Bladder Incontinence: What It Is, Why It Happens, and How to Manage It
If you’ve ever felt a sudden urge to run to the bathroom or noticed a small leak when you laugh, you’re not alone. Bladder incontinence—also called urinary leakage—is a common problem that affects millions of adults, both men and women. The good news is that most cases have clear reasons behind them, and there are easy steps you can take right now to feel more in control.
Why Your Bladder Might Be Leaking
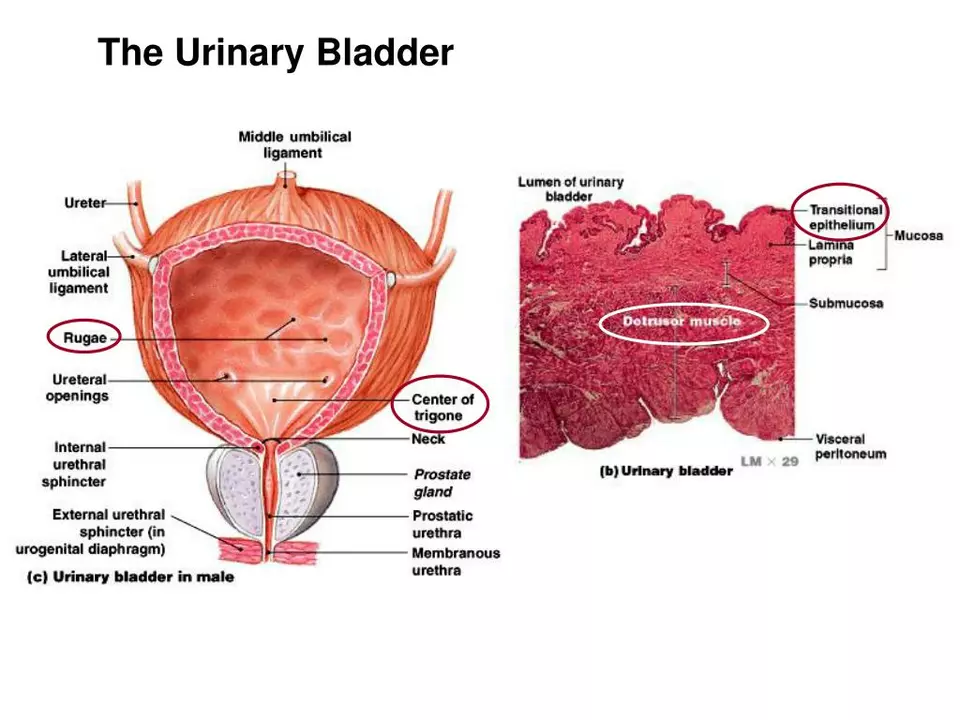
The bladder works like a balloon: it fills with urine, stores it, and then empties when a signal tells the muscles to contract. Anything that weakens those muscles or confuses the signals can cause leakage. Common culprits include:
- Weak pelvic floor muscles. These are the muscles you use to stop the flow of urine mid‑stream.
- Overactive bladder. The muscle contracts too often, creating a sudden urge.
- Enlarged prostate (in men). It can block urine flow and cause pressure buildup.
- Pregnancy or childbirth. Hormone changes and the strain of labor stretch pelvic muscles.
- Medications. Diuretics, antihistamines, and some blood pressure drugs increase bathroom trips.
Identifying which factor applies to you helps narrow down the best treatment plan.
Simple Steps You Can Try Today
Before you rush to a doctor’s office, try these low‑risk strategies. They’re cheap, easy, and often enough to make a noticeable difference.
- Pelvic floor exercises (Kegels). Sit or lie down, tighten the muscles you’d use to stop urinating, hold for five seconds, then release. Do three sets of ten reps each day. Over weeks, the muscles get stronger and leaks decrease.
- Timed voiding. Set a schedule—every two to four hours—to empty your bladder, even if you don’t feel an urge. This trains the bladder to hold more urine safely.
- Watch fluid intake. Cut back on caffeine and alcohol; they irritate the bladder. Keep water steady throughout the day instead of gulping large amounts at once.
- Weight management. Extra weight pushes on the pelvis, weakening support for the bladder. Losing a few pounds can relieve pressure and improve control.
- Dress smart. Loose‑fit clothing and breathable underwear reduce irritation and make bathroom trips easier.
If these tweaks don’t help after a month or two, it’s time to talk to a healthcare professional. They can suggest medical options such as prescription medications, bladder training programs, or minimally invasive procedures.
When to Seek Professional Help
You should call a doctor if you notice any of these signs:
- Painful urination or blood in the urine.
- Frequent infections (more than three a year).
- Sudden, severe leakage that disrupts daily life.
- Inability to empty the bladder completely.
A urologist or pelvic health therapist can run simple tests—like a post‑void residual scan—to pinpoint the problem. Treatment may involve prescription drugs that calm an overactive bladder, topical estrogen for women after menopause, or even a small surgical sling to support the urethra.
Remember, bladder incontinence is treatable, and most people find relief with a combination of lifestyle changes and professional care. You don’t have to live with constant worry about leaks—start with a few easy habits today, track your progress, and reach out for help if you need it. Your bladder will thank you.
The impact of bladder and urinary incontinence symptoms on exercise and physical activity
In my recent blog post, I discussed the impact of bladder and urinary incontinence symptoms on exercise and physical activity. It's surprising to know that these symptoms can significantly affect a person's confidence and willingness to participate in physical activities. As a result, many individuals experiencing incontinence tend to avoid exercises, which in turn, can lead to a decline in overall health and well-being. Fortunately, there are ways to manage these symptoms, such as using appropriate incontinence products and seeking professional help. By addressing this issue, we can help individuals regain control of their lives and stay active in spite of their bladder challenges.
read more