
Antidepressant Risk Comparison Tool
How This Tool Works
This tool compares the relative risk of suicidal thoughts with different antidepressants based on clinical evidence. It's designed to help you understand the differences between medications and make informed decisions with your doctor.
The data shows the risk profile for young people under 25, as they are most affected by the FDA black box warning. For adults over 25, the risk is much lower and the benefits usually outweigh the risks.
Medication Risk Comparison
Early Warning Signs to Watch For
During the first 1-4 weeks of starting an antidepressant, some people may experience:
- Increased agitation or restlessness
- Insomnia
- Increased talk about death or self-harm
- Withdrawing from friends and family
- Increased irritability
If you notice any of these symptoms, contact your doctor immediately.
When you start taking an antidepressant, your doctor should talk to you about one thing you might not expect: the risk of suicidal thoughts. It sounds scary. And it’s supposed to. The U.S. Food and Drug Administration (FDA) put a black box warning on all antidepressants in 2004 - the strongest safety alert they can give short of pulling the drug off the market. This warning doesn’t say antidepressants cause suicide. It says they might increase the risk of suicidal thoughts and behaviors, especially in kids, teens, and young adults under 25. But here’s the part no one talks about: the warning might be doing more harm than good.
What the Black Box Warning Actually Says
The FDA’s black box warning is printed in bold, at the very top of every antidepressant’s prescribing guide. It’s not a footnote. It’s front and center. It says: “Antidepressants increase the risk of suicidal thinking and behavior in children, adolescents, and young adults in short-term studies.” The warning covers all antidepressants - SSRIs like fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro), as well as SNRIs like venlafaxine (Effexor) and even bupropion (Wellbutrin).
It’s based on a review of 24 clinical trials involving over 4,400 young people. In those trials, 4% of those taking antidepressants had suicidal thoughts or behaviors - twice the rate of those on placebo (2%). No one died. But the events were serious enough: planning, talking about death, self-harm attempts. The FDA didn’t find a single case where antidepressants caused a completed suicide in those studies. But the rise in suicidal thinking? That was real.
By 2006, the warning was expanded to include everyone under 25. Fluoxetine (Prozac) got a special exception - it’s still the only antidepressant approved for treating depression in children under 18. Sertraline and fluvoxamine are approved for OCD in kids, but not for depression. The rest? All carry the same warning.
Why This Warning Exists - And Why It’s Controversial
The FDA didn’t make this call lightly. A team of 10 pediatric suicidologists from Columbia University independently reviewed the drug companies’ raw data. They didn’t trust the original summaries. So they went back, reclassified every report of suicidal behavior, and confirmed the risk. That’s rare. Most warnings are based on the drugmakers’ own analysis. This one wasn’t.
But here’s where it gets messy. The trials were short - usually 8 to 12 weeks. They didn’t track long-term outcomes. And they didn’t look at people with severe depression. Most participants had mild to moderate symptoms. So what happens when you give these drugs to someone who’s truly at risk - someone who’s already thinking about ending their life?
Some experts say the warning saved lives. Others say it’s made things worse.
The Unintended Consequences
After the warning went live, prescriptions for antidepressants in young people dropped by 22.3% in just two years. Psychotherapy visits fell too - by 17.1%. Meanwhile, emergency room visits for drug poisonings - often self-harm attempts - jumped 28.6%. And suicide deaths among teens rose 14.9% between 2003 and 2005.
A 2023 study in Health Affairs looked at 15 years of data. It found the warning didn’t just reduce prescriptions - it reduced care. Kids with depression stopped seeing doctors. Families became terrified. Some parents refused medication outright. And when medication was avoided, suicide risk went up.
One real case: a 16-year-old girl with severe depression refused fluoxetine after reading the black box warning online. Her parents agreed. Within three months, she attempted suicide. She survived. But her therapist later said: “If she’d taken the medication, we might have prevented this.”
The problem isn’t the warning itself. It’s how people interpret it. Many believe the FDA is saying: “Antidepressants cause suicide.” That’s not true. The warning says: “In the first few weeks of treatment, some people - especially young ones - may feel worse before they feel better. Watch closely.”
Not All Antidepressants Are the Same
The black box warning treats all antidepressants like they’re identical. But they’re not.
