When you're on a blood thinner, it's not just about taking a pill every day. It's about balancing risk, cost, convenience, and what happens if something goes wrong. For decades, warfarin was the only game in town. Now, DOACs - direct oral anticoagulants - have taken over as the go-to choice for most people. But that doesn't mean warfarin is obsolete. And knowing how to reverse either one in an emergency? That could save your life.
Why Do People Need Blood Thinners?
Clots can be deadly. A clot in your leg can travel to your lungs and cause a pulmonary embolism. A clot in your brain? That’s a stroke. People with atrial fibrillation - an irregular heartbeat - are five times more likely to have a stroke because blood pools in the heart and can clot. After a deep vein thrombosis (DVT) or pulmonary embolism (PE), you need long-term protection. That’s where anticoagulants come in. They don’t “thin” your blood. They slow down the clotting process. And choosing the right one matters.
Warfarin: The Old Standard
Warfarin has been around since the 1940s. It works by blocking vitamin K, which your body needs to make clotting factors. Simple, right? Not quite. The problem is that warfarin’s effect is unpredictable. One day you’re perfectly in range. The next, your INR (a blood test that measures clotting time) spikes or drops. That’s why most people on warfarin get their INR checked every 2 to 4 weeks - sometimes more. The ORBIT-AF registry found patients average nearly 18 tests a year. That’s a lot of needle sticks, appointments, and anxiety.
Food matters too. Leafy greens like spinach, kale, and broccoli are full of vitamin K. Eat more one week, and your INR drops. Eat less, and it climbs. Even a single meal can throw things off. And then there are the drug interactions. Over 300 medications - from antibiotics to herbal supplements - can interfere with warfarin. A simple cold medicine could turn your INR from 2.5 to 5.0 overnight, putting you at risk of bleeding. It’s why warfarin requires constant attention.
DOACs: The Modern Alternative
DOACs - dabigatran, rivaroxaban, apixaban, edoxaban - changed everything. These drugs don’t rely on vitamin K. They directly block clotting factors: dabigatran stops thrombin, the others block factor Xa. Their effects are more predictable. No routine blood tests. Fewer food restrictions. And far fewer drug interactions - only about 40 major ones per DOAC, compared to 300+ for warfarin.
Studies confirm they’re better. The 2023 JAMA Network Open study of nearly 18,500 people with blood clots found DOACs cut the risk of another clot by 34% compared to warfarin. A 2021 meta-analysis of 35 trials showed DOACs reduced major bleeding by 17% overall. Apixaban, in particular, cut stroke risk by 25% and major bleeding by 35% compared to warfarin. For older adults, frail patients, or those with kidney issues, the safety advantage is even clearer.
