
Every year, thousands of people in hospitals and pharmacies suffer harm-not from illness, but from the very medicines meant to help them. A misplaced decimal point. A mislabeled syringe. A drug given to the wrong patient. These aren’t rare mistakes. They’re systemic failures that happen because we’ve relied too long on human memory instead of system design.
The patient safety goals set by The Joint Commission aren’t just paperwork. They’re the bare minimum we should expect from every pharmacy and hospital that wants to keep people alive. And in 2025, those goals are sharper, more specific, and more urgent than ever.
What Are the National Patient Safety Goals (NPSGs)?
The National Patient Safety Goals (NPSGs) are updated every year by The Joint Commission, the main organization that accredits hospitals and healthcare facilities in the U.S. They started in 2003 after a landmark report called To Err is Human revealed that up to 98,000 people die each year in U.S. hospitals because of preventable medical errors. Medication errors alone were responsible for about 250,000 deaths annually.
These goals aren’t suggestions. If a hospital wants to get paid by Medicare or Medicaid, it must meet them. That’s why nearly 96% of U.S. hospitals follow them. The NPSGs focus on six areas, but the most critical for pharmacies is using medicines safely. That means fixing errors at every step: when a doctor writes a prescription, when a pharmacist fills it, when a nurse gives it to the patient, and when the patient takes it at home.
Key Medication Safety Goals for Pharmacies in 2025
The 2025 NPSGs have tightened the rules around medication dispensing. Here’s what pharmacy teams must get right:
- NPSG.03.04.01: Label everything. Every vial, syringe, IV bag, or container-even those used in surgery-must have a clear label with the drug name, strength, concentration, and expiration date. The font size must be at least 10-point. No exceptions. In operating rooms, unlabeled syringes are still found in 27% of facilities. That’s not negligence; it’s a system failure.
- NPSG.03.05.01: Manage anticoagulants. Blood thinners like warfarin are among the most dangerous drugs if dosed wrong. The goal requires standardized protocols for monitoring INR levels, educating patients, and documenting therapeutic ranges. Compliance must hit 95% every quarter.
- Barcode scanning beyond the inpatient unit. Barcode-assisted medication administration (BCMA) was once only required on hospital floors. Now, it’s expected in outpatient clinics, long-term care, and even home health settings. Facilities using BCMA report up to an 86% drop in wrong-drug errors.
- Automated dispensing cabinet (ADC) overrides. Pharmacists and nurses sometimes bypass the system to get a drug faster-especially in emergencies. But when override rates go above 5%, medication errors jump 3.7 times. The 2025 NPSGs now require facilities to track and reduce these overrides with real-time alerts and staff training.
- Bedside specimen labeling. A patient’s blood sample gets mislabeled? That can lead to a wrong diagnosis, wrong surgery, or wrong treatment. The new rule requires labels to be applied in the patient’s presence using two identifiers (name and date of birth). This simple step could prevent 160,000 adverse events each year.
Why the Five Rights Aren’t Enough
You’ve heard them: right patient, right drug, right dose, right route, right time. Nurses are taught to chant them like a mantra. But here’s the truth: 83% of medication errors happen even when all five rights are checked.
Why? Because the Five Rights put the burden on the person at the end of the line-the nurse rushing between 8 patients on a 12-hour shift. It ignores the system flaws that got the wrong drug to that nurse in the first place.
A 2023 survey of 1,200 nurses found that 78% believe the Five Rights are outdated. One nurse wrote: “We’re told to memorize them, but no one gives us the tools to actually verify them.” The answer isn’t more training. It’s better systems: barcode scanning, automated alerts, double-checks for high-risk drugs, and clear labeling.

High-Alert Medications: The Real Killers
Not all drugs are created equal. Some are so dangerous that a tiny mistake can kill. These are called high-alert medications. The Institute for Safe Medication Practices (ISMP) lists 19 critical scenarios. Here are three that kill:
- Promethazine injections. Given in the wrong vein, this anti-nausea drug can destroy tissue and cause amputations. Between 2006 and 2018, 37 patients lost limbs because it was given intravenously instead of intramuscularly. Now, hospitals must use separate containers, color-coded labels, and mandatory double-checks.
