TNF Inhibitor Cancer Risk Calculator
This tool estimates your relative cancer risk profile when taking TNF inhibitors based on the latest research. Remember: TNF inhibitors are not cancer triggers when used wisely. This assessment helps you and your doctor make informed treatment decisions.
Recommendations
When you’re living with rheumatoid arthritis, psoriatic arthritis, or Crohn’s disease, the idea of taking a drug that suppresses your immune system can be terrifying. You’ve heard the warnings: biologics might raise your cancer risk. Especially TNF inhibitors-drugs like Humira, Enbrel, and Remicade-that block a key inflammation protein called tumor necrosis factor-alpha. But is the fear real? Or is it based on old data, misunderstood science, or panic from a single black box warning on a pill bottle?
The truth isn’t simple. It’s layered. And it matters because over 1.5 million Americans are on these drugs right now. Many of them are young, active, and worried. They want to know: if I take this, will I get cancer? And if I already had cancer, can I still use it?
How TNF Inhibitors Actually Work
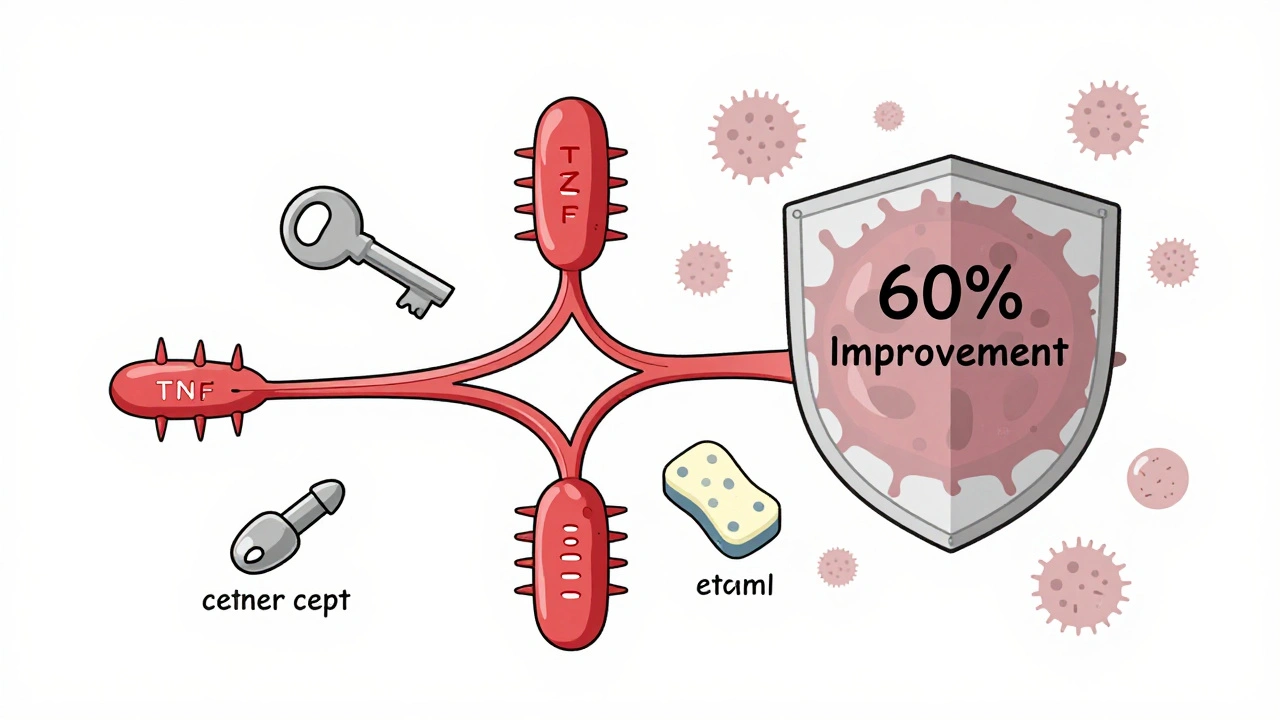
TNF-alpha is a chemical your body uses to fight infection and trigger inflammation. In autoimmune diseases, it goes haywire-attacking your joints, skin, or gut instead of germs. TNF inhibitors shut that down. But they don’t all work the same way.
