
Opioid Dose Adjuster for Older Adults
Opioid Dose Calculator
Based on CDC and geriatric guidelines, calculate a safe starting dose for older adults. Remember: Start low, go slow.
Enter your information and click Calculate to see the recommended starting dose.
Why Opioids Are Riskier for Older Adults
Older adults don’t process opioids the same way younger people do. Their kidneys and liver don’t clear drugs as quickly. Their body fat increases while muscle mass declines. Their blood-brain barrier becomes more permeable. These changes mean even small doses can cause big problems-sedation, confusion, dizziness, and a much higher chance of falling.
Between 2005 and 2014, emergency room visits for opioid-related issues in people 65 and older jumped by over 110%. That’s not just a trend-it’s a crisis. And it’s not just about addiction. Many older adults are prescribed opioids for chronic pain, but they don’t realize how dangerous these drugs can be for their age group.
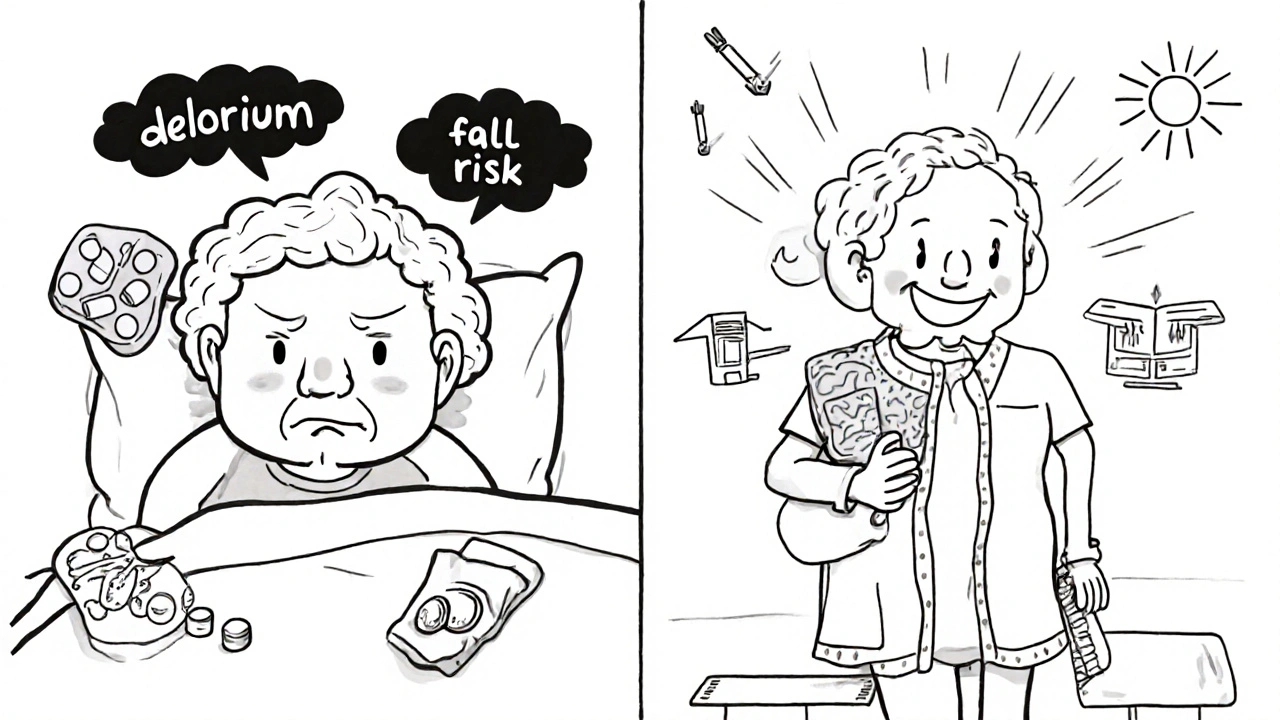
Falls: A Silent but Deadly Consequence
Falls are the leading cause of injury and death in older adults. Opioids make them far more likely. How? They slow down reaction time, blur vision, lower blood pressure when standing up, and cause dizziness. Even weak opioids like tramadol can trigger hyponatremia-a drop in sodium levels-that leads to confusion and unsteadiness.
One study of 2,341 adults over 60 found that those taking opioids had a 6% fracture rate over 33 months, compared to 4% in those not taking them. The difference wasn’t quite statistically significant, but the pattern was clear: opioids = more falls = more broken hips and skulls.
