Tacrolimus Neurotoxicity: Signs, Risks, and What You Need to Know
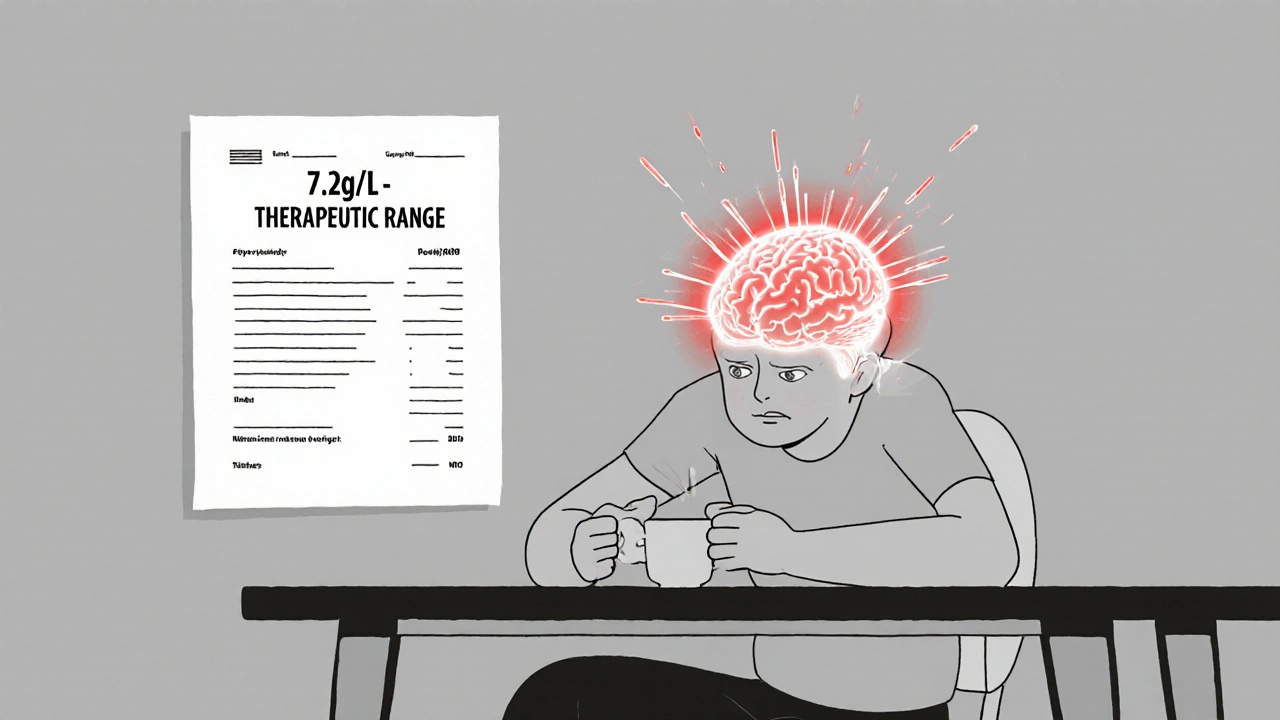
When you take tacrolimus, a powerful immunosuppressant used after organ transplants to prevent rejection. Also known as FK506, it keeps your body from attacking the new organ—but it doesn’t do so without risks. One of the most serious, though often overlooked, side effects is tacrolimus neurotoxicity, a condition where the drug affects the nervous system, leading to confusion, tremors, seizures, or even stroke-like symptoms. This isn’t rare. Studies show up to 1 in 5 transplant patients on tacrolimus experience some form of neurological side effect, especially in the first few weeks after starting treatment.
It’s not just about the dose. kidney function, how well your body clears the drug from your system. If your kidneys are struggling, tacrolimus builds up faster, raising your risk. Older patients, those with high blood pressure, or people taking other drugs that affect the liver—like antifungals or certain antibiotics—are more vulnerable. Even small changes in how you take your pills, like skipping a dose or taking it with grapefruit juice, can push levels into dangerous territory.
The symptoms don’t always show up the same way. Some people get mild tremors in their hands. Others feel dizzy, have trouble speaking, or see blurry vision. In worse cases, seizures or altered mental states happen. These aren’t just "side effects"—they’re red flags. If you’re on tacrolimus and notice anything unusual with your coordination, memory, or speech, don’t wait. Tell your doctor right away. Blood tests can check your tacrolimus levels, and sometimes just lowering the dose or switching to another immunosuppressant can reverse the problem.
What’s often missed is how easily this gets confused with other issues. A transplant patient who’s confused might be written off as "just tired" or "recovering slowly." But neurotoxicity can progress fast. It’s why doctors monitor tacrolimus levels closely—sometimes weekly at first. It’s also why some patients end up on lower doses long-term, even if their body seems to tolerate it fine. Safety matters more than maximum suppression.
There’s no one-size-fits-all fix. Some patients need a switch to cyclosporine. Others benefit from magnesium supplements, which can help calm nerve activity. And in severe cases, doctors may use plasma exchange to quickly remove the drug from the bloodstream. The key is catching it early. The longer it goes untreated, the higher the chance of lasting damage.
Below, you’ll find real-world insights from patients and clinicians who’ve dealt with this issue firsthand. From how to recognize the early signs to what labs to ask for, these posts give you the practical knowledge you won’t always get from a pamphlet. You’re not just reading about a drug—you’re learning how to protect yourself while using it.
Tacrolimus Neurotoxicity: Understanding Tremor, Headache, and Safe Blood Level Targets
Tacrolimus neurotoxicity causes tremor, headache, and other neurological symptoms in 20-40% of transplant patients-even at therapeutic blood levels. Learn what triggers it, how to spot it early, and how to manage it safely.
read more