
Stress-Related Infection Risk Calculator
Ever wonder why a bad day can end with an upset stomach or a pesky yeast infection? The link isn’t magic - it’s biology. Emotional Stress is a psychological response that activates hormonal and nervous system pathways, reshaping how our bodies defend against microbes. When those pathways go haywire, the gut and the vagina - two ecosystems that rely on delicate microbial balance - become vulnerable. Below we unpack the science, show how the two sites differ, and give you practical ways to keep stress from turning into infection.
Key Takeaways
- Stress spikes cortisol, which weakens immune surveillance in the gut and vagina.
- Dysbiosis - the loss of healthy microbes - is the main bridge between stress and infection.
- Intestinal infections often present as diarrhea, abdominal pain, or bloating, while vaginal infections show itching, discharge, or burning.
- Targeted diet, sleep, and stress‑reduction techniques can restore microbial balance.
- Seek medical care if symptoms persist longer than a week or are accompanied by fever.
How Emotional Stress Impacts the Body
When you feel anxious or overwhelmed, the hypothalamic‑pituitary‑adrenal (HPA) axis fires up. The adrenal glands release Cortisol a steroid hormone that helps mobilize energy but also suppresses immune function when chronically elevated. At the same time, the sympathetic nervous system pumps adrenaline, tightening gut muscles and altering blood flow. These changes are adaptive for short‑term threats but become harmful if they linger.
Two critical outcomes follow:
- Immune System damping - white blood cells become less efficient at spotting and destroying pathogens.
- Microbial environment shifts - beneficial bacteria lose ground to opportunistic species, a state known as Dysbiosis an imbalance in the body's microbial communities that can trigger inflammation and infection.
Stress and the Gut: From Cortisol to Intestinal Infection
The Gut Microbiome trillions of bacteria, viruses, and fungi living in the digestive tract that aid digestion, produce vitamins, and train the immune system is especially sensitive to stress hormones. Cortisol can thin the protective mucus lining, letting harmful bacteria like Clostridioides difficile or pathogenic Escherichia coli attach to intestinal cells.
Research from the University of Melbourne (2023) showed that students experiencing exam‑related stress had a 30% increase in gut permeability and a 2‑fold rise in opportunistic bacterial counts. The result? More frequent episodes of Intestinal Infection an invasion of the gastrointestinal tract by harmful microbes, leading to symptoms like diarrhea, cramping, and fever.
Common stress‑linked intestinal infections include:
- Travelers’ diarrhea caused by Enterotoxigenic E. coli
- Clostridioides difficile infection, often following antibiotic use and stress‑induced dysbiosis
- Viral gastroenteritis, where a weakened immune response lets norovirus linger longer
People with pre‑existing conditions such as Irritable Bowel Syndrome a functional gastrointestinal disorder marked by abdominal pain and altered bowel habits are especially prone; stress can trigger flare‑ups that mimic infection, making diagnosis tricky.
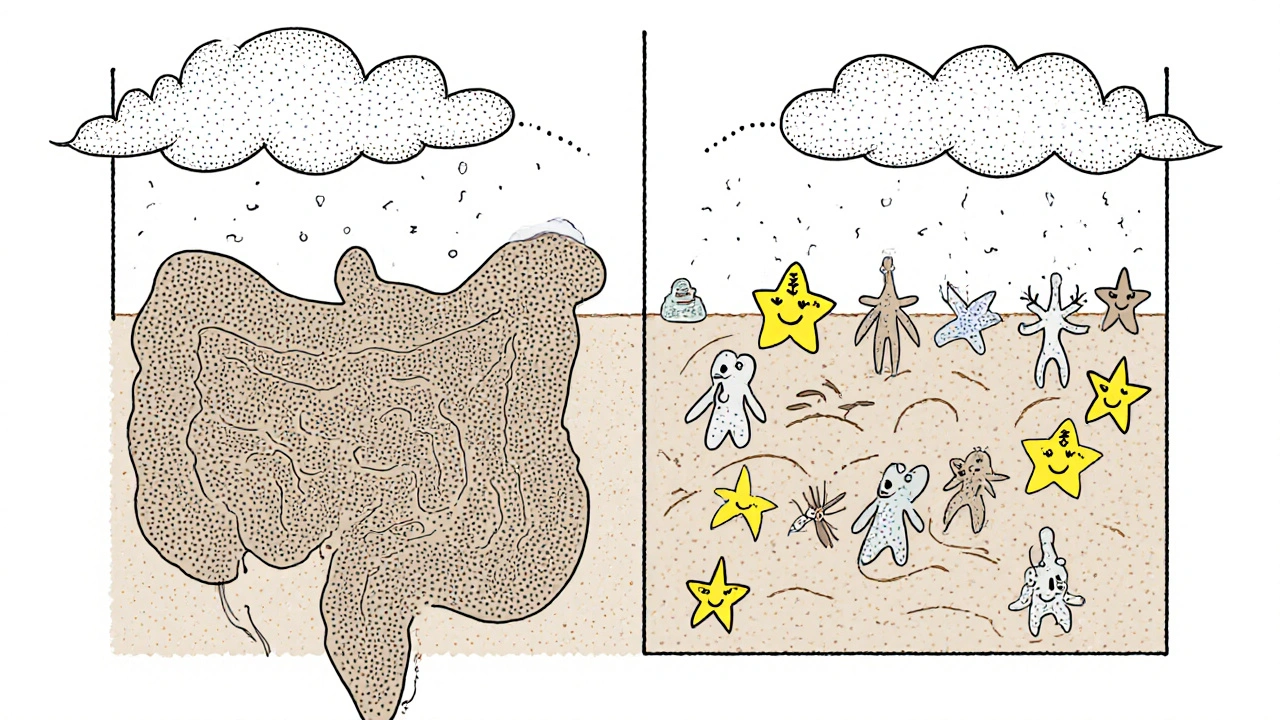
Stress and the Vagina: Hormones Meet the Vaginal Microbiome