- Opioids. Giving a patient a full opioid dose without checking their tolerance can stop their breathing. Systems now require electronic alerts for opioid-naïve patients and mandatory documentation of pain scores before and after administration.
- Insulin. A misplaced decimal point turns a 5-unit dose into 50. That’s a deadly overdose. Hospitals now require insulin to be stored separately, labeled in bold, and dispensed only through pre-filled syringes or automated pumps.
Children are especially vulnerable. Medication error rates in pediatric units are three times higher than in adults. That’s why the Pediatric Medication Safety Model requires weight-based dosing with double-checks, specialized training, and electronic alerts that auto-calculate doses based on pounds or kilograms. At Children’s Hospital of Philadelphia, this cut dosing errors by 91%.
Technology That Actually Works
Technology isn’t magic. But when used right, it saves lives.
- Barcode scanning. Nurses scan the patient’s wristband and the medication barcode before giving a drug. If the system says “this isn’t right,” they stop. Simple. Effective. Reduces errors by up to 86%.
- Automated dispensing cabinets (ADCs). These locked cabinets store drugs and require a password or badge to open. They track every pill taken, who took it, and when. But when staff override them too often, safety crumbles. The fix? Limit overrides to true emergencies and review every override weekly.
- Electronic health records (EHRs) with clinical decision support. When a doctor orders 500 mg of amoxicillin for a 12-pound infant, the system should scream. It doesn’t always. The best EHRs flag dose errors, drug interactions, and allergies in real time.
- AI-powered alerts. Pilot programs at Mayo Clinic use artificial intelligence to predict which patients are at highest risk for adverse drug events. In early tests, AI cut potential harm by 47%. This isn’t sci-fi-it’s coming to hospitals near you.
What’s Missing? Culture, Not Just Checklists
Dr. Michael Cohen, former president of ISMP, says it best: “The Joint Commission’s goals are the floor, not the ceiling.” Many hospitals treat NPSGs like a compliance checklist. They train staff, run audits, and file reports. But they don’t change the culture.
True safety comes from a system where:
- Pharmacists feel safe reporting errors without fear of punishment.
- Staff are empowered to stop a medication if something feels off-even if the doctor says it’s fine.
- Leadership invests in safety, not just cost-cutting.
Dr. Terry Poling at Johns Hopkins says the Model Strategic Plan for Medication Safety-created by ASHP-is the real blueprint. It includes seven goals: leadership-driven safety, error reporting, standardized processes, communication, response to errors, community involvement, and formularies based on safety, not price.
Facilities with executive sponsorship and dedicated pharmacy leadership see 89% of their safety programs survive past five years. Those without? Only 42% make it.
Implementation: What It Really Takes
Trying to roll out these changes without a plan is like building a house without a foundation. Here’s what works:
- Assess your gaps. Use ECRI’s self-assessment tool. Score yourself on ISMP best practices. If you’re below 60%, you’re at high risk.
- Train everyone. Not just pharmacists. Nurses, techs, doctors. Each person needs 8-12 hours of training per year. Right now, 38% of facilities give less than 4 hours.
- Start with high-risk areas. Focus on anticoagulants, opioids, insulin, and pediatric meds first. Don’t try to fix everything at once.
- Track and report. You can’t improve what you don’t measure. Track override rates, labeling errors, barcode scan compliance, and adverse events. Aim for 90% documentation completeness.
- Involve patients. The WHO found that facilities with strong patient engagement see 42% fewer errors. Ask patients: “What medications are you taking?” “Do you know why?” “Did you get this before?”
It takes 12 to 18 months to fully implement these changes. But the cost of doing nothing? Far higher.
