CGM Dose Adjustment: How Continuous Glucose Monitoring Changes Insulin and Medication Decisions
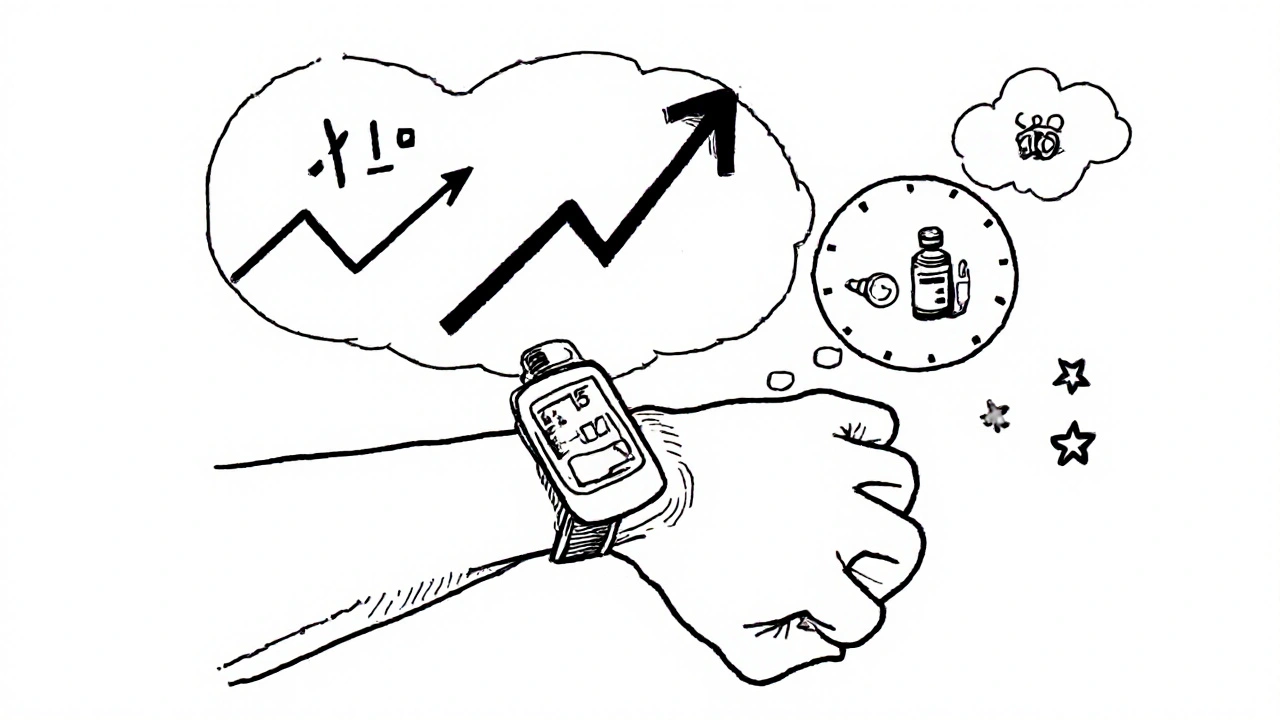
When you use a continuous glucose monitoring, a wearable device that tracks glucose levels in real time, often every 5 minutes. Also known as CGM, it gives you a live picture of how your blood sugar moves—up and down—throughout the day and night. This isn’t just a number on a screen. It’s a story. And that story changes how you take insulin, adjust meals, or even switch medications.
CGM dose adjustment isn’t guesswork anymore. It’s data-driven. If your glucose spikes after breakfast every day, you know it’s not "just bad luck"—it’s a signal to tweak your insulin bolus. If your levels dip in the middle of the night without you feeling it, that’s hypoglycemia unawareness, and your doctor might lower your bedtime insulin. You don’t need to rely on fingersticks alone. Studies show people using CGM reduce HbA1c by 0.5% to 1.5% on average, simply by acting on the trends, not just the spikes. And it’s not just for type 1 diabetes. More people with type 2 on insulin, or even those on GLP-1 agonists, use CGM to avoid lows and understand how food, stress, or sleep affects their numbers.
Related tools like insulin dosing, the process of calculating how much insulin to take based on food, activity, and current glucose levels. Also known as carb counting with correction factors, it becomes far more precise when paired with CGM. You’re no longer reacting to a single number—you’re seeing the direction and speed of change. A rising arrow at 3 a.m. tells you something different than a falling one. And glucose trends, the patterns of rising, falling, or stable glucose over hours. Also known as rate-of-change indicators, they help you decide whether to wait, correct, or eat. This is why many endocrinologists now say: if you’re on insulin and not using CGM, you’re flying blind.
CGM dose adjustment also helps avoid dangerous mistakes. For example, combining insulin with beta-blockers can hide low blood sugar symptoms. But with CGM, you don’t need to feel the low—you see it coming. That’s life-saving. It’s not just about numbers. It’s about confidence. Knowing your body’s response to stress, exercise, or even a bad night’s sleep lets you adjust before things go wrong. And when you see your glucose curve after a meal, you learn what foods truly spike you—not what the diet books say.
People who stick with CGM long-term don’t just manage diabetes better—they live better. Fewer hospital visits. Fewer panic checks in the middle of the night. More freedom to eat, sleep, and move without fear. The real power of CGM isn’t in the device. It’s in the decisions you make because of what it shows you.
Below, you’ll find real-world guides from people who’ve walked this path—how they adjusted their insulin, handled overnight lows, used CGM data with their doctors, and even figured out which foods wrecked their numbers. No fluff. Just what works.
How to Adjust Diabetes Medication Doses Using CGM Trend Arrows to Prevent Low and High Blood Sugar
Learn how to use CGM trend arrows to adjust insulin and other diabetes medications in real time, preventing dangerous lows and highs with science-backed protocols. Reduce hypoglycemia, improve time-in-range, and take control of your diabetes management.
read more