
Most people think a bad cough means they need antibiotics. But if you’ve been sick for a few days with a nagging cough, runny nose, and maybe a low-grade fever, you’re probably dealing with acute bronchitis-and antibiotics won’t fix it. In fact, taking them could do more harm than good.
What Exactly Is Acute Bronchitis?
Acute bronchitis is a short-term inflammation of the bronchial tubes-the airways that carry air to your lungs. It’s almost always caused by a virus, the same ones that give you colds and the flu. You don’t need a lab test to diagnose it. Doctors look for a cough lasting less than three weeks, often with mucus, and no signs of pneumonia like high fever, rapid breathing, or chest pain.
It’s incredibly common. About 5% of U.S. adults get it every year. That’s roughly 10 million doctor visits annually, mostly because of coughing. The cough can be brutal. Half of people are still coughing after 10 days. One in four still has it after two weeks. And 1 in 10 are coughing at three weeks. That’s not unusual. That’s normal.
Why Antibiotics Don’t Work (and Why They’re Dangerous)
Ninety to ninety-five percent of acute bronchitis cases are viral. Antibiotics kill bacteria. They don’t touch viruses. That’s basic biology. But despite this, doctors still prescribe antibiotics for bronchitis in more than half of cases.
Why? Because patients expect them. And doctors feel pressured to give something-even if it doesn’t help. But here’s what the science says: antibiotics reduce cough duration by less than a day. A Cochrane review of nearly 6,000 patients found a reduction of just 0.6 days. That’s less than 15 hours. For that tiny benefit, you risk side effects like diarrhea, nausea, or yeast infections. One in 14 people who take antibiotics for bronchitis will have an adverse reaction.
And the bigger problem? Antibiotic resistance. Every unnecessary antibiotic prescription adds to the global crisis. The CDC estimates 46 million unnecessary antibiotic prescriptions are given for respiratory infections like bronchitis every year in the U.S. That’s fueling superbugs that kill 35,000 Americans annually. When you take an antibiotic you don’t need, you’re not just risking your own health-you’re making it harder to treat infections in your family, your community, and future generations.
What Actually Helps? Evidence-Based Cough Care
Since antibiotics don’t work, the goal is simple: manage symptoms and wait it out. Your body will clear the virus on its own. Here’s what works, backed by real studies.
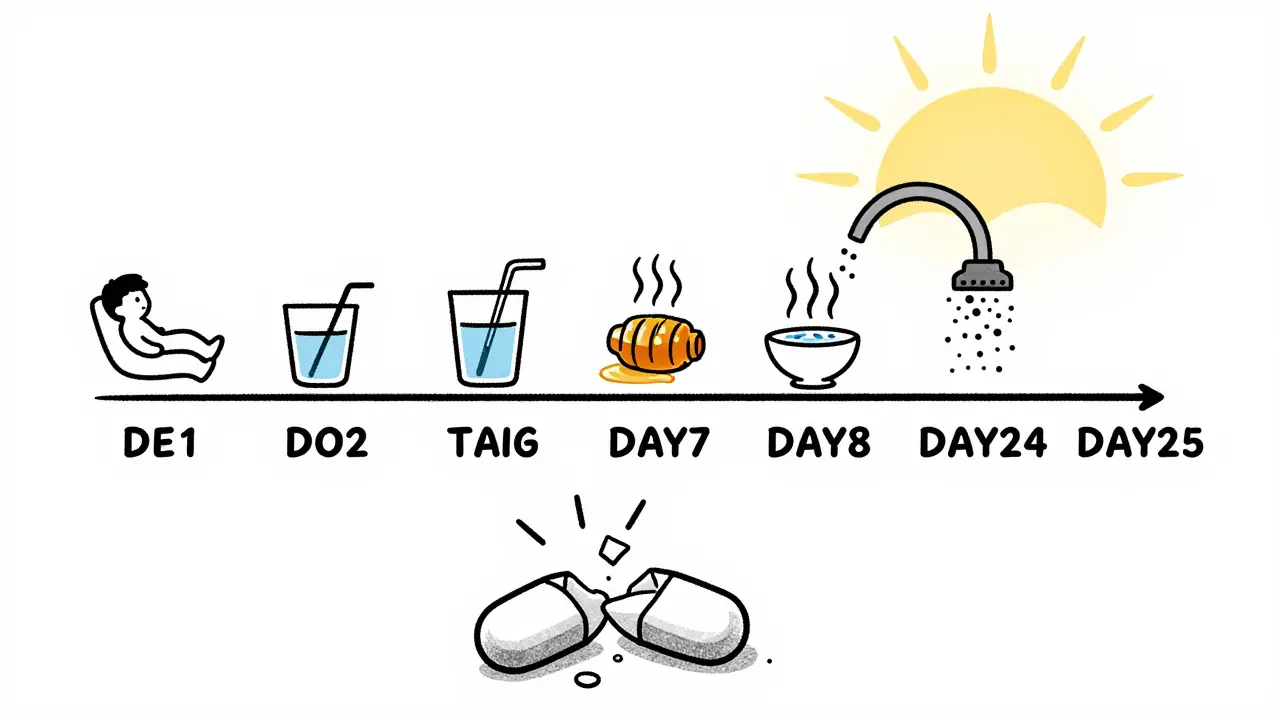
Hydration and Rest
Drink plenty of fluids-water, broth, tea. Staying hydrated helps thin mucus so it’s easier to cough up. Aim for 8 to 10 glasses a day. Rest is just as important. Your immune system needs energy to fight the virus. Skip the gym, cancel the plans, and let your body heal.