A 2021 meta-analysis in JAMA Psychiatry found big differences. Paroxetine (Paxil) had the highest risk of suicidal behavior in young people. Fluoxetine (Prozac) had the lowest. Sertraline was in the middle. Mirtazapine and bupropion showed almost no increase in risk.
Why does this matter? Because if you’re a teen with depression, your doctor should be choosing the drug with the lowest risk - not just any SSRI. But most prescribers don’t know this. The black box warning doesn’t break it down. It just says “all of them.”
And here’s another twist: some antidepressants work better for certain symptoms. Fluoxetine helps with energy and motivation. Sertraline is better for anxiety. If you’re severely depressed and unmotivated, a drug that doesn’t help with energy might make you feel even more stuck. That could increase suicidal thoughts - not because of the drug’s danger, but because it’s the wrong fit.
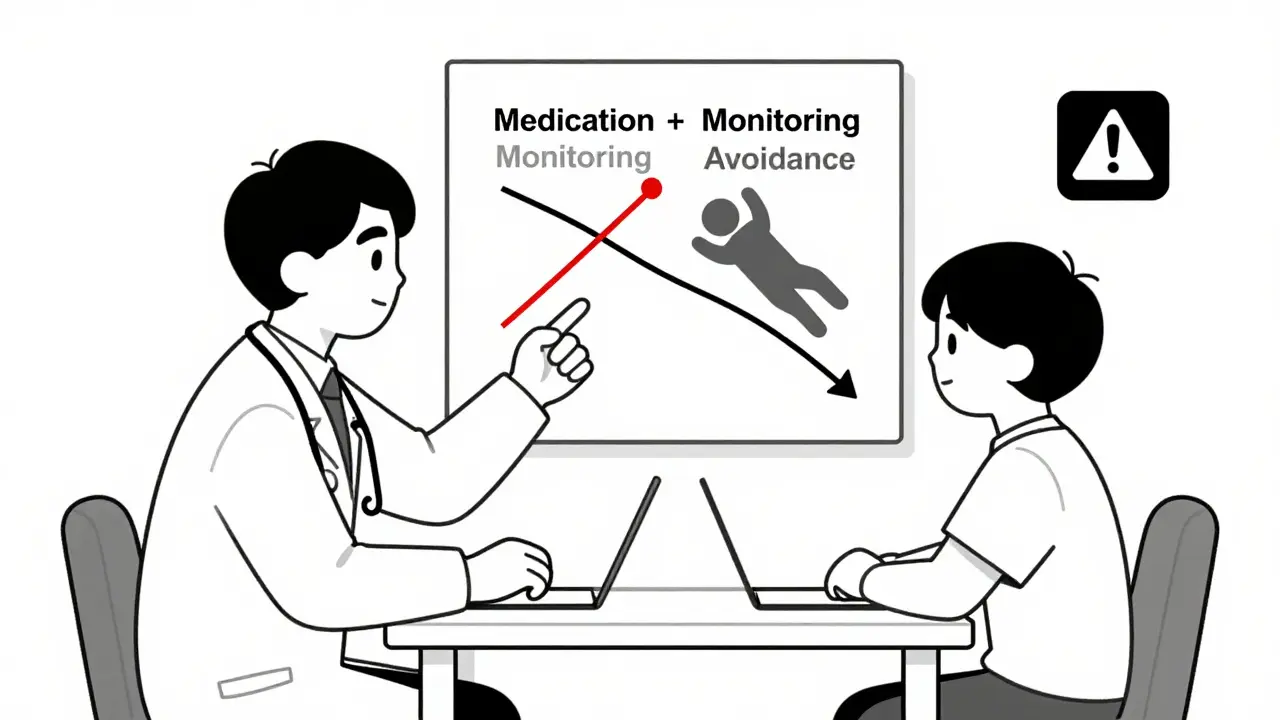
What Doctors Should Be Doing - But Often Aren’t
The FDA didn’t just slap on a warning. They also required doctors to give patients a MedGuide - a written handout explaining the risk. But most patients never read it. And many doctors don’t discuss it properly.
A good clinical practice looks like this:
- Explain that suicidal thoughts can happen early in treatment - usually within the first 1 to 4 weeks.
- Emphasize that this doesn’t mean the drug isn’t working. It means the brain is adjusting.
- Set up weekly check-ins for the first month - not just a 6-week follow-up.
- Ask directly: “Have you had thoughts about hurting yourself this week?”