Infliximab, adalimumab, and golimumab are monoclonal antibodies. They latch onto TNF like a key in a lock. Etanercept is a fusion protein-it acts like a decoy, soaking up excess TNF before it can cause damage. Certolizumab is a smaller fragment, designed to be more targeted. All of them are injected or infused, require refrigeration, and cost between $4,500 and $6,500 a month. And yes, they work. About 60% of patients see major improvement in joint pain, swelling, and fatigue within six months.
But here’s the catch: by dampening your immune system’s ability to detect trouble, you might be making it harder for your body to spot early cancer cells. That’s the theory. But theory doesn’t always match real life.
The Cancer Risk Data: What the Studies Really Say
The biggest fear? Lymphoma. Back in 2008, the FDA added a black box warning to all TNF inhibitors because early trials showed a small rise in lymphoma cases. But those trials were short. They didn’t follow patients long enough to see the full picture.
Fast forward to 2022. The Swedish ARTIS registry tracked 15,700 rheumatoid arthritis patients for up to 12 years. The result? No overall increase in cancer risk compared to patients on older, non-biologic drugs. In fact, the hazard ratio was 0.98-meaning TNF inhibitors were slightly *less* linked to cancer than the alternatives.
But there’s a twist. Adalimumab showed a temporary spike in cancer risk during the first year after starting treatment. Etanercept? Lower risk than even patients not on biologics. Why? Researchers think it’s not the drug causing cancer-it’s the other way around. People who are already developing cancer might have worse inflammation, so doctors start them on TNF inhibitors earlier. That’s called protopathic bias. The cancer was already there. The drug didn’t cause it.
For skin cancer, the data is clearer. A 2021 meta-analysis of over 32,000 psoriasis patients found a 32% higher risk of non-melanoma skin cancer (basal cell and squamous cell carcinomas) with TNF inhibitors. That’s not huge-but it’s real. And it’s why dermatologists now recommend skin checks every six months for anyone on these drugs.
And here’s something surprising: a 2023 study found RA patients on TNF inhibitors who later developed lung cancer had a 42% better chance of surviving five years than those on traditional drugs. Why? Maybe because TNF inhibitors reduce inflammation that helps tumors grow. Or maybe because these patients get better overall care. Either way, it flips the script.
Which TNF Inhibitor Is Safest?
Not all TNF inhibitors are created equal when it comes to cancer risk. Based on the latest data:
- Etanercept has the lowest cancer risk profile. It’s often the go-to for patients with a history of skin cancer or older adults.
- Adalimumab carries a slightly higher risk-especially for non-melanoma skin cancer. Studies show a 1.3x higher rate than etanercept.
- Infliximab and golimumab fall in between. No major red flags, but not the safest either.
- Certolizumab has the least long-term data, but early signals suggest it’s similar to etanercept.
That’s why rheumatologists now choose based on your personal history. If you’ve had basal cell carcinoma before? Etanercept is likely your best bet. If you’re young, healthy, and have aggressive joint damage? Adalimumab might still be the right tool.
What If You’ve Had Cancer Before?
This is the question that keeps patients up at night. I had breast cancer three years ago. Can I take Humira now?
The answer: maybe. And it’s not a yes-or-no decision. It’s a team decision.
According to 2023 American College of Rheumatology guidelines, you need to be cancer-free for at least five years before restarting TNF inhibitors if you had lymphoma or melanoma. For breast, prostate, or colon cancer? Two years is usually enough.
