Physical Activity and Medication: Boost Health With Smart Exercise Choices
If you take prescription meds, moving your body isn’t just okay—it can actually make the drugs work better. Simple habits like a daily walk or short bike ride help control blood pressure, improve mood, and keep weight in check, which all feed into how well medication does its job.
How Exercise Changes What Your Medicine Does
When you exercise, your heart pumps faster, lungs breathe deeper, and muscles need more oxygen. Those changes speed up blood flow, so the medicine reaches every part of your body quicker. For example, people on blood‑thinners notice that a regular jog helps keep clot risk steady because circulation stays smooth.
At the same time, activity can lower the dose you need for certain drugs. Diabetes patients who walk 30 minutes most days often see their insulin requirements drop. That’s not magic—it’s your body becoming more efficient at using glucose after you move.
Staying Safe While You Sweat
Not all meds love heavy sweating. Some heart medicines can cause dizziness if you stand up too fast after a hard workout. To avoid that, cool down slowly and keep water handy. If you’re on thyroid pills, take them with a full glass of water and wait at least 30 minutes before any vigorous activity; food and intense exercise can mess with absorption.
Know the red flags: sudden chest pain, shortness of breath beyond normal workout fatigue, or unusual bruising. Those could mean your drug isn’t playing nice with the extra stress you’re adding. Stop exercising for that session and call your doctor.
Timing matters too. For most pills, morning is best because you’re up and moving. If you prefer evening workouts, talk to a pharmacist about whether taking meds after exercise changes effectiveness.
Here are three quick steps to keep the balance right:
- Check with your doctor or pharmacist before starting a new routine.
- Start slow—10‑minute walks, then add minutes each week.
- Track how you feel: energy levels, sleep quality, and any side effects.
Remember, the goal isn’t to become an elite athlete overnight. Even modest activity can lower blood pressure by a few points, cut cholesterol, and help weight loss—all of which reduce the strain on the drugs you’re already taking.
If you have joint pain or arthritis, low‑impact options like swimming or yoga keep you moving without stressing joints. Those choices also boost flexibility, which can improve posture and reduce back pain that sometimes comes from sitting for long periods while filling prescriptions.
Finally, don’t forget the mental side. Exercise releases endorphins, which can lift mood and lessen anxiety. For people on antidepressants, this extra boost often means a smoother path to feeling better, sometimes letting doctors lower dosages safely.
Bottom line: regular physical activity is a free tool that works hand‑in‑hand with your meds. Use it wisely, listen to your body, and keep the conversation open with your healthcare team. Your health will thank you with stronger results and fewer side effects.
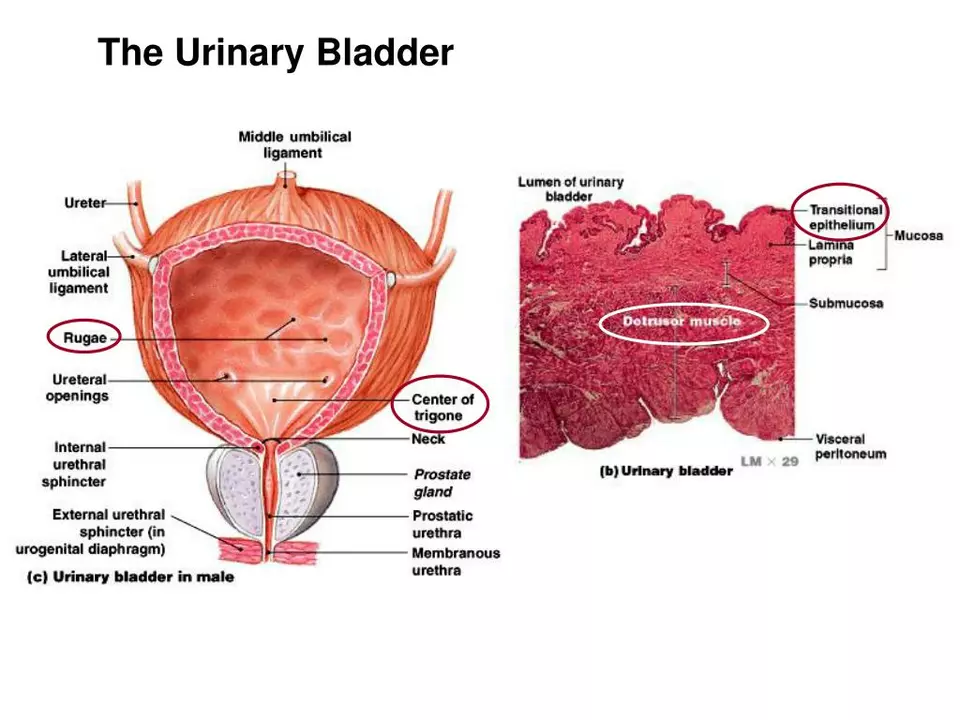
The impact of bladder and urinary incontinence symptoms on exercise and physical activity
In my recent blog post, I discussed the impact of bladder and urinary incontinence symptoms on exercise and physical activity. It's surprising to know that these symptoms can significantly affect a person's confidence and willingness to participate in physical activities. As a result, many individuals experiencing incontinence tend to avoid exercises, which in turn, can lead to a decline in overall health and well-being. Fortunately, there are ways to manage these symptoms, such as using appropriate incontinence products and seeking professional help. By addressing this issue, we can help individuals regain control of their lives and stay active in spite of their bladder challenges.
read more