When you pick up a prescription, you might see two options: the name you recognize from TV ads, or a cheaper one with a long chemical name you’ve never heard of. You might wonder - is the cheaper one just as good? The answer isn’t just yes, it’s proven - and the science behind it is clearer than most people realize.
They’re Not Just Similar - They’re the Same
Generic drugs aren’t "close enough" versions of brand-name drugs. They are required by law to be exact matches in one critical way: the active ingredient. That’s the part that actually treats your condition. Whether you take Lipitor or its generic, atorvastatin, your body gets the same molecule, in the same amount, delivered the same way - whether it’s a pill, capsule, or injection.
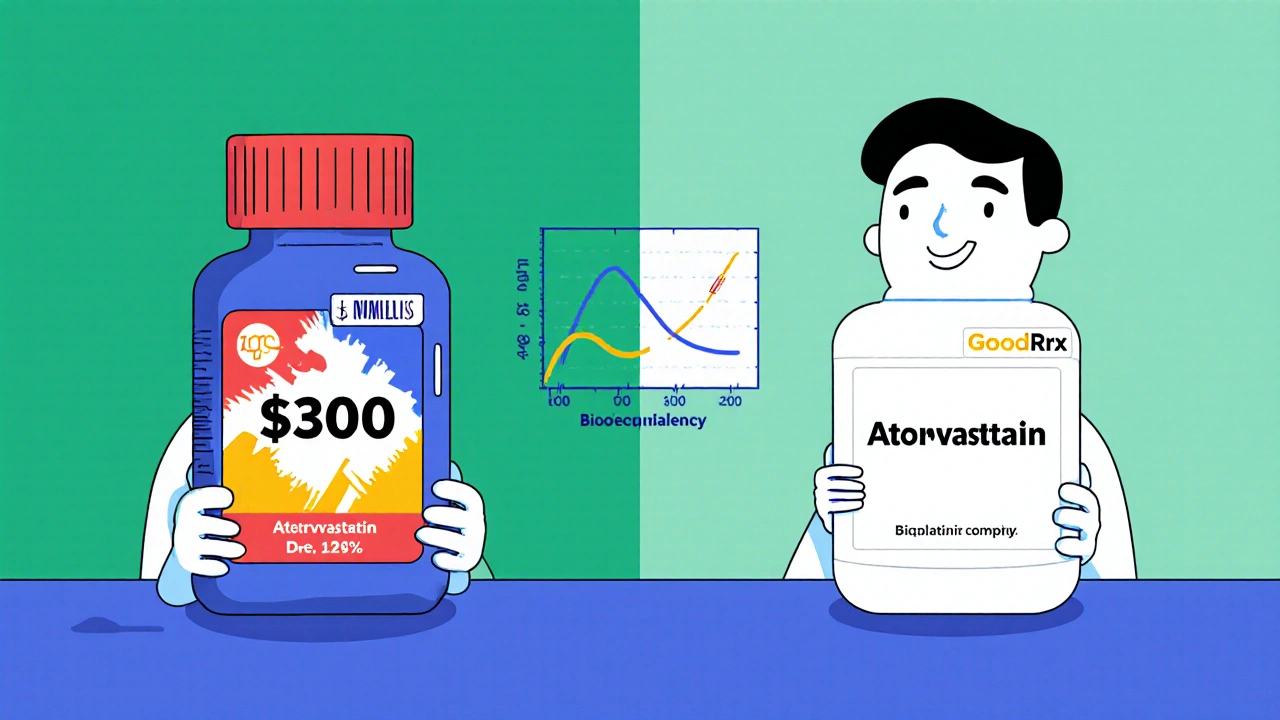
The FDA doesn’t just trust manufacturers to say it’s true. Every generic must pass a strict test called bioequivalence. That means in studies with healthy volunteers, the generic must release the drug into the bloodstream at the same rate and to the same extent as the brand. The standard? The amount of drug absorbed (measured as AUC) and the peak level (Cmax) must fall within 80% to 125% of the brand’s numbers. That’s not a wide gap - it’s a tight one. In fact, studies show the average difference in absorption between generics and brands is less than 4%. That’s less than what you’d see if you took the same brand drug on an empty stomach versus after a meal.
Cost? A Massive Difference
Here’s where the real win comes in. Generic drugs cost, on average, 80% to 85% less than their brand-name counterparts. That’s not a small discount. That’s life-changing for people on fixed incomes, for families juggling medical bills, and for the whole healthcare system.
In 2023 alone, generic drugs saved the U.S. healthcare system an estimated $373 billion. Let that sink in. That’s money that didn’t go to drug companies - it went to patients’ pockets, to lower insurance premiums, and to funding other care.
Take statins - the cholesterol-lowering drugs. The brand-name Lipitor might cost over $300 for a 30-day supply. The generic? Often $0 with a coupon from GoodRx. Plavix, a blood thinner, runs about $450 brand-name. The generic? Again, $0. These aren’t hypotheticals. These are real prices patients pay every day.