And here’s what the data shows: 87% of rheumatologists continue TNF inhibitors in patients with early-stage, low-risk cancers after talking to their oncologist. And 92% of those patients had no cancer recurrence linked to the drug.
One patient in Melbourne, 54, had stage I breast cancer in 2020. She went off her biologic for two years. After her oncologist cleared her, she restarted etanercept. Her arthritis stayed under control. Her cancer didn’t come back. She’s now in her fifth year on the drug.
That’s not luck. It’s careful planning.
What About Glucocorticoids? The Hidden Risk
Here’s something no one talks about enough: steroids.
Many patients on TNF inhibitors also take prednisone. It’s common. It works fast. But high doses-7.5 mg or more per day-have been linked to worse cancer outcomes. One 2023 study found patients on high-dose steroids had nearly triple the risk of dying from cancer compared to those not on steroids.
That means: if you’re on a TNF inhibitor and still taking daily steroids, you’re not just managing inflammation-you’re stacking risks. The goal isn’t just to control arthritis. It’s to get you off steroids as fast as possible.
Most rheumatologists now aim to taper steroids within three to six months of starting a biologic. If you’re still on them after a year, ask why.

What Patients Are Really Saying
Online forums are full of fear. Reddit threads titled “I’m scared to start Humira” get hundreds of comments. One woman wrote: “My doctor said it’s safe. But I read the pamphlet. It says ‘may cause cancer.’ I’m not taking it.”
But the other side? There are thousands of people who say: “This drug gave me my life back.”
A 2023 survey by the National Psoriasis Foundation found 78% of patients who had early-stage cancer would restart their TNF inhibitor after treatment. Why? Because their quality of life was too good to give up. They’d rather monitor their skin than live in pain.
And 65% of them said their dermatologist recommended skin checks every six months. That’s the key: not stopping the drug, but staying vigilant.
What You Should Do Right Now
If you’re considering a TNF inhibitor-or already on one-here’s what to do:
- Get a full skin exam from a dermatologist before starting. Document any moles or lesions.
- Ask your rheumatologist: “Which TNF inhibitor do you recommend for me, and why?” Don’t accept “it’s the most popular.” Ask about your personal risk.
- Review your steroid use. Are you still on prednisone? If yes, ask for a plan to get off it.
- If you’ve had cancer, bring your oncology records to your rheumatology appointment. Don’t assume they’ll know your history.
- Schedule skin checks every six months. Even if you feel fine.
- Don’t panic over old warnings. The FDA’s black box warning is based on early data. The latest studies show the risk is far lower than feared.
Most importantly: don’t stop your medication because of fear. Untreated inflammation does damage too. It increases your risk of heart disease, lung problems, and even some cancers. A controlled immune system is better than a raging one.
The Future: Personalized Risk Scoring
By 2027, we’ll likely see something new: genetic risk scores for TNF inhibitor users. Researchers are already identifying gene variants that make some people 3.2 times more likely to develop lymphoma on these drugs. Imagine a simple blood test that tells you: “Your genetic profile suggests low risk. You’re safe on adalimumab.” Or: “You’re high risk. Try etanercept instead.”
That’s not sci-fi. It’s coming. And it means the days of one-size-fits-all warnings are ending.
For now, the message is clear: TNF inhibitors are not a cancer trigger. They’re a powerful tool. Used wisely-with screening, monitoring, and smart choices-they can give you back your life without putting you at serious risk.
Don’t let fear silence your treatment. Let knowledge guide it.


Comments
Elizabeth Crutchfield
i just started etanercept last month and honestly? i’m terrified every time i inject it. but my joints don’t scream anymore, so i’m keeping going. skin checks every 6 months? yeah, i already booked mine.
