Graves' Disease Heart Risk Calculator
Your Heart Risk Assessment
- Graves' disease can speed up heart rate and raise blood pressure.
- Uncontrolled thyroid hormones increase the chance of atrial fibrillation and high cholesterol.
- Medication, beta‑blockers, and lifestyle tweaks lower those heart risks.
- Regular check‑ups-ECG, blood pressure, and lipid tests-catch problems early.
- Early prevention lets you enjoy a healthier heart while managing thyroid disease.
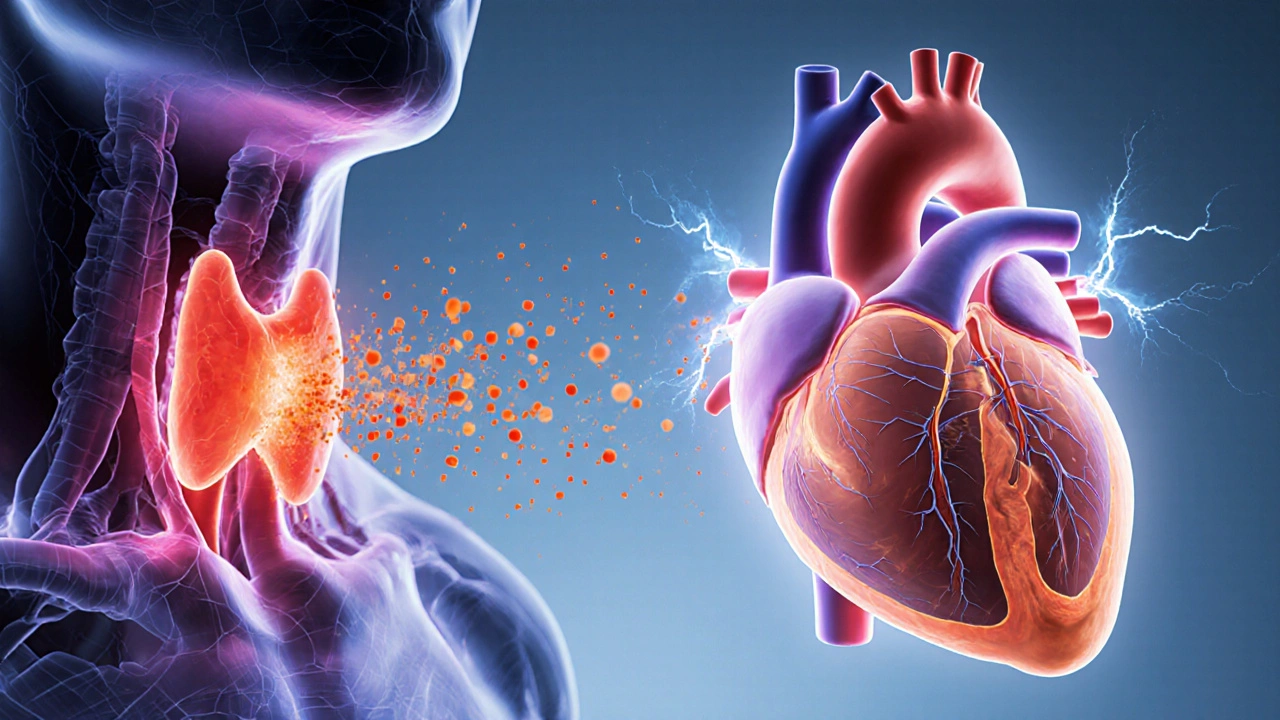
Graves' disease is a autoimmune disorder that forces the thyroid gland to produce excess hormones. This overactive thyroid, known medically as hyperthyroidism, sends a cascade of signals through the whole body, including the cardiovascular system. Understanding how these signals affect your heart and what you can do to protect it is the focus of this guide.
WhatisGraves' disease and why it matters for your heart
Graves' disease belongs to a family of thyroid conditions that cause the gland to release too much thyroxine (T4) and triiodothyronine (T3). The extra hormones crank up metabolism, which feels great at first-more energy, weight loss, a faster pulse-but the same surge also pushes the heart to work harder. Think of your heart as a car engine that suddenly gets more fuel than it can handle; the wear and tear add up quickly.
