneys. They can cross the blood-brain barrier and disrupt neurotransmitters. Specifically, they block GABA receptors (which calm brain activity) and stimulate NMDA receptors (which excite neurons). This imbalance can trigger seizures, confusion, hallucinations, delirium, and even psychosis.Levofloxacin is especially linked to seizures and delirium. Ciprofloxacin often causes brain fog and anxiety. Even people with no history of mental health issues can be affected. The risk goes up if you’re older, have kidney problems, or are on other medications that affect the brain.
NSAIDs aren’t innocent here either. While they rarely cause serious neurological problems, they can trigger headaches, dizziness, and-very rarely-aseptic meningitis, especially with ibuprofen and naproxen. When combined with fluoroquinolones, these effects aren’t just added together-they’re amplified. The brain gets hit from two sides: chemical disruption from the antibiotic and reduced clearance from kidney stress.
Who’s Most at Risk?
This combo isn’t dangerous for everyone. But certain groups need to avoid it completely:- People over 60
- Anyone with eGFR below 60 mL/min/1.73m² (signs of kidney impairment)
- Those with a history of seizures, epilepsy, or psychiatric disorders
- Patients on dialysis or with chronic kidney disease
- Anyone taking corticosteroids (which also raise tendon and nerve risks)
Even if you’re young and healthy, don’t assume you’re safe. Fluoroquinolone toxicity can strike without warning. One study found that 32% of patients who developed long-term disability after fluoroquinolone use had no prior risk factors.
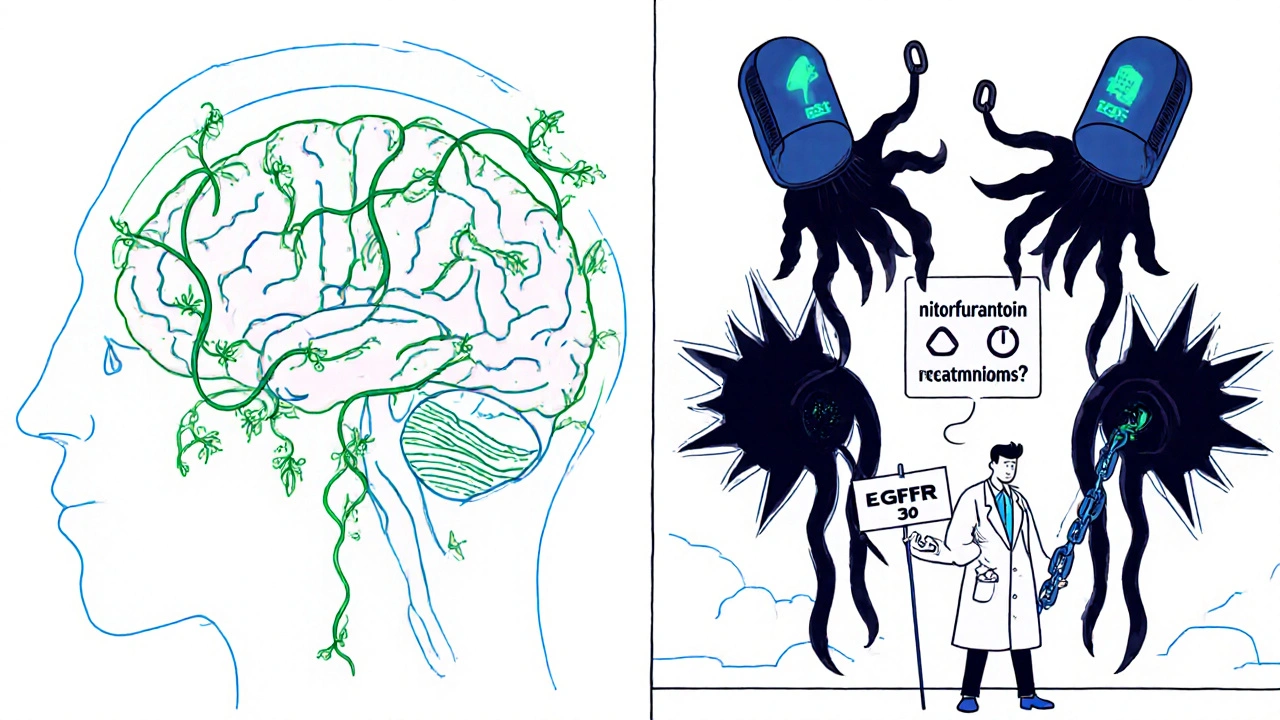
What Should You Do Instead?
If you need an antibiotic and pain relief, here’s what to ask your doctor:- For UTIs: Nitrofurantoin or fosfomycin are safer alternatives to fluoroquinolones.
- For respiratory infections: Amoxicillin-clavulanate or doxycycline are often just as effective and carry lower neurological and renal risks.
- For pain: Switch from NSAIDs to acetaminophen (paracetamol). It doesn’t harm the kidneys or interfere with fluoroquinolone clearance.
And if you’re already on both drugs? Don’t stop abruptly. Talk to your doctor. They may need to adjust your dose, monitor your kidney function with blood tests, or switch you to a safer option.
The Bigger Picture: Why This Is Still Happening
Despite warnings from regulators and mountains of evidence, fluoroquinolones are still prescribed far too often. In the U.S., prescriptions dropped 22% between 2015 and 2022-but they’re still handed out for mild infections like sinusitis or bronchitis, where they offer little benefit.Meanwhile, NSAIDs are treated like candy. People pop them daily without realizing the toll on their kidneys. Combine that with the fact that many patients don’t tell their doctors about OTC meds they’re taking, and you’ve got a perfect storm of hidden risk.
