Halobetasol Safe Usage Calculator
Usage Guidelines
Halobetasol is a super-potent topical corticosteroid recommended for short-term use only. Based on clinical guidelines, usage should not exceed 2 weeks per treatment period to minimize the risk of side effects such as skin thinning and HPA-axis suppression.
Safety Assessment
Enter your body surface area and condition type to see safety recommendations.
Key Takeaways
- Halobetasol is a super‑potent topical corticosteroid used for several inflammatory skin disorders.
- It acts by binding the glucocorticoid receptor, suppressing cytokine production and immune cell activation.
- Recommended for short‑term use on plaque psoriasis, severe eczema, and lichen planus, but not for large‑area or long‑duration therapy.
- Adverse effects include skin thinning, HPA‑axis suppression, and increased infection risk; monitoring is essential.
- Compared with clobetasol propionate and betamethasone dipropionate, halobetasol offers the highest anti‑inflammatory potency with a slightly different safety profile.
What Is Halobetasol?
Halobetasol propionate is a synthetic glucocorticoid approved for topical use in concentrations of 0.05% (cream, ointment, lotion) and 0.01% (shampoo). It belongs to the class of super‑potent corticosteroids (class I in the US potency scale).
The drug was first FDA‑approved in 2009 for short‑term management of plaque psoriasis and later gained indication for severe atopic dermatitis and lichen planus. Its high affinity for skin → strong anti‑inflammatory effect makes it a go‑to option when milder steroids fail.
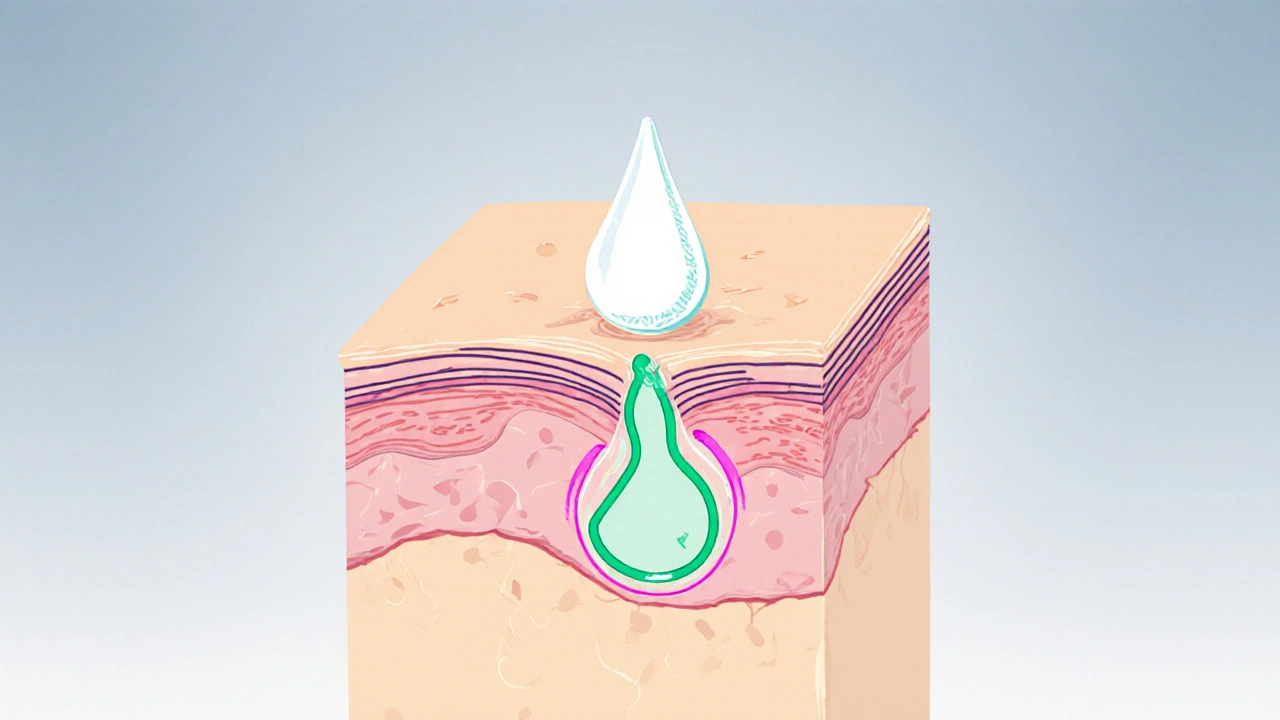
How Halobetasol Works: The Mechanism
When applied, halobetasol penetrates the epidermis and binds to the intracellular glucocorticoid receptor. This receptor‑ligand complex translocates to the nucleus and regulates gene transcription:
- It up‑regulates anti‑inflammatory proteins such as annexin‑1.