Key thyroid markers to watch are thyroid‑stimulating hormone (TSH), which drops when T3/T4 are high, and the actual hormone levels themselves. When your doctor says your TSH is "suppressed," that’s a red flag that the thyroid is overactive and that your cardiovascular system might be under stress.
How excess thyroid hormones strain the cardiovascular system
Thyroid hormones have a direct influence on several heart functions:
- Heart rate (chronotropism): T3 stimulates the sino‑atrial node, leading to tachycardia.
- Contractility (inotropism): More hormone means stronger heart muscle contractions, raising cardiac output.
- Vascular resistance: Hormones cause blood vessels to relax, which can paradoxically provoke reflex hypertension.
These changes increase the workload on the heart and set the stage for specific risks.
Major cardiovascular risks linked to Graves' disease
Below are the most common heart‑related complications observed in patients with uncontrolled Graves' disease.
- Atrial fibrillation - irregular, rapid beating that raises stroke risk.
- Hypertension - high blood pressure that can damage arteries over time.
- Elevated cholesterol - thyroid overdrive can alter lipid metabolism, leading to higher LDL.
- Heart failure - prolonged tachycardia and high output may eventually weaken the heart.
- Arrhythmias other than atrial fibrillation, such as premature ventricular contractions.
Medical strategies to reduce heart risk
First line of defense is getting thyroid hormone levels back to normal. Your endocrinologist may prescribe:
- Anti‑thyroid drugs (methimazole, propylthiouracil) to stop excess hormone production.
- Radioactive iodine therapy, which selectively destroys overactive thyroid cells.
- Thyroidectomy (surgical removal) in severe or refractory cases.
While you’re stabilizing the thyroid, doctors often add beta‑blockers (e.g., propranolol) to blunt the heart‑racing effects. These meds lower heart rate, reduce tremor, and mitigate anxiety, buying you time while the thyroid treatment takes effect.

Lifestyle and dietary tweaks that protect your heart
Even with medication, daily habits make a big difference.
- Exercise wisely: Aim for moderate aerobic activity-brisk walking, cycling, swimming-for 150 minutes a week. Avoid high‑intensity bursts that could trigger palpitations.
- Watch caffeine and alcohol: Both can amplify tachycardia and trigger atrial fibrillation episodes.
- Heart‑healthy diet: Emphasize omega‑3 fatty acids (salmon, walnuts), soluble fiber (oats, beans), and limit saturated fats. Keeping LDL low counters the cholesterol surge linked to thyroid excess.
- Stress management: Chronic stress raises cortisol, which interacts with thyroid hormones. Techniques like mindfulness, yoga, or simple breathing exercises help keep heart rhythm steady.
- Maintain a healthy weight: Sudden weight loss from uncontrolled hyperthyroidism can strain the heart; a balanced approach prevents extremes.
Monitoring your cardiovascular health
Regular check‑ups let you spot trouble before it escalates.
| Test | Frequency | Why it matters |
|---|---|---|
| ECG (electrocardiogram) | Every 6-12months | Detect atrial fibrillation or other arrhythmias early |
| Blood pressure measurement | At each endocrinology visit | Catch hypertension caused by hormone spikes |
| Lipid panel (cholesterol, LDL, HDL) | Annually or after thyroid normalization | Monitor cholesterol changes linked to thyroid levels |
| TSH, Free T4, Free T3 | Every 4-6weeks until stable, then every 6-12months | Ensure thyroid hormones stay within target range |
Ask your doctor to keep a log of any palpitations, dizziness, or chest discomfort. Even brief episodes can hint at developing atrial fibrillation.
When to seek urgent care
If you notice any of these warning signs, call emergency services or head to the nearest hospital:
- Sudden, severe chest pain.
- Persistent rapid heartbeat (>120bpm) that doesn’t settle with rest.
- Shortness of breath at rest.
- Fainting or near‑fainting spells.