- Make sure family members or roommates know what to watch for.
- Never start an antidepressant without a plan for monitoring.
Too often, patients get a prescription, a 30-day supply, and a vague warning. No follow-up. No safety plan. That’s not treatment. That’s negligence.
The Bigger Picture: Depression Is the Real Killer
The American Psychiatric Association says this clearly: Untreated depression carries a far higher risk of suicide than treated depression. The lifetime risk of suicide for someone with major depression? Around 15%. That’s higher than the risk of dying in a car crash.
Antidepressants aren’t magic. But for many people, they’re the only thing that brings relief. A 2020 review in PMC found that when antidepressant use dropped, suicide attempts went up. Not because the drugs caused harm - but because people stopped getting help.
Here’s the truth: if you’re severely depressed, waiting to see if things get better on their own is dangerous. Antidepressants don’t fix everything. But they can give you the energy to start therapy, reconnect with friends, and rebuild your life.
What You Should Do If You’re Considering Antidepressants
If you’re under 25 and thinking about starting an antidepressant:
- Ask your doctor: “Which drug has the lowest risk of suicidal thoughts for someone like me?”
- Request fluoxetine (Prozac) if you’re under 18 - it’s the only one approved for teen depression.
- Insist on weekly check-ins for the first month.
- Have a trusted person - a parent, partner, or friend - check in with you daily.
- Know the warning signs: increased agitation, insomnia, talking about death, withdrawing completely.
- Don’t stop the medication without talking to your doctor. Stopping suddenly can make things worse.
If you’re already on an antidepressant and feel worse - especially in the first few weeks - don’t panic. Call your doctor. Don’t quit. This is normal for some people. It doesn’t mean the drug won’t work. It means you need support.
The Future of the Warning
The FDA reviewed the warning again in 2022. They kept it - but added new language to clarify that the risk is highest early in treatment and that the benefits often outweigh the risks for most patients.
Experts agree: the black box warning needs to change. A class-wide warning doesn’t make sense. We need medication-specific warnings. We need better education. We need to stop scaring people away from treatment.
The goal isn’t to eliminate risk. It’s to manage it. Depression kills. Untreated depression kills faster than any drug ever could.
Do antidepressants cause suicide?
No. Antidepressants don’t cause suicide. But in the first few weeks of treatment, some people - especially under age 25 - may experience increased suicidal thoughts. This is rare, temporary, and usually happens before the medication starts working. The real danger is not taking treatment at all - untreated depression has a much higher suicide risk.
Why is fluoxetine (Prozac) the only antidepressant approved for teens?
Fluoxetine is the only antidepressant that has consistently shown a favorable benefit-risk profile in teens with major depression. In clinical trials, it reduced depressive symptoms without a significant increase in suicidal behavior. Other SSRIs either didn’t show clear benefits or had higher rates of adverse events in young people. That’s why it’s the only one approved for depression in patients under 18.
Should I avoid antidepressants if I’m under 25?
Not necessarily. If you have moderate to severe depression, the risks of not treating it - including suicide, self-harm, and long-term disability - are far greater than the small, temporary risk of increased suicidal thoughts. Talk to your doctor about fluoxetine or sertraline, which have the lowest risk profiles. Never skip treatment because of fear. But do insist on close monitoring.
What should I do if I start feeling worse after beginning an antidepressant?
Call your doctor immediately. Don’t stop the medication on your own. Feeling worse in the first 1-4 weeks is a known pattern for some people. Your doctor may adjust the dose, switch medications, or add therapy. This is not a sign that the drug is failing - it’s a signal that you need more support right now.
Is the black box warning outdated?
Evidence suggests it is. Studies show the warning led to fewer prescriptions, fewer therapy visits, and more suicide deaths. Experts now recommend replacing the blanket warning with medication-specific alerts and clearer guidance on monitoring. The FDA has started updating the language, but the warning remains unchanged. More research is needed before it’s fully revised.
Final Thought: Don’t Let Fear Keep You From Help
Antidepressants aren’t perfect. They don’t work for everyone. And yes - they come with risks. But so does doing nothing. If you’re struggling, please don’t let a warning label stop you from getting help. Talk to a professional. Ask questions. Demand monitoring. And remember: the goal isn’t to avoid all risk. It’s to find the safest path forward - and that path often includes medication.


Write a comment