- It down‑regulates pro‑inflammatory cytokines (IL‑1, IL‑6, TNF‑α) and chemokines.
- It reduces leukocyte migration and dampens T‑cell activation.
The net result is rapid reduction of erythema, scaling, and itching-often noticeable within 48‑72 hours.
Topical Steroid Potency Classification
In the United States, topical corticosteroids are grouped into seven classes, with Class I being the most potent. Halobetasol sits at the top of this scale, alongside clobetasol propionate and fluocinonide. The potency is driven by three factors:
- High receptor affinity.
- Low molecular weight enabling deeper skin penetration.
- Formulation vehicle (ointment > cream > lotion for maximal delivery).
Understanding potency helps clinicians balance efficacy against the risk of adverse effects.
Which Dermatoses Respond to Halobetasol?
Halobetasol is indicated for “corticosteroid‑responsive dermatoses,” a term covering skin diseases that improve with anti‑inflammatory steroids. The most common indications include:
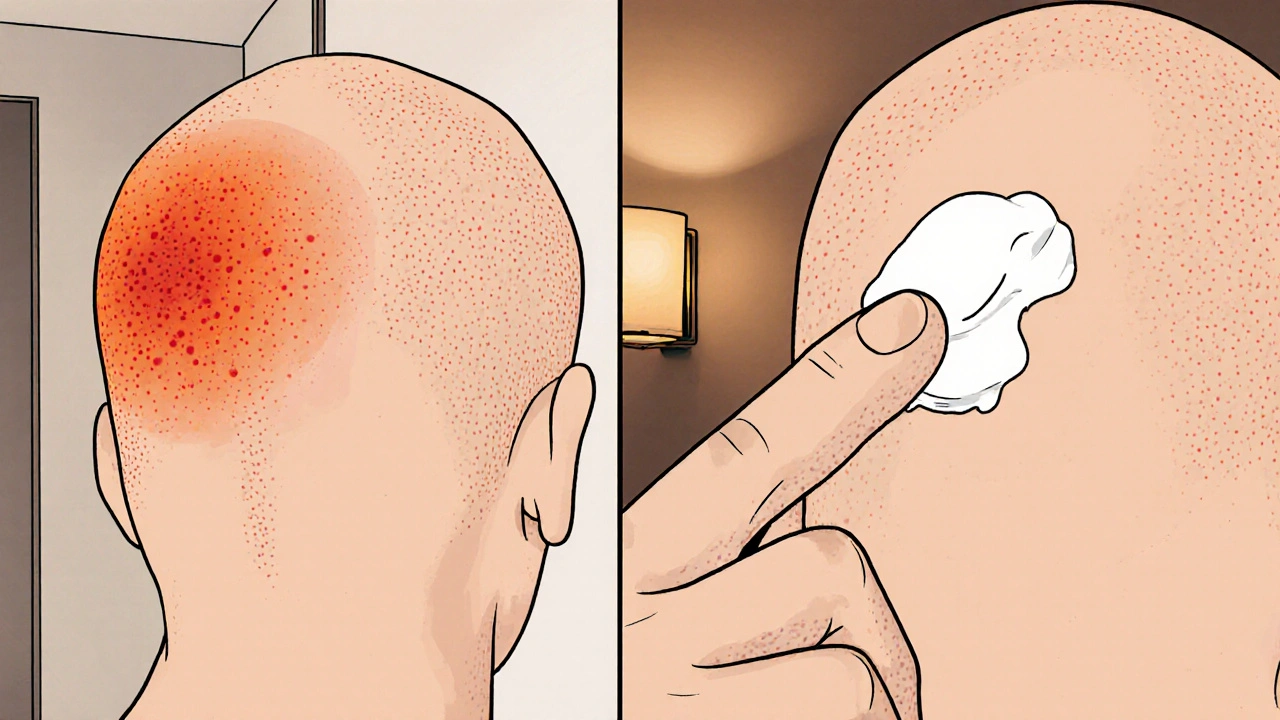
- Plaque psoriasis - especially thick, recalcitrant plaques on the scalp or extremities.