- New onset of irregular pulse (fluttering or skipping beats).
These symptoms could signal a serious arrhythmia, heart attack, or heart failure that needs immediate attention.
Quick prevention checklist
- Keep thyroid hormone levels in the target range (regular labs).
- Take beta‑blockers as prescribed during the initial hyperthyroid phase.
- Schedule an ECG at least twice a year.
- Follow a Mediterranean‑style diet rich in omega‑3s and low in saturated fat.
- Limit caffeine to one cup of coffee daily.
- Exercise moderately and avoid extreme high‑intensity workouts until hormones stabilize.
- Practice stress‑relief techniques for at least 10minutes each day.
By pairing medical treatment with heart‑smart habits, you can keep both your thyroid and cardiovascular system in good shape. Remember, the goal isn’t just to control hormone numbers; it’s to stay active, feel well, and reduce long‑term heart risk.
Frequently Asked Questions
Can Graves' disease cause a heart attack?
Directly, Graves' disease doesn’t cause a heart attack, but the high heart rate, increased blood pressure, and altered cholesterol can accelerate atherosclerosis, which raises heart‑attack risk over time.
Is atrial fibrillation reversible after thyroid levels normalize?
In many patients, AFIB improves once TSH, T4, and T3 are stable, especially if caught early. However, prolonged episodes can cause structural changes that may require long‑term rhythm control medication.
Do I need a cardiologist if I’m already seeing an endocrinologist?
A joint approach works best. Your endocrinologist manages hormone levels, while a cardiologist can monitor heart rhythm, blood pressure, and lipid profile, ensuring nothing slips through the cracks.
Can lifestyle changes alone keep my heart safe while I’m on anti‑thyroid meds?
Lifestyle habits dramatically lower risk, but they complement-not replace-medical therapy. Hormone control is essential; diet and exercise fine‑tune the protection.
How often should I get my cholesterol checked?
Once your thyroid is stable, an annual lipid panel is typical. If you have additional risk factors-family history, hypertension, smoking-your doctor may suggest more frequent testing.


Comments
KaCee Weber
Hey everyone! 🌟 I just wanted to say how impressive this guide is for anyone dealing with Graves' disease. It breaks down the complex relationship between thyroid hormones and heart health in a way that anyone can grasp. The way you explained the effects on heart rate, contractility, and vascular resistance felt like a mini‑lecture that was still easy to follow. I love that you included both medical strategies and lifestyle tips, because we know both are essential for prevention. The section on beta‑blockers and how they can calm the racing heart was especially clear. Also, the reminder to monitor cholesterol and blood pressure really drives the point home about comprehensive care. The exercise recommendations are spot on; moderate aerobic activity is a safe sweet spot for most patients. I appreciate the warning about caffeine and alcohol, as these are easy triggers we often overlook. The checklist at the end is a fantastic quick‑reference for busy lives. 🙌 The use of a risk calculator tool also empowers readers to take an active role in understanding their own numbers. I think the visual cues and bullet points make the information digestible, even for those who aren’t medically trained. Your emphasis on regular check‑ups with both endocrinologists and cardiologists highlights a collaborative approach that saves lives. The FAQ section answered many lingering doubts I had, like whether atrial fibrillation can reverse after hormone normalization. Overall, the guide feels like a supportive companion rather than a dry medical pamphlet. Thank you for putting together such a thorough resource, and I hope it reaches everyone who needs it. 😊
jess belcher
Great guide Thanks for the clear breakdown of thyroid and heart risks.
Sriram K
Thank you for the comprehensive overview. It’s especially helpful to see the direct link between excess T3/T4 and increased cardiac output. Knowing that beta‑blockers can transiently control tachycardia gives patients a concrete option while awaiting thyroid normalization. I also appreciate the practical advice on exercise intensity and caffeine limits, as these are often the first lifestyle tweaks we can implement. Regular monitoring of ECG and lipid panels, as you suggested, can catch early changes before they become serious. Keep sharing such evidence‑based guidance; it really empowers the community.