Honey
Honey is one of the best cough remedies you’ve probably never tried. A 2018 study in JAMA Pediatrics found honey worked as well as dextromethorphan (a common cough suppressant) for children with upper respiratory infections-and better than no treatment at all. For adults, 1 to 2 teaspoons of honey before bed can reduce nighttime coughing and improve sleep. Just don’t give it to kids under 1 year old. Honey can carry spores that cause infant botulism, a rare but serious condition.
Dextromethorphan
If you need to suppress a dry, hacking cough, dextromethorphan (found in Robitussin DM, Delsym) is an option. Studies show it reduces cough frequency modestly. The standard dose is 15-30 mg every 6-8 hours, not to exceed 120 mg in 24 hours. It won’t make your cough disappear overnight, but it can make it less disruptive.
Guaifenesin
This expectorant (in Mucinex) is supposed to loosen mucus. But the evidence is mixed. Some studies show a small benefit. Others show nothing. If you want to try it, go for the extended-release version. Drink water with it-it helps the medication work.
Humidifiers and Steam
Moist air soothes irritated airways. Use a cool-mist humidifier in your bedroom at night. Or take a hot shower and breathe in the steam. Just be careful not to burn yourself. Don’t use hot water bowls unless you’re sitting far enough away to avoid steam burns.
Pain and Fever Relief
If you have a sore throat, headache, or low fever, use ibuprofen (Advil, Motrin) or acetaminophen (Tylenol). Stick to the recommended doses: no more than 3,000 mg of acetaminophen per day for adults. Don’t mix pain relievers with cold medicines-many already contain acetaminophen. Double-dosing can cause liver damage.
What Doesn’t Work (and What to Avoid)
There’s a lot of misinformation out there. Here’s what science says doesn’t help-and can hurt.
- Antibiotics: Not for viral bronchitis. Period.
- Inhaled bronchodilators (like albuterol): Only help if you’re wheezing. For most people with bronchitis, they do nothing and can cause shakiness, rapid heartbeat, or anxiety.
- Codeine or hydrocodone cough syrups: The FDA banned these for children under 12 in 2018. Even for adults, they’re overkill and carry addiction risk.
- Over-the-counter cold medicines for kids under 4: The FDA warns against them. They don’t work and can be dangerous.
- Herbal supplements like echinacea or elderberry: No strong evidence they help with bronchitis. Save your money.
When Should You Worry? Signs It’s Not Just Bronchitis
Most cases of acute bronchitis are harmless. But sometimes, it’s something worse. See a doctor if you have:
- Fever over 100.4°F (38°C) that lasts more than a few days
- Coughing up blood or thick, dark mucus
- Shortness of breath or chest pain when breathing
- Cough lasting longer than 3 weeks
- Wheezing or a history of asthma, COPD, or heart disease
These could signal pneumonia, asthma flare-up, or even heart failure. Don’t wait. Get checked.
How to Talk to Your Doctor About Antibiotics
If your doctor offers an antibiotic, you have the right to ask questions. Try saying:
- “Is this likely viral or bacterial?”
- “What are the risks of taking an antibiotic if it’s not needed?”
- “Can we wait a few days and see if it gets better on its own?”
Many doctors now use “delayed prescriptions.” They give you a script for antibiotics but tell you to fill it only if you’re not better in 48-72 hours. This reduces antibiotic use without making patients feel ignored.
It’s also okay to say: “I’d rather not take antibiotics unless absolutely necessary.” Most doctors respect that.
What’s Changing in Treatment Guidelines
Doctors are finally catching up. The American Academy of Family Physicians, the CDC, and the American College of Chest Physicians all agree: don’t prescribe antibiotics for acute bronchitis. New guidelines focus on communication, not pills.
One big shift? Setting expectations. Patients think a cough should last 3-5 days. The truth? It can last 2-3 weeks. When doctors explain this upfront, patients are far less likely to demand antibiotics. A 2021 study showed using a simple 5-question tool to discuss expectations cut antibiotic requests by 32%.
Future research is looking at natural options like ivy leaf extract, which early trials suggest might help reduce cough. But for now, the best treatment remains: time, hydration, honey, and patience.
Bottom Line: You Don’t Need Antibiotics
Acute bronchitis is annoying. It’s exhausting. But it’s not dangerous for most people. Antibiotics won’t make you feel better faster. They’ll just add side effects and contribute to a growing public health crisis.
Focus on what actually works: rest, fluids, honey, and time. Let your body heal. If your cough drags on past three weeks, or you develop new symptoms, see your doctor. But don’t rush to the pharmacy for antibiotics. Your cough isn’t broken. It’s just running its course.


Write a comment