The Bottom Line
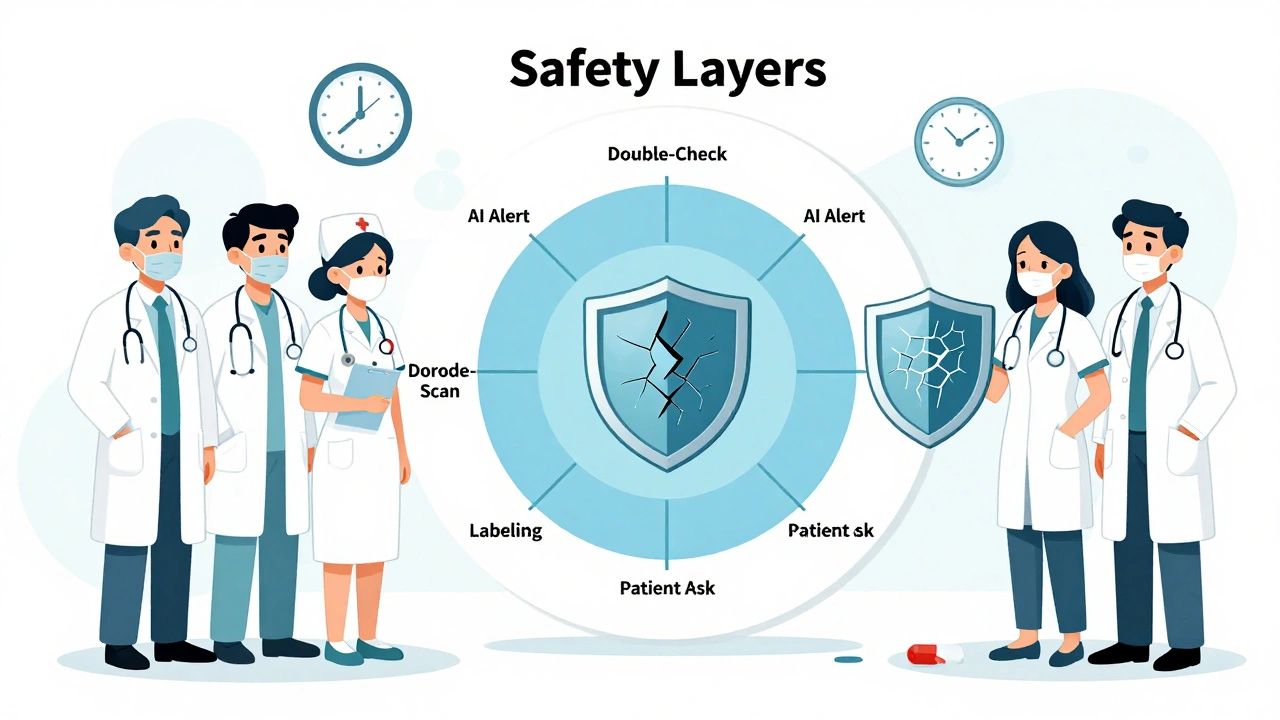
Medication safety isn’t about being perfect. It’s about building layers of protection so that when one fails, another catches it. A label. A barcode. A second check. An alert. A culture that says, “Stop if something’s wrong.”
Pharmacists are the last line of defense. But you shouldn’t be the only one holding the line. Systems must protect you. Technology must support you. Leaders must prioritize you.
In 2025, patient safety goals aren’t optional. They’re the difference between healing and harm. And in a world where a single error can end a life, we owe it to every patient to get it right.


Comments
John Filby
This is so true. I saw a nurse almost give a 50-unit insulin dose because the label was smudged. Thank god she double-checked. We need more barcodes, not more memorization.
Isabelle Bujold
I've been a hospital pharmacist for 22 years, and honestly, the NPSGs are the bare minimum. I've seen systems where the ADC override rate hits 18% because nurses are exhausted and the system doesn't support them. It's not about blame-it's about design. We need automated alerts that don't just beep but actually pause the workflow until someone confirms. And we need to stop treating pharmacists like human barcode scanners. We're clinical experts. Let us consult. Let us question. Let us be part of the decision, not just the last step in a broken chain. The insulin labeling change alone saved lives in my unit-no joke. One nurse told me she cried when she realized her patient had been getting the wrong concentration for months because the label was too small. That's not negligence. That's a system that forgot to care. We need mandatory training for all staff-not just pharmacists-on why these labels matter. And we need leadership that doesn't cut pharmacy budgets when margins shrink. Safety isn't a cost center. It's the foundation of care.
Elizabeth Crutchfield
i just read this and cried. my mom almost died bc of a med error and no one ever said sorry. just paperwork. why does it take a tragedy to fix this?