And it’s not just the drug itself. When opioids are mixed with other medications-like benzodiazepines, antidepressants, or even over-the-counter sleep aids-the risk multiplies. Drug interactions affect enzymes like CYP2D6 and CYP3A4, which are already slower in older adults. The result? More sedation, longer-lasting effects, and a higher chance of ending up in the hospital after a fall.
Delirium: When Pain Meds Cause Confusion
Delirium isn’t just "being forgetful." It’s a sudden, dangerous shift in mental state-confusion, hallucinations, agitation, or extreme drowsiness. In older adults, especially those with dementia, opioids are a major trigger.
A 2023 study of 75,471 Danes over 65 with dementia found that those who started opioids had an elevenfold higher risk of dying in the first two weeks. That’s not a typo. Eleven times. The researchers didn’t find this was due to overdose alone. It was the brain’s reaction to the drug-disrupting alertness, sleep cycles, and cognition.
Doctors often mistake delirium for worsening dementia. Families think Grandma is just "getting worse." But if she started an opioid last week and now doesn’t recognize her own children, it might not be dementia-it might be the medicine.
Dose Adjustments: Start Low, Go Slow
There’s no such thing as a "normal" opioid dose for older adults. What’s safe for a 40-year-old can be deadly for a 75-year-old. Experts agree: start at 25 to 50% of the usual adult dose. Then wait. Watch. Reassess.
For example, if a younger patient gets 10 mg of oxycodone every 6 hours, an older adult might start with 2.5 mg every 8 hours. And even that might be too much. Some patients need only 1 mg every 12 hours to get relief.
It’s not about being stingy. It’s about precision. Older adults need less, but they also need careful monitoring. Are they sleeping too much? Are they stumbling in the hallway? Do they seem foggy after taking their pill? If yes, the dose is too high.
Don’t wait for a fall to happen. Check in weekly. Use simple tools like the STOPPFall checklist-designed by geriatric specialists-to help decide if the opioid is doing more harm than good.
Deprescribing: When It’s Time to Stop
Many older adults have been on opioids for years. They think they need them. But long-term use doesn’t always mean better pain control. Often, it just means more side effects.
Deprescribing isn’t about quitting cold turkey. It’s about reducing slowly, with support. Tapering too fast can cause withdrawal-sweating, nausea, anxiety, insomnia. But tapering too slow keeps the risks alive.
Start by cutting the dose by 10-20% every 1-2 weeks. Watch for pain flare-ups and withdrawal signs. Replace opioids with non-drug options: physical therapy, heat packs, acupuncture, or even cognitive behavioral therapy for pain.
And here’s the hard truth: many older adults resist stopping opioids because they fear pain will return. But what they don’t realize is that the opioids themselves may be making their pain worse over time-through a condition called opioid-induced hyperalgesia, where the nervous system becomes more sensitive to pain.
What Doctors and Families Should Do
Primary care doctors often feel unprepared. Nearly half say they lack confidence in tapering opioids safely. And older patients? They rarely bring up side effects. They’re afraid of being seen as complainers. Or they don’t know what’s normal.
Here’s what works:
- Ask directly: "Have you felt dizzy or confused since starting this medicine?"
- Review every pill in the medicine cabinet-not just opioids, but everything.
- Use the START/STOPP criteria: a proven checklist for safe prescribing in older adults.
- Involve pharmacists. They spot dangerous interactions doctors miss.
- Build trust. If the patient doesn’t feel heard, they won’t agree to change.
And families: don’t assume your parent is just aging. If they’re suddenly falling, forgetting names, or sleeping all day, ask: "Could this be the pain meds?"
Non-Opioid Alternatives That Actually Work
Opioids aren’t the only option. And often, they’re not the best one.
- Physical therapy: Strength and balance training reduce pain and prevent falls.
- Topical NSAIDs: Creams or gels with diclofenac or ibuprofen work for joint pain with almost no systemic side effects.
- Cognitive behavioral therapy: Helps reframe how the brain perceives pain.
- Acupuncture and massage: Proven to help chronic back and knee pain in older adults.
- TENS units: Small devices that send gentle electrical pulses to block pain signals.
These options don’t come with a risk of delirium or a broken hip. They take more time and effort-but they’re safer, and often just as effective.
The Bottom Line
Opioids aren’t evil. They have a place in pain management. But for older adults, the risks often outweigh the benefits. Falls, delirium, heart attacks, and early death aren’t side effects-they’re predictable outcomes when doses aren’t adjusted for age.
The solution isn’t to stop all opioids. It’s to start smarter. Prescribe less. Monitor closer. Replace when possible. And always ask: "Is this helping, or just hiding the problem?"