- Severe atopic dermatitis (eczema) - when acute flares affect limited body surface area.
- Lichen planus - erosive or hypertrophic variants that resist milder steroids.
- Discoid lupus erythematosus - for short bursts to control inflammation.
Clinical guidelines (American Academy of Dermatology, 2023) recommend reserving halobetasol for cases where first‑line Class III‑V steroids have failed.
Halobetasol vs. Other Super‑Potent Steroids
| Attribute | Halobetasol | Clobetasol Propionate | Betamethasone Dipropionate |
|---|---|---|---|
| Potency (US class) | Class I (Super‑potent) | Class I (Super‑potent) | Class II (Potent) |
| Typical concentration | 0.05% cream/ointment | 0.05% cream/ointment | 0.05% cream/ointment |
| Approved indications | Psoriasis, severe eczema, lichen planus | Psoriasis, eczema, alopecia areata | Psoriasis, eczema, allergic contact dermatitis |
| Typical duration of use | ≤ 2 weeks (intermittent) | ≤ 2 weeks (intermittent) | ≤ 4 weeks (continuous) |
| Risk of HPA‑axis suppression | Higher (due to potency) | Higher | Moderate |
The table shows that halobetasol and clobetasol share the same potency, but halobetasol’s newer formulation provides a smoother vehicle, making it slightly better tolerated on the face and intertriginous areas.
Safety Profile and Adverse Effects
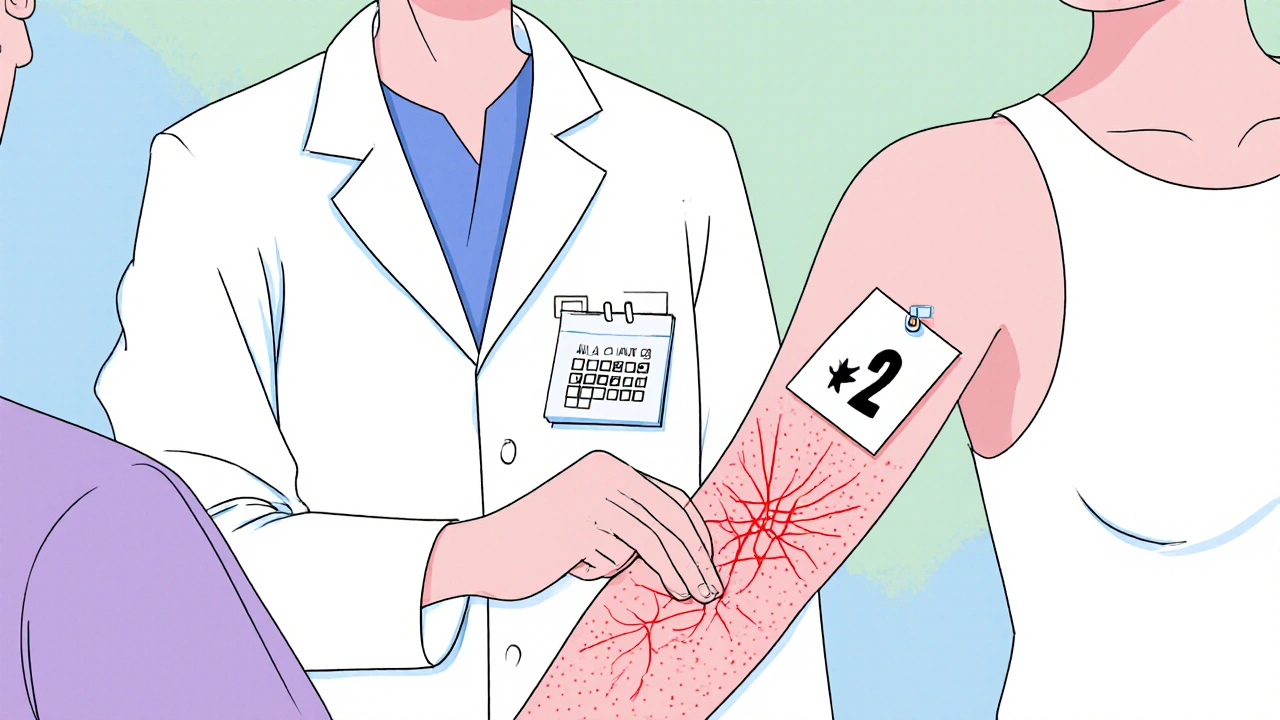
Because of its strength, halobetasol carries a higher potential for side effects, especially when used over large areas or for prolonged periods. Common adverse events:
- Skin atrophy - thinning of the epidermis and dermis, visible as translucency.
- Telangiectasia - small dilated blood vessels causing red patches.
- Striae - stretch marks, especially on flexural zones.
- Perioral dermatitis - papular rash around the mouth.
- Systemic effects - rare HPA‑axis suppression leading to cortisol deficiency.
Risk mitigation strategies include:
- Limiting treatment to ≤ 2 weeks per lesion.
- Using the lowest‑effective formulation (cream vs. ointment).
- Avoiding occlusion unless specifically prescribed.
- Monitoring for skin thinning with periodic photographs.
Pregnant or breastfeeding patients should only use halobetasol when the benefit outweighs potential fetal risk; the drug is classified as FDA Pregnancy Category C.