Ashley Elliott
I’ve worked in both urban and rural hospitals, and the gap in resources is insane. In one place, we had AI alerts that flagged potential interactions before the order even went through. In another, nurses were writing doses on sticky notes because the EHR crashed. Technology helps-but only if it’s accessible. And let’s not pretend that ‘training’ fixes everything. You can train someone to check five rights all day, but if the vial looks like another drug, and the screen is flickering, and they’ve got 12 patients and no break, they’re gonna make a mistake. It’s not them. It’s the system. We need to stop asking people to be perfect and start building systems that are forgiving.
Chad Handy
Let’s be real-this whole safety movement is just a PR stunt. The Joint Commission doesn’t care about patients. They care about lawsuits. They update these goals every year so hospitals keep paying for their ‘accreditation’ services. And don’t get me started on barcode scanning-most of the time, it’s just another thing nurses have to click through while they’re running on fumes. They don’t fix errors-they just create more steps. And who pays for all this tech? The patient, through higher bills. This isn’t safety. It’s corporate theater.
Augusta Barlow
You know what they don’t tell you? The same companies that sell the barcode scanners and ADCs also own the EHRs. And guess what? They design them to make overrides easy-because if you can’t override, you’ll buy their ‘premium’ version. It’s all a money grab. The real reason they push these ‘goals’? So when someone dies, they can say, ‘We followed protocol.’ But protocol doesn’t save lives. People do. And if you’re too busy clicking through 17 pop-ups to give a med, you’re not helping anyone. The system is rigged. And they’re laughing all the way to the bank.
Joe Lam
I’ve reviewed 37 hospital compliance reports this year. 90% of them are performative. They have the labels, the scanners, the audits-but they don’t have culture. You can’t fix a broken system with a checklist. You need leaders who sit in the ER at 3 a.m. and ask, ‘What’s really going wrong?’ Not ‘Are we compliant?’ The NPSGs are a joke if they’re not paired with psychological safety. If your pharmacist is afraid to say, ‘This order is wrong,’ then you’ve already lost.
Chase Brittingham
I work in a small clinic and we just implemented bedside labeling last month. We had a mom come in with her 4-year-old and she caught a mislabeled vial because she asked, ‘Is this the same as last time?’ She wasn’t a nurse. She was a parent. That’s the real safety net. We started asking patients to confirm their meds before they leave. Simple. Human. It cut our errors by 40%. We didn’t need AI. We just needed to listen.
Bill Wolfe
Let me be blunt: if your pharmacy still allows unlabeled syringes in the OR, you’re not just negligent-you’re a danger to society. I’ve seen ORs where techs grab vials off the cart like they’re grabbing snacks. And then they wonder why someone dies. The Joint Commission’s rules are barely enough. We need mandatory re-certification every 6 months for everyone handling meds. No exceptions. No ‘but we’re short-staffed.’ If you can’t follow the rules, you shouldn’t be touching a syringe. Period. And if your hospital won’t enforce this, they shouldn’t be allowed to operate. This isn’t healthcare. It’s Russian roulette with IV bags.
michael booth
Implementation is key. We rolled out BCMA in our outpatient clinic over 14 months. We trained everyone. We started with anticoagulants. We tracked every override. We celebrated small wins. The error rate dropped 82%. It wasn’t magic. It was discipline. And leadership didn’t just sign off-they showed up. Every quarter. In the pharmacy. Watching. Listening. That’s how you change culture. Not with posters. With presence.
Alex Piddington
I’ve been training pharmacy techs for 15 years. The biggest mistake? Assuming they know why they’re doing something. We don’t just teach them to scan. We teach them to think. ‘Why is this dose 10x higher than usual?’ ‘Why is this drug in a clear bag?’ ‘Who wrote this order?’ We turn compliance into curiosity. And when they start asking questions, the errors stop.
Shofner Lehto
I’m a nurse in a pediatric ICU. We started using weight-based dosing with auto-calculation last year. Before? We had two near-misses in three months. After? Zero. Not one. It’s not about tech. It’s about making the right choice the easy choice. We stopped relying on nurses to do math under stress. We automated the math. And we gave them back their time. That’s what safety looks like.
val kendra
The Five Rights are a relic. We need the Five Systems: labeling, scanning, alerts, double-checks, and culture. One without the others is just noise. I’ve seen it all. The best units aren’t the ones with the fanciest tech-they’re the ones where the pharmacist feels safe saying, ‘Hold on.’ That’s the real win.