But What About the Exceptions?
There’s a reason you hear people say, "My doctor won’t let me switch." It’s not because generics don’t work - it’s because some drugs are more sensitive.
Drugs with a narrow therapeutic index (NTI) are the exception. These are medications where even a tiny change in blood level can cause big problems - too little and the drug doesn’t work; too much and it becomes toxic. Examples include warfarin (a blood thinner), levothyroxine (for thyroid issues), phenytoin (for seizures), and lithium (for bipolar disorder).
For these, doctors and pharmacists may recommend sticking with one version - brand or generic - and monitoring blood levels closely after a switch. That’s not because generics are less effective. It’s because these drugs leave no room for error. The FDA still approves generics for NTI drugs, but the margin for variation is tighter, and monitoring is part of the safety plan.
Real People, Real Stories
Despite the data, skepticism lingers. On Reddit, a thread about generic vs. brand drugs got over 400 comments. Most people - 67% - reported no difference at all. But nearly 30% said they had issues, especially with levothyroxine. Some felt their energy dropped or their heart raced after switching. In many cases, those symptoms disappeared when they switched back.
Why? It’s not the active ingredient. It’s the fillers - the inactive ingredients that hold the pill together. Different manufacturers use different binders, dyes, or coatings. For most people, this doesn’t matter. But for someone with a rare sensitivity - say, to a specific dye or gluten filler - even a tiny change can cause side effects.
That’s why, if you notice a change after switching, talk to your pharmacist. They can check if the generic you got uses different fillers than the one you were on. Sometimes, switching to a different generic - not back to the brand - solves the problem.
What Pharmacists Know That You Don’t
Your pharmacist has access to the FDA’s Orange Book - a public database that lists every approved generic and its bioequivalence rating. Look for "AB-rated" drugs. That means the FDA has confirmed they’re therapeutically equivalent to the brand.
Some generics are rated "B" - meaning they’re approved, but there’s less certainty about how closely they match the brand. These aren’t bad drugs. But for NTI medications, pharmacists may avoid substituting them unless your doctor specifically approves it.
Most states allow pharmacists to substitute generics automatically unless the doctor writes "Dispense as Written" or "Do Not Substitute." That’s a good thing - it saves money. But if you’re on warfarin or levothyroxine, speak up. Ask for the brand or a specific generic. Keep the same one. And get your blood tested 7 to 14 days after any switch.
Why Do Brands Still Exist?
If generics are cheaper and just as effective, why do brand-name drugs still exist? Marketing. Drug companies spend billions on TV ads, doctor visits, and patient materials that make people believe the brand is better. One study found that 43% of patients think generics are less effective - even though the science says otherwise.
And it’s not just patients. A 2023 survey of doctors showed that while 78% knew warfarin needed monitoring after a switch, only 32% knew the same was true for levothyroxine. That’s a gap in knowledge - not in evidence.
What’s Next?
The future of generics is getting even better. New technology is making manufacturing more precise. A 2023 MIT study showed that with advanced analytics, bioequivalence variation for warfarin generics could be reduced to under 2% - nearly eliminating the concerns around NTI drugs.
At the same time, the FDA is fast-tracking approvals for complex generics - things like inhalers, creams, and injectables - which used to be harder to copy. In 2023, they approved 247 of them, up 19% from the year before.
But there’s a warning: drug shortages are rising. In 2023, there were 312 shortages of generic drugs, mostly sterile injectables. That’s not because generics are unstable - it’s because supply chains are fragile. When one factory in India or China has a problem, it can ripple across the country.
Still, the bottom line hasn’t changed. For over 90% of prescriptions, the generic is not just a cost-saving alternative - it’s the exact same medicine, proven by science, approved by the FDA, and used safely by millions every day.
What You Can Do Today
- If you’re on a brand-name drug, ask your pharmacist: "Is there a generic?"
- If you’re on warfarin, levothyroxine, phenytoin, or lithium, ask your doctor if you should stick with one version - brand or generic - and schedule a blood test after any switch.
- Use GoodRx or SingleCare to compare prices. Often, the generic is free with a coupon.
- If you notice a change in how you feel after switching, don’t assume the generic is broken. Talk to your pharmacist. It might be the filler, not the drug.
- Don’t let marketing scare you. The science is clear: generics work.
Are generic drugs as safe as brand-name drugs?
Yes. Generic drugs must meet the same FDA standards for safety, strength, quality, and performance as brand-name drugs. The active ingredient is identical, and the manufacturing facilities are inspected to the same standards. The FDA reports that generic medicines have the same risks and benefits as their brand-name counterparts.
Why do some people say generics don’t work for them?