Deborah Summerfelt
Honestly the risk calculator feels a bit overhyped. Most of us don’t have the time to input every little detail and still get a vague “moderate” label. Plus, the heart risk from Graves’ can vary wildly, so a one‑size‑fits‑all score seems simplistic. Still, the guide has some solid points.
Maud Pauwels
I appreciate the balanced tone of the article.
Scott Richardson
That’s nonsense we need real data not a guesswork tool.
Laurie Princiotto
Wow great advice 😒
Justin Atkins
Your exposition elegantly intertwines pathophysiology with pragmatic recommendations, rendering a complex endocrine‑cardiac nexus accessible to lay readers. By elucidating the mechanistic cascade-from heightened adrenergic stimulation to potential atrial fibrillation-you furnish a lucid scaffold upon which patients can build informed health strategies. The inclusion of both pharmacologic interventions, such as propranolol, and lifestyle modifications, notably the Mediterranean‑style diet, reflects a holistic ethos that is commendable. Moreover, the periodic surveillance schedule you propose-ECG semi‑annually, lipid panel annually-demonstrates a proactive stance against insidious cardiovascular sequelae. In sum, this guide serves as a paragon of patient‑centered education.
June Wx
Yo that’s some solid info you dropped. I’m gonna start walking more and cut back on coffee. Thanks for keeping it simple.
kristina b
In the grand theatre of human physiology, Graves’ disease assumes a role both tempestuous and consequential, orchestrating a symphony of hormonal excess that reverberates through the cardiovascular arena. The hyperthyroid surge, akin to an unbridled conductor, accelerates the heart’s rhythm, compelling the sino‑atrial node to beat with relentless vigor. This tachycardic overture, while initially perceived as a mere flourish of vitality, swiftly devolves into a perilous cadence that may precipitate atrial fibrillation, a discordant arrhythmia with grave implications. Moreover, the augmented contractility and stroke volume imposed upon the myocardium elevate cardiac output, engendering a state of hyperdynamic circulation that can erode myocardial reserves over time. Concurrently, the vasodilatory influence of excess thyroid hormones paradoxically triggers reflexive hypertension, further straining arterial walls and fostering a milieu conducive to atherosclerotic progression. The cumulative effect of these intertwined mechanisms is a heightened vulnerability to myocardial infarction, heart failure, and cerebrovascular accidents. Yet, within this narrative of risk lies a chorus of hope, as evidenced by the therapeutic interventions delineated herein. Antithyroid agents, radioactive iodine, and surgical thyroidectomy each offer a pathway to reestablish hormonal equilibrium, thereby attenuating the cardiovascular onslaught. Beta‑blockers, serving as pharmacologic saboteurs, temper the tachycardic surge, granting the heart a respite from relentless pacing. Lifestyle modifications, embodied in moderated caffeine consumption, regular aerobic exercise, and a diet rich in omega‑3 fatty acids, further consolidate cardiac resilience. The vigilant monitoring regimen-periodic ECGs, lipid panels, and blood pressure assessments-functions as an early warning system, detecting subclinical derangements before they burgeon into overt disease. In essence, this comprehensive guide does not merely catalogue risks; it furnishes an actionable blueprint for preservation of cardiac health amidst the turbulence of Graves’ disease. By embracing both medical and behavioral strategies, patients can navigate the storm with confidence, securing a future where the heart beats in harmonious balance.
Ida Sakina
The exposition you have presented stands as a testament to the moral imperative of informed self‑care. It is incumbent upon each individual to heed the cautionary insights regarding cardiac jeopardy and to act with prudence. Neglecting such knowledge would be a dereliction of one’s duty to oneself and to those who depend upon us. Therefore, I commend the emphasis on proactive monitoring and disciplined lifestyle alteration. Let us all resolve to uphold these principles with unwavering dedication.
Amreesh Tyagi
Honestly I think all this hype is just fear‑mongering.
Brianna Valido
Love the uplifting spirit 🙏 Let’s all stay positive and follow the guidance 🌟
Caitlin Downing
Wow This guid is like a total lifesaver but also a bit hefty tho its full of good tipz and blink everyon must read it