Practical Usage Tips
Effective and safe application hinges on a few simple steps:
- Clean the area - gentle cleansing with a pH‑balanced cleanser, pat dry.
- Apply a thin layer - a pea‑size amount for a palm‑sized area is enough; rub in until fully absorbed.
- Frequency - usually once daily in the evening to reduce sun‑induced irritation.
- Follow‑up - re‑evaluate after 7‑10 days; if minimal improvement, consider stepping down to a lower‑potency steroid.
- Adjunct care - moisturize after the steroid wears off to restore barrier function.
Patients should be warned not to use on the face, genitals, or broken skin unless a dermatologist explicitly directs it.
Frequently Asked Questions
Can I use halobetasol on my scalp?
Is halobetasol safe for scalp psoriasis?
Yes, a 0.05% ointment or cream is often the first‑line choice for thick scalp plaques. Apply a small amount, massage in, and wash hair after 30 minutes to avoid excessive absorption.
How long does it take to see results?
When will the rash start to improve?
Most patients notice reduced redness and itching within 2-3 days, with visible plaque flattening by the end of the first week.
What should I do if I develop skin thinning?
Is skin atrophy reversible?
Early atrophy can improve after discontinuation and switching to a lower‑potency steroid plus barrier‑repair moisturizers. Persistent thinning may require topical retinoids or professional laser therapy.
Can children use halobetasol?
Is it safe for pediatric patients?
Guidelines limit use in children under 12 to short courses (≤ 1 week) for localized severe eczema or psoriasis, due to higher surface‑area‑to‑body‑mass ratio.
Do I need a prescription?
Is halobetasol available over the counter?
No. In the United States and most other countries, halobetasol is a prescription‑only medication because of its potency.
Understanding the pharmacology, potency, and safety considerations of halobetasol equips clinicians and patients to use this powerful tool responsibly. When applied correctly, it can provide rapid relief for stubborn, corticosteroid‑responsive dermatoses while keeping risks at a manageable level.