The Vaginal Microbiome a community dominated by Lactobacillus species that maintains an acidic pH (≈3.5-4.5) to keep pathogens at bay reacts to cortisol much like the gut does. Elevated stress hormones can lower estrogen levels, which reduces glycogen production - the food source for Lactobacilli. Without enough Lactobacilli, the pH rises, opening the door for Bacterial Vaginosis an overgrowth of anaerobic bacteria that causes a fishy odor and discharge or Candidiasis a yeast infection caused by over-proliferation of Candida species, leading to itching and burning.
A 2022 Dutch cohort study found that women scoring high on the Perceived Stress Scale were 1.8 times more likely to develop bacterial vaginosis over a 12‑month period. The mechanism: stress‑induced cortisol suppresses local immunity, while the shift in hormone balance alters the vaginal environment.
Typical stress‑related vaginal infection signs:
- Thin, grayish discharge with a fishy smell (BV)
- Thick, white "cottage‑cheese" discharge, itching, and redness (yeast infection)
- Burning during urination or intercourse
Side‑by‑Side: Intestinal vs. Vaginal Infections Under Stress
| Aspect | Intestinal Infection | Vaginal Infection |
|---|---|---|
| Primary microbiome | Gut Microbiome (Bacteroidetes, Firmicutes) | Vaginal Microbiome (Lactobacillus spp.) |
| Stress hormone impact | Cortisol thins mucus, increases permeability | Cortisol lowers estrogen → less glycogen for Lactobacilli |
| Typical pathogens | Clostridioides difficile, pathogenic E. coli, norovirus | Gardnerella vaginalis (BV), Candida albicans (yeast) |
| Common symptoms | Diarrhea, abdominal cramping, fever | Discharge, itching, burning, odor |
| Diagnostic tests | Stool culture, PCR for C. difficile toxin | Microscopy (wet mount), pH test, DNA probe |
Practical Steps to Shield Your Microbiomes
Knowing the science helps, but day‑to‑day habits are the real hero. Here are evidence‑backed moves you can adopt right now:
- Mind‑body techniques. A 10‑minute daily meditation lowers cortisol by up to 20% (Harvard Health, 2024). Apps like Insight Timer or simple breathing exercises work.
- Sleep hygiene. Aim for 7‑9 hours; poor sleep spikes cortisol and impairs gut barrier function.
- Fiber‑rich diet. Soluble fiber (oats, apples, legumes) feeds beneficial gut bacteria and indirectly supports vaginal health by stabilizing blood glucose.
- Targeted probiotics. Strains such as Lactobacillus rhamnosus GR‑1 and L. reuteri RC‑14 have clinical data for preventing recurrent bacterial vaginosis. For gut health, Bifidobacterium infantis and Lactobacillus plantarum are solid choices.
- Limit refined sugar. High sugar feeds Candida and disrupts gut bacteria, amplifying stress‑related dysbiosis.
- Stay hydrated. Adequate water maintains mucus barrier integrity in both the intestines and vagina.
If you’re already battling an infection, short‑term antibiotics (for bacterial gut infections) or antifungals (for yeast) are necessary, but pair them with probiotics to avoid a secondary imbalance.
When to Seek Medical Help
Stress can mask or mimic infection, so keep an eye on red flags:
- Fever over 38°C (100.4°F) lasting more than 24 hours
- Blood in stool or persistent watery diarrhea (>3 days)
- Severe abdominal pain that doesn’t improve with over‑the‑counter meds
- Vaginal discharge with a strong odor, itching, or pain during sex that lasts beyond a week
- Recurring infections (≥3 episodes in a year) - may signal underlying chronic dysbiosis
Early intervention prevents complications like dehydration, pelvic inflammatory disease, or chronic gut inflammation.