Ben Choy
the fact that etanercept has lower cancer risk than even non-biologics is wild. i thought all TNF inhibitors were equally scary. glad i switched from humira last year. also, i’m not gonna lie-i cried when my rheum said i could stop prednisone. 😅
Jenny Rogers
It is imperative to recognize that the conflation of correlation with causation in this article is not only scientifically unsound but potentially dangerous. The Swedish ARTIS registry does not establish causality; it merely observes temporal association. Furthermore, the assertion that 'TNF inhibitors are not a cancer trigger' is a gross oversimplification of a complex immunological phenomenon. One must not disregard the FDA’s black box warning, which exists for a reason, regardless of retrospective analyses.
Moreover, the suggestion that patients should 'let knowledge guide them' is patronizing. Knowledge, without epistemological rigor, is merely opinion dressed in data. The pharmaceutical industry has a vested interest in minimizing risk perception. This article reads like a marketing whitepaper disguised as medical advice.
zac grant
Big picture: TNF-alpha isn't just an inflammation switch-it's a tumor surveillance node. Blocking it = reduced immune surveillance, period. But the real kicker? Inflammation itself is carcinogenic. So you're trading one risk (drug-induced immunosuppression) for another (chronic inflammation-driven mutagenesis).
Etanercept’s lower risk? Probably because it's a soluble receptor decoy, not a monoclonal antibody-so it doesn't trigger Fc-mediated immune cell apoptosis like infliximab does. That’s the mechanistic nuance no one talks about.
Also, prednisone is the silent killer here. 7.5mg/day is the threshold where immunosuppression shifts from therapeutic to toxic. Taper hard, fast, and early.
michael booth
Great breakdown. I’ve been on adalimumab for 4 years. No cancer. No issues. But I do my skin checks religiously. My derm says I’ve got three benign BCCs so far-caught early. That’s the point. This isn’t about avoiding the drug. It’s about managing the risk.
And yeah, I got off prednisone in 5 months. My rheum gave me a plan. Stick to the plan.
Carolyn Ford
Oh, so now we’re just supposed to ‘trust the data’? But the data is funded by Big Pharma. And you’re telling me that suppressing the immune system for decades doesn’t increase cancer risk? That’s not science-that’s wishful thinking.
My cousin died of lymphoma after 3 years on Humira. She was 31. And now you want me to ‘get a skin check’? That’s not enough. That’s not safety. That’s damage control.
And don’t even get me started on ‘etanercept is safer’-it’s still a TNF inhibitor. Same class. Same mechanism. Same warning. You’re just repackaging fear as ‘personalized medicine’.
Heidi Thomas
Stop lying to patients. The black box warning is there for a reason. You think the FDA puts those on drugs for fun? The data is messy because they didn’t follow people long enough. But guess what? We’re still watching. People are still getting lymphoma. And you’re telling them it’s okay because some registry says ‘no overall increase’? That’s not reassurance. That’s gaslighting.
Alex Piddington
Thank you for this thoughtful, evidence-based overview. As a clinician, I appreciate how you contextualized the risk without minimizing it. The distinction between etanercept and monoclonal antibodies is critical-and often overlooked.
Also, the steroid point? Crucial. Too many patients stay on prednisone for years because ‘it’s working.’ But the cost is real. We need to normalize the conversation around tapering.
And yes-skin checks every 6 months. Non-negotiable.
Libby Rees
I’ve been on adalimumab for 6 years. I had stage 1 breast cancer in 2021. My oncologist said I could restart after two years. I did. No recurrence. I get skin checks. I don’t take steroids. I feel like myself again.
It’s not about fear. It’s about balance.
Dematteo Lasonya
I’m 29 and just started etanercept. I had a basal cell removed last year. My derm said it’s fine to continue as long as I stay on top of checks. I didn’t know about the differences between the drugs until I read this. So thank you. I feel less alone now.
Rudy Van den Boogaert
My mom’s on infliximab. She had colon cancer in 2019. Treated. Remission for 5 years. Rheum said go ahead. She’s been on it for 18 months. No issues. Skin checks. Blood work. Every 3 months. She’s not scared anymore. She’s just careful. And she walks her dog every day now. That’s the win.