The economic cost is staggering. A 2020 study estimated fluoroquinolone-related adverse events cost the U.S. healthcare system $1.8 billion annually. Kidney injuries made up 37% of those costs. Neurological complications added another 29%.
And it’s not just money. It’s quality of life. Patients in online communities like r/FQAntibioticDamage describe chronic pain, brain fog, and fatigue that lasts years. Some can’t work. Some can’t walk. These aren’t side effects-they’re life-altering.
Bottom Line: Think Before You Mix
Fluoroquinolones and NSAIDs are both useful drugs. But together, they’re a high-risk pair. The risks aren’t just possible-they’re proven. And they’re not rare.If your doctor prescribes a fluoroquinolone, ask: Is this really necessary? Are there safer options? And if you’re taking NSAIDs for pain, tell them. Don’t assume they know. Your kidneys and your brain can’t afford the guesswork.
There’s no shame in choosing a slower, safer path. Sometimes, the best medicine is the one you don’t take.


Comments
Edward Ward
It's wild how we treat antibiotics like they're candy, and NSAIDs like they're harmless aspirin. The science here is crystal clear: fluoroquinolones mess with mitochondrial DNA repair, and NSAIDs choke off renal perfusion. Together, they create a perfect storm where your kidneys can't clear the drug, and your neurons start firing erratically. This isn't anecdotal-it's in the JAMA study, the FDA warnings, the Yellow Card reports. Yet doctors still prescribe cipro for sinus infections like it's a vitamin. We've normalized medical negligence because it's faster and cheaper. The real tragedy? Most patients don't even know they were given a high-risk combo until they're already in the ER with elevated creatinine and brain fog that won't quit.
Jessica Chambers
My aunt took cipro and ibuprofen for a UTI. Three months later, she couldn’t walk without a cane and kept forgetting her own birthday. No one told her this could happen. Now she’s on disability. 💔
John Foster
The system is designed to ignore the silent suffering of patients who don't fit the demographic of "high-risk." Young, healthy, middle-class people get prescribed fluoroquinolones like they're a reward for having a fever. But the damage doesn't discriminate by age or fitness-it discriminates by ignorance. The pharmaceutical industry doesn't care about your tendons or your mitochondria; they care about market share. And the medical establishment? They're too busy checking boxes to look up the latest meta-analyses on fluoroquinolone toxicity. We're living in an era where informed consent is a formality, not a right. The fact that 78% of survivors report symptoms beyond six months isn't a statistical outlier-it's a systemic failure. And yet, we keep handing out these prescriptions like they're coupons for a free latte.
BABA SABKA
Fluoroquinolones are basically chemical weapons disguised as medicine. The fact that the FDA didn't ban them outright is a testament to how corrupted our regulatory bodies are. NSAIDs are just the accomplice-making the neurotoxicity worse by reducing renal clearance. This isn't medicine, it's pharmacological warfare on the civilian population. And don't get me started on how acetaminophen is the only safe alternative. That's the real conspiracy-Big Pharma pushing NSAIDs because they're profitable, while acetaminophen is generic and cheap. They want you dependent on the expensive, dangerous stuff.
Jonathan Dobey
Let’s be real: fluoroquinolones are the pharmaceutical equivalent of a nuclear bomb in a toy store. They were designed to obliterate bacteria, but they don’t discriminate-they obliterate your mitochondria, your tendons, your GABA receptors, your sanity. And NSAIDs? They’re the guy who hands you the match after you’ve already set the house on fire. The real horror isn’t the data-it’s the silence. The medical community has known about this for decades. They’ve got case reports, longitudinal studies, and regulatory warnings. Yet every year, millions still get prescribed this combo. Why? Because doctors are overworked, underpaid, and trained to trust the algorithm, not the evidence. The patient? They’re just a data point in a profit margin. This isn’t negligence. It’s complicity.
Andrew Eppich
It is unfortunate that anecdotal narratives are being elevated above evidence-based guidelines. While the risks of fluoroquinolones and NSAIDs are documented, the incidence of severe adverse events remains low in the general population. The majority of patients tolerate these medications without issue. The concern expressed here is disproportionate to the actual data. Physicians are trained to weigh benefits against risks, and in many cases, fluoroquinolones remain the most effective option for serious infections. Dismissing them outright based on outlier cases is irresponsible and may lead to increased morbidity from untreated infections. Acetaminophen is indeed preferable for pain, but it is not without its own hepatic risks. A balanced approach is required.
Ogonna Igbo
You Americans act like you invented medicine. In Nigeria we know how to treat infections without your fancy pills. We use herbs, clean water, and rest. Your drugs are poison. Your doctors don't care about you. They care about money. You take cipro and ibuprofen because you are lazy. In my country we don't need your toxic pills to survive. We are stronger than you think.
Chris Bryan
This whole post is a liberal scare tactic. Fluoroquinolones are safe. The FDA didn't ban them. The WHO still lists them as essential. The real danger is people like you spreading fear instead of facts. NSAIDs? Everyone takes them. Your kidneys will be fine. This is just another way to make people distrust science. If you're scared of antibiotics, don't take them. But don't drag down the entire medical system because you read a blog post. Also, why are you even on Reddit? Go touch grass.
Shyamal Spadoni
fluoroquinolone? NSAID? i think its all about the chemtrails and 5g. the government wants us to get kidney damage so they can sell us more drugs. also the moon landing was fake. i took cipro once and my left toe tingled for 3 days. that was the start. now i cant sleep. they put something in the water. the doctors are all in on it. i saw a video on youtube where a guy said the same thing. he had a tattoo of a kidney on his arm. he died. now im scared. i dont trust anyone. even my dog looks at me weird now.