Quick Checklist for Stress‑Related Infection Prevention
- Track stress levels daily (journal or app)
- Schedule at least one relaxation activity per day
- Eat 5‑7 servings of fiber‑rich foods weekly
- Take a probiotic containing Lactobacillus strains if you’ve had a vaginal infection before
- Consult a doctor if symptoms linger more than 7 days
Frequently Asked Questions
Can stress cause a gut infection without any bacteria?
Stress alone doesn’t create pathogens, but it weakens the gut barrier and immune response, making it easier for existing microbes to overgrow and cause infection.
Why do some women get yeast infections during stressful periods?
Stress lowers estrogen, which reduces glycogen in vaginal cells. Less glycogen means fewer food sources for good Lactobacilli, allowing Candida to multiply.
Are probiotics enough to fix stress‑induced dysbiosis?
Probiotics help, but they work best alongside diet, sleep, and stress‑reduction practices. A holistic approach restores balance more reliably.
How long does it take for the gut to recover after a stressful episode?
Recovery varies; with good nutrition and low stress, the gut microbiome can rebound in 2‑4 weeks. Persistent high stress may take months.
Should I see a gastroenterologist or a gynecologist first?
Start with the specialist whose symptoms are most prominent. If you have both gut and vaginal issues, a coordinated approach between both doctors works best.


Comments
Bethany Torkelson
Stress is the silent assassin that wrecks your gut and down there. Stop ignoring it and start taking control.
Rohit Sridhar
Thanks for sharing this solid breakdown. It's amazing how stress flips our hormones and opens the door for infections. By adding a quick 10‑minute breathing routine you can blunt that cortisol surge. Pair it with a fiber‑rich snack and you give the good microbes a fighting chance. Keep experimenting, everyone-your body will thank you.
Sarah Hanson
While the mechanisms are complex, the core message remains clear: manage stress to protect your microbiome. Consider daily probiotic supplementation and adequate rest. It’s definatly worth the effort.
kendra mukhia
You think stress is just a fleeting feeling? It is a physiological tyrant that hijacks your HPA axis and saps immune vigilance. When cortisol floods the bloodstream, it thins the intestinal mucus and deprives Lactobacilli of their glycogen feast. This double‑edged assault opens the door for Clostridioides difficile in the gut and Gardnerella in the vagina. Moreover, chronic anxiety rewires neural pathways, reinforcing a feedback loop that perpetuates dysbiosis. The resultant microbial imbalance fuels inflammation, which further depresses mood, creating a vicious cycle. People who ignore these signals often find themselves battling recurring infections. Studies from Melbourne and the Netherlands prove the statistical link between perceived stress scores and infection rates. Ignoring the science is tantamount to neglecting a ticking time bomb in your own body. You cannot simply “push through” a stressful week without consequences. Proactive measures-such as mindful breathing, consistent sleep, and targeted probiotics-are not optional, they are essential. Even a modest reduction in cortisol can restore mucosal barriers within weeks. Failure to act invites opportunistic pathogens to colonize and dominate. So, the next time you brush off stress, remember that your microbiome is watching, and it will retaliate. Take charge now before the hidden enemies establish a foothold.
nitish sharma
Incorporating mindfulness into your daily routine can dramatically reduce cortisol output, thereby preserving the integrity of both gut and vaginal barriers. A disciplined approach to sleep hygiene-aiming for seven to nine hours-reinforces immune surveillance. Coupled with targeted probiotic strains, these practices form a robust defense against opportunistic pathogens. I encourage you to adopt these strategies consistently for optimal health.
Avril Harrison
Honestly, I never thought my exam stress could mess with my stomach, let alone cause a yeast flare‑up. A simple walk and some herbal tea have been my go‑to lately, and it seems to help keep things balanced.
Natala Storczyk
Wow!!! This is exactly what we need!!! Stress blows up our bodies like a volcano!!! 🌋🔥 Let’s all grab that breathing app and smash those cortisol spikes!!! 💪🚀
Nhasala Joshi
According to the hidden agenda of the “wellness elite,” the cortisol‑induced dysbiosis is a covert method to keep the masses compliant. The microbiome‑stress feedback loop is a classic example of biowarfare in disguise ⚠️🧬. Stay vigilant, question everything, and consider the quantum impact of emotional resonance on pathogenic emergence 🌌🤯.
Grace Hada
Stress is the silent catalyst of infection.
alex montana
Stress-cortisol; gut; vagina? all under attack!!!
Wyatt Schwindt
Good points coping strategies work.
Lyle Mills
Modulating the HPA axis via biofeedback can attenuate microbial dysbiosis.
Barbara Grzegorzewska
Dearest readers, the exquisite interplay between neuroendocrine flux and microbial symphony is nothing short of a flamboyant ballet of biochemistry, and one must valiantly curate their lifestyle to avoid a tragicomic descent into dysbiosis-truly, it’s a matter of genteel self‑preservation, even if some might say “blahblah” about it.