If you or someone you love is over 65 and on opioids, talk to a doctor. Ask about alternatives. Ask about dose reduction. Ask about fall risk. Don’t wait for a fall to happen before you act.
Can opioids cause dementia in older adults?
Opioids don’t cause dementia, but they can trigger delirium-which looks a lot like dementia and can worsen existing cognitive decline. In people with early dementia, starting opioids can lead to sudden confusion, memory loss, and disorientation. A 2023 study found that dementia patients who started opioids had an elevenfold higher risk of death in the first two weeks, largely due to this confusion and its complications.
Is tramadol safer than other opioids for seniors?
No. Tramadol is often seen as "milder," but it’s particularly risky for older adults. It can cause hyponatremia (low sodium), leading to dizziness, confusion, and falls. It also interacts with many common medications and affects brain chemistry differently than other opioids. Many geriatric experts now avoid tramadol entirely in patients over 70.
How do I know if my parent is physically dependent on opioids?
Physical dependence means the body adapts to the drug. Signs include needing higher doses for the same effect, withdrawal symptoms like sweating, nausea, or anxiety when the dose is missed or reduced, and persistent pain even when the original injury has healed. Dependence isn’t addiction-it’s a physiological response. It can happen in as little as a few days with regular use.
Should I stop opioids cold turkey if my elderly parent is having side effects?
Never stop abruptly. Sudden withdrawal can cause dangerous symptoms like high blood pressure, rapid heart rate, seizures, or severe anxiety. Always work with a doctor to taper slowly-usually by 10-20% every 1-2 weeks. Monitor for both pain flare-ups and withdrawal signs. Support from a pharmacist or geriatric specialist makes this safer.
Are there guidelines for prescribing opioids to older adults?
Yes. The CDC, FDA, and professional geriatric societies all recommend the "start low, go slow" approach. Initial doses should be 25-50% lower than for younger adults. Use the START/STOPP criteria to guide prescribing. Avoid long-acting opioids unless absolutely necessary. Always consider non-opioid options first. The STOPPFall tool is now recommended for patients at risk of falls.
Can opioids increase the risk of heart problems in seniors?
Yes. A study of nearly 300,000 patients found that taking opioids for 180 days or more over 3.5 years nearly tripled the risk of heart attack. Even shorter use increases the odds by about 28%. Opioids can raise blood pressure, slow heart rate irregularly, and increase inflammation-all bad for older hearts. This risk is often overlooked because pain management focuses on relief, not long-term cardiovascular impact.
What Comes Next?
If you’re managing opioids for an older adult, the next step is simple: schedule a medication review. Bring every pill bottle-prescription, over-the-counter, supplements-to your doctor or pharmacist. Ask: "Is this still necessary?" "Could it be causing dizziness or confusion?" "Are there safer alternatives?"
Change doesn’t have to be dramatic. Sometimes, cutting one pill in half, switching to a topical cream, or adding a daily balance exercise makes all the difference. The goal isn’t to live without pain. It’s to live without fear-of falling, of forgetting, of dying too soon because a pill didn’t fit the person taking it.


Comments
satya pradeep
Man, I’ve seen this too many times-Grandpa on oxycodone for his knee, now he’s tripping over his slippers and calling his dog "Mom." Doc says it’s "just aging." Nah. It’s the pills. Start low, go slow? More like START ZERO and SKIP THE OPIATES ALTOGETHER.
Prem Hungry
Dear all, I am writing this with utmost sincerity. As a caregiver to my 78-year-old father, I can confirm that opioids, even in small doses, induce profound cognitive fog. We switched him to topical diclofenac and daily tai chi. His balance improved. His memory returned. His eyes sparkled again. Please, if you are prescribing or managing such medications-choose wisely. There is always a better way.
Leslie Douglas-Churchwell
Let’s be real-this is Big Pharma’s greatest scam since the tobacco industry said smoking was safe. 🤡 They’ve been pushing opioids on seniors for decades because it’s profitable, not because it’s ethical. And now we’re told to "start low"? Like we didn’t already know? The FDA is complicit. The AMA is complicit. The entire medical-industrial complex is built on exploiting the elderly. 🚨💊 #OpioidCrisis #CorporateMurder
shubham seth
Tramadol? More like Trama-DANGER. It’s the opioid version of a fake ID-looks harmless, but it’s got a secret stash of sodium-sucking, brain-fogging, fall-inducing poison. And don’t get me started on the CYP enzyme chaos. Older folks aren’t just slow-they’re sitting ducks for pharmacokinetic grenades. I’ve seen 80-year-olds turn into zombies after one week of tramadol. It’s not pain management. It’s chemical sedation with a side of funeral planning.