Comments
Brian Van Horne
Halobetasol exemplifies a super‑potent corticosteroid, delivering rapid anti‑inflammatory effects while demanding judicious use. Its mechanism hinges on glucocorticoid receptor binding, swiftly curbing cytokine cascades.
Norman Adams
Oh, thank heavens you’ve elucidated the mechanism-without your scintillating exposition we’d all be lost in the abyss of epidermal ignorance.
Really, the world needed another dissertation on steroid pharmacology.
Margaret pope
You’re on the right track remember to limit use to two weeks and monitor skin thickness for safety
James Mali
Seems like another overhyped steroid to me.
Matthew Miller
Whoa! That’s the kind of punch you need when eczema refuses to quit-just remember to taper down! A short burst can bring relief without the dreaded side‑effects.
Alex Lineses
From a pharmacodynamic standpoint, halobetasol exhibits a high glucocorticoid receptor affinity, resulting in up‑regulation of annexin‑1 and down‑regulation of IL‑1, IL‑6, and TNF‑α.
The vehicle matrix-ointment versus cream-modulates percutaneous absorption, with the ointment providing a higher occlusive effect.
Moreover, the drug’s low molecular weight facilitates dermal penetration, enhancing its class I potency.
Clinical guidelines advise intermittent application-typically 5‑7 days-followed by a steroid‑sparing regimen.
Vigilance for HPA‑axis suppression remains paramount, especially in pediatric cohorts.
kendra mukhia
When I first laid eyes on that glossy paper about halobetasol, I was instantly blinded by the hubris of pharmaceutical marketing. They parade it as the holy grail for stubborn plaques, as if a single cream could magically erase years of dermatological misery. But let us not ignore the dark underbelly-the insidious skin atrophy that creeps in like a silent assassin. Patients, dazzled by promises of rapid flattening, often forget that tomorrow’s mirror may reveal translucent skin and telangiectasia. The tables of potency are nothing more than a vanity metric, a badge of honor for manufacturers, not a guarantee of safety. Clinical guidelines caution us to restrict use to no more than two weeks, yet the advertising copy suggests endless application. Meanwhile, the HPA‑axis suppression looms like an unseen cliff, ready to plunge unsuspecting users into adrenal crisis. And who will bear the burden of monitoring? Too many clinicians dismiss the need for periodic photos, leaving patients in the dark. Even the so‑called “gentle” vehicle-cream versus ointment-is a gamble, as the former may increase percutaneous absorption on compromised barrier. In pediatric hands, the stakes rise exponentially; a child’s surface‑area‑to‑body‑mass ratio turns a modest dose into a systemic overdose. Pregnant women are warned with vague Category C language, a euphemism for “we’re not sure, proceed at your own risk.” The truth is, halobetasol is a double‑edged sword: it slices through inflammation but can also carve away the very fabric of skin. If you’re not vigilant, the aftermath may demand laser resurfacing or retinoid therapy-another round of costly interventions. So before you anoint your lesions with this potent potion, ask yourself whether you’re chasing a quick fix or committing to a responsible treatment plan. Remember, the skin is a living organ, not a battlefield to be conquered with indiscriminate force. In the end, mastery of any steroid lies in restraint, patience, and the humility to admit that sometimes less truly is more.
Bethany Torkelson
Enough with the sugar‑coated hype; if you’re not monitoring for atrophy you’re courting disaster.
Take responsibility for your patients’ skin integrity.
Grace Hada
You sound like a cautionary tale, not a prescription guide.
Trim the drama and stick to the facts.
Rohit Sridhar
Hey, I get the frustration-steroids can feel like a gamble, but with a clear plan they become allies.
Start with a pea‑size amount, reassess after a week, and if the plaque is still stubborn, consider stepping down to a mid‑potency option.
Most importantly, keep the dialogue open with your dermatologist; they can fine‑tune the schedule to avoid systemic fallout.
Stay positive, progress is usually visible within a few days when you stick to the protocol.