Transplant Medication Risks: What You Need to Know About Rejection, Side Effects, and Long-Term Safety
When you get a new organ, your body doesn’t know it’s supposed to accept it. That’s why transplant medication risks, the dangers tied to drugs that prevent your immune system from attacking a transplanted organ. Also known as immunosuppressants, these drugs are life-saving—but they come with serious trade-offs. Without them, your body will reject the new kidney, heart, liver, or lung. With them, you’re more likely to get infections, develop cancer, or face kidney damage over time. It’s a constant balancing act.
immunosuppressants, a class of drugs that weaken the immune system to protect transplanted organs. Also known as anti-rejection drugs, they include cyclosporine, tacrolimus, mycophenolate, and sirolimus. Each one works differently, and each has its own side effect profile. Tacrolimus can raise your blood sugar and hurt your kidneys. Mycophenolate might cause nausea or lower your white blood cell count. Cyclosporine can make your gums swell or your hands shake. These aren’t rare side effects—they happen to most people. That’s why regular blood tests aren’t optional. Your doctor checks drug levels, kidney function, and infection markers every few weeks, especially in the first year.
One of the biggest hidden dangers is organ rejection, when the immune system attacks the transplanted organ despite medication. It doesn’t always come with warning signs. Sometimes you feel fine, but a biopsy shows early damage. That’s why sticking to your schedule matters more than you think. Missing one dose can trigger a rejection episode. And if you stop taking your meds because you’re tired of the side effects? That’s how people lose their transplants. The risk isn’t just theoretical—it’s real, and it’s common.
You’re also more vulnerable to infections. A simple cold can turn into pneumonia. A skin rash might be a sign of shingles, not allergies. Even routine dental work needs special care. Your doctor will likely recommend vaccines before transplant, but many aren’t safe after. That’s why you need to be your own advocate. If something feels off—fever, fatigue, swelling, unexplained pain—don’t wait. Call your transplant team. Early action saves organs.
Long-term, transplant patients face higher risks of skin cancer, lymphoma, and high blood pressure. Some meds cause bone thinning or weight gain. Others interfere with cholesterol or blood sugar. That’s why lifestyle changes aren’t just helpful—they’re critical. Eating well, avoiding smoking, staying active, and protecting your skin from the sun aren’t suggestions. They’re part of your treatment plan.
Below, you’ll find real, practical guides from people who’ve walked this path. Learn how to spot early signs of rejection, how to handle side effects without quitting meds, and what to do when your insurance won’t cover your next prescription. These aren’t theoretical tips. They’re lessons from patients, pharmacists, and doctors who’ve seen what works—and what doesn’t.
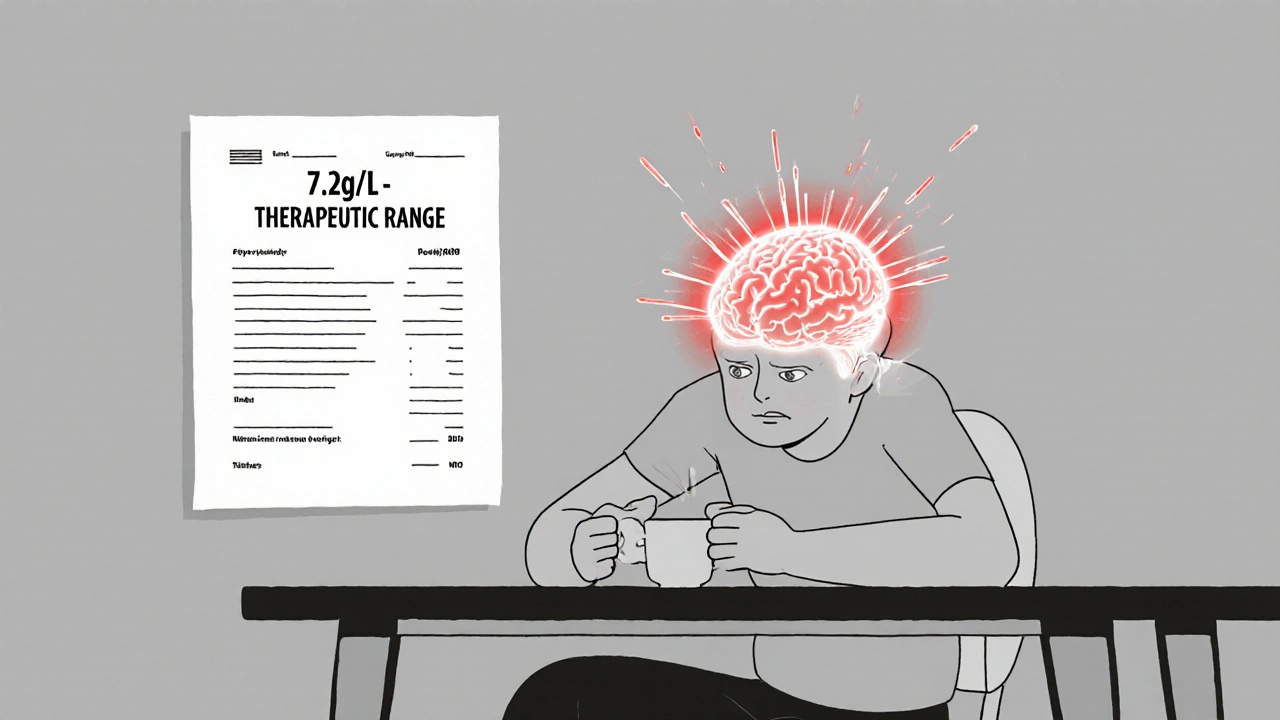
Tacrolimus Neurotoxicity: Understanding Tremor, Headache, and Safe Blood Level Targets
Tacrolimus neurotoxicity causes tremor, headache, and other neurological symptoms in 20-40% of transplant patients-even at therapeutic blood levels. Learn what triggers it, how to spot it early, and how to manage it safely.
read more