Kathryn Ware
I’m a geriatric nurse and I see this every single shift. A woman came in last week with a hip fracture-she’d been on 10mg oxycodone daily for 3 years. We tapered her down to 1mg every 12 hours, added PT, and gave her a TENS unit. She cried because she thought she’d never walk without pain again… then she stood up on her own two feet two days later. No opioids. Just patience, love, and science. 💙 Please, if you’re reading this and your parent is on opioids-ask for a med review. Don’t wait for the fall. The system fails them every day. We can change that. One pill at a time.
kora ortiz
Stop opioids in seniors. Now. Not tomorrow. Not next week. Now. Falls kill. Delirium destroys. And your grandma doesn’t need a chemical crutch-she needs movement, connection, and respect. Replace the pills with physical therapy, heat, and human touch. You think you’re helping? You’re just delaying the inevitable. Take action today.
Jeremy Hernandez
Lol. So now we’re blaming the drugs? What’s next? The sun causes dementia? People are just getting old. You think Grandma’s confused because of oxycodone? Nah. She’s just forgetful. And if she’s falling, maybe she needs a walker, not a drug ban. This whole thing feels like woke medicine. Next they’ll say coffee causes heart attacks. 🤷♂️
Tarryne Rolle
Is the real issue here the medicalization of aging? We’ve turned the natural decline of the body into a pathology to be pharmacologically suppressed. Opioids are merely the symptom of a culture that refuses to sit with pain, to honor the dignity of frailty. To deprescribe is not just to reduce dosage-it is to reject the illusion that every ache must be erased. Perhaps the deeper question is: why do we fear old age so much that we poison it?
Kelsey Robertson
Wow. So we’re just supposed to ‘taper’? Like this is some kind of yoga retreat? People are dying from delirium and falls because doctors are too lazy to think critically. And now we’re supposed to trust pharmacists? Please. They’re just the ones who print the labels. The real problem? No one wants to admit that aging means dying-and opioids are just the Band-Aid on a corpse.
Joseph Townsend
My aunt went from ‘walking the dog every morning’ to ‘sleeping in a chair for 18 hours’ after her doctor gave her 5mg oxycodone for a sprained ankle. She didn’t get better. She got ghosted. We found her meds in a drawer labeled ‘emergency pain relief’-she’d been taking two pills a day for 8 months. Eight months. For a sprain. That’s not medicine. That’s a slow-motion tragedy with a prescription pad.
Bill Machi
Why are we letting foreigners tell us how to treat our elders? This is American medicine. We don’t need some hippie checklist from California to tell us opioids are dangerous. My dad’s 79 and he’s still hunting. He needs his meds. If he falls, he falls. That’s life. Stop over-medicalizing everything. You think Europe’s doing better? Look at their healthcare bills. We do things differently here. And we’re not wrong.
Elia DOnald Maluleke
There is a sacred contract between the body and time. To intervene with chemical force against the natural unraveling of age is to insult the dignity of decay. Opioids are not the villain-they are the mirror. They reflect our collective terror of vulnerability. The real crisis is not the dose-it is our refusal to hold the hand of the aging without reaching for a pill. Let them feel the pain. Let them feel the silence. Let them feel the truth. That is the only medicine left that still carries grace.
Kyle Swatt
I’ve been in hospice for 12 years. I’ve held hands as people faded. And I’ve seen the difference between a person on opioids and one who’s been gently weaned. The ones who stopped? They smiled more. They recognized their grandkids. They whispered stories instead of staring at the ceiling. The opioids didn’t take away pain-they took away presence. And presence? That’s the only thing worth fighting for at the end.
Deb McLachlin
Thank you for this comprehensive and clinically grounded overview. The data on CYP450 enzyme activity decline in geriatric populations is particularly compelling. I would like to add that the STOPPFall tool, while useful, is underutilized in primary care settings due to systemic time constraints and lack of reimbursement for medication reconciliation. Furthermore, the integration of pharmacogenomic testing-especially for CYP2D6 poor metabolizers-could revolutionize individualized dosing. Unfortunately, insurance barriers prevent widespread adoption. This is not merely a clinical issue-it is a policy failure.
saurabh lamba
Bro, I’m just saying… if your grandma’s on pain meds and she’s acting weird, maybe she just needs a nap and some chai. Not a whole lecture on pharmacokinetics. 😴🍵