Most of the time, it’s not the active ingredient - it’s the inactive ingredients, like fillers or dyes. A small number of people are sensitive to these, which can cause side effects like stomach upset or fatigue. Switching to a different generic - not back to the brand - often fixes the issue. If you notice a change after switching, talk to your pharmacist.
Can I switch from a brand-name drug to a generic without my doctor’s permission?
In most cases, yes. Pharmacists are allowed to substitute generics unless your doctor writes "Do Not Substitute" on the prescription. But for drugs with a narrow therapeutic index - like warfarin or levothyroxine - it’s best to talk to your doctor first. They may want to monitor your blood levels after the switch.
Do generic drugs take longer to work?
No. Bioequivalence testing ensures generics are absorbed into your bloodstream at the same rate and to the same extent as the brand. Any difference in how fast you feel relief is usually due to your body’s natural variation - not the drug itself.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to repeat expensive clinical trials. Once a brand-name drug’s patent expires, other companies can make the same drug by proving it’s bioequivalent - a much faster, cheaper process. They also face competition from multiple generic makers, which drives prices down.
Are all generics the same?
They all contain the same active ingredient and meet FDA bioequivalence standards. But different manufacturers use different inactive ingredients. That’s why, if you have a reaction to one generic, switching to another generic (not the brand) might help. The FDA’s Orange Book lists which generics are rated AB - meaning they’re considered interchangeable.
Final Thought
You don’t need to choose between saving money and getting good care. With generics, you get both. The science, the data, the real-world outcomes - they all point to the same conclusion. For most people, most of the time, the generic is the smart, safe, and effective choice. The only question left is: why are you still paying more?


Comments
Asia Roveda
Let me get this straight - you’re telling me I’ve been overpaying for years because some pharma execs convinced me their pill is ‘better’? 😑 I switched to generic levothyroxine last year and my heart started racing like I’d chugged three espressos. Turned out it was the dye. Not the drug. But now I’m paranoid every time my pharmacy switches it. Why do they even bother making different fillers if they’re just gonna mess with people’s nerves?
Micaela Yarman
It is imperative to underscore, with the utmost clarity, that the regulatory framework governing generic pharmaceuticals in the United States is among the most rigorous in the world. The Food and Drug Administration does not permit any deviation from bioequivalence standards, regardless of manufacturer or market pressure. To suggest otherwise is to undermine the integrity of public health infrastructure. The cost savings are not merely fiscal - they are moral.
Cynthia Springer
So if the active ingredient is identical, why do some generics make me feel like a zombie and others don’t? I’ve tried three different atorvastatin brands - two were fine, one made me so tired I napped through my kid’s soccer game. Is it the coating? The starch? The ghost of a factory worker’s lunch? I just want to know what’s actually in these things. Does the FDA publish filler lists?
Marissa Coratti
It is a profound and disturbing irony that in a nation that prides itself on scientific literacy and evidence-based decision-making, millions of citizens continue to be manipulated by corporate advertising campaigns that exploit psychological biases - particularly the false assumption that higher price equates to higher efficacy. The FDA’s bioequivalence criteria, which demand absorption profiles within 80–125% of the originator product, are not arbitrary thresholds - they are statistically validated benchmarks grounded in pharmacokinetic science. The fact that the average deviation is less than 4% is not a coincidence; it is the result of decades of methodological refinement. And yet, the myth persists - fueled not by data, but by brand loyalty cultivated through $10 billion annual marketing budgets. The real tragedy? Patients who could be saving hundreds - even thousands - per year are instead paying premiums for placebo branding. This isn’t healthcare. It’s consumer manipulation dressed in white coats.
Rachel Whip
For anyone worried about switching: if you’re on warfarin or levothyroxine, stick with one generic and don’t switch unless you have to. Keep a little notebook - write down the pill color, shape, and the name on it. If you feel weird after a refill, check if the pill looks different. Most pharmacies have a sheet that tells you which generic is which. And if you’re on GoodRx? You’re already saving. Don’t let fear cost you more than the drug itself.
Stephen Adeyanju
So let me get this straight I took my generic Lipitor and felt like a wet sock that got stepped on and now you’re telling me it’s not the drug it’s the filler and I’m supposed to just shrug and take another one because science says so WHAT ABOUT MY FEELINGS DO THEY NOT COUNT
Deborah Williams
It’s funny how we treat medicine like a luxury brand. ‘Oh, I only drink the organic, artisanal, hand-crafted version of my blood pressure pill.’ Meanwhile, the guy in India who made it is working 14-hour shifts in a facility that meets FDA standards. We’re not choosing between efficacy and cost - we’re choosing between ego and empathy. The real question isn’t ‘Is the generic the same?’ It’s ‘Why do we still believe the brand is better?’
mohit passi
bro the generics saved my dad's life 🙏 he was on Plavix for $400/month - now he pays $0 with GoodRx. no side effects. no drama. just a man who can afford to eat. 🇮🇳❤️