And patients notice. A 2023 Mayo Clinic survey found 87% of people preferred DOACs over warfarin - mostly because they didn’t have to get blood drawn every few weeks. No more worrying about broccoli or antibiotics.

When Warfarin Still Makes Sense
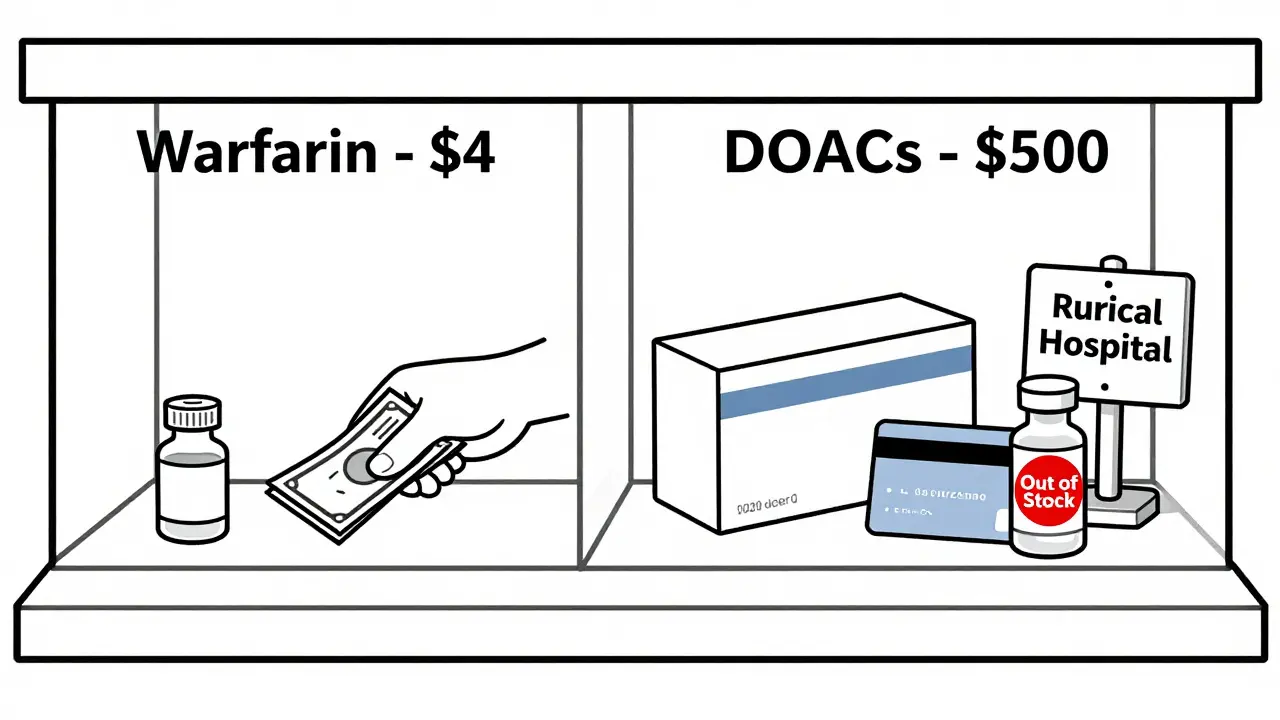
DOACs aren’t perfect. They’re expensive. Without insurance, a month’s supply can cost $300 to $500. Warfarin? As little as $4 to $30. For people on tight budgets, that difference is huge. In Australia, Medicare subsidizes warfarin heavily - but DOACs still cost more out-of-pocket.
There are also medical reasons to stick with warfarin. If you have a mechanical heart valve - like a metal one replacing a damaged aortic or mitral valve - DOACs are dangerous. They don’t work well here. Warfarin is still the gold standard. Same goes for people with severe antiphospholipid syndrome, a rare autoimmune condition that causes repeated clots. And while DOACs are generally safe in kidney disease, they’re not recommended if your eGFR drops below 15 mL/min (end-stage kidney failure). Warfarin can still be used, though carefully.
What Happens If You Bleed? Reversal Agents
This is where things get urgent. If someone on a blood thinner has a major bleed - say, a brain hemorrhage or a severe stomach bleed - you need to stop the anticoagulant fast. With warfarin, you have options. Vitamin K (given intravenously) starts working in a few hours. Fresh frozen plasma (FFP) gives you clotting factors right away. But the fastest option is a prothrombin complex concentrate (PCC). It can reverse warfarin in under 30 minutes. Hospitals keep PCC on hand.
DOACs are trickier. You can’t use vitamin K or PCC reliably. Each DOAC needs its own antidote. For dabigatran, there’s idarucizumab (Praxbind). It’s a monoclonal antibody that binds to dabigatran and neutralizes it immediately. In the RE-VERSE AD trial, it worked in 98.7% of patients with major bleeding. But it costs $3,400 per vial. For rivaroxaban, apixaban, or edoxaban, the antidote is andexanet alfa (Andexxa). It’s a modified version of factor Xa that acts like a sponge, soaking up the DOAC. One treatment course runs over $17,000.
Here’s the problem: not every hospital has these drugs. A 2023 American Hospital Association survey found only 62% of U.S. hospitals stock idarucizumab. Rural hospitals? Often none. And in Australia, access varies by region. Emergency departments in big cities like Melbourne or Sydney are usually stocked. Smaller regional hospitals? Not always.
For DOACs without a specific antidote, doctors often use 4-factor PCC anyway - even though it’s less effective. It’s a stopgap. And there’s hope on the horizon: ciraparantag, an experimental universal reversal agent, is in Phase III trials and could be available by 2026. If it works, it could reverse all DOACs - and even warfarin - with one drug.
Cost vs. Clinical Benefit
DOACs cost more upfront. But they save money over time. Why? Fewer hospitalizations for bleeding. Fewer lab tests. Fewer ER visits. A 2022 Pharmacoeconomics study found DOACs saved $1,200 to $2,800 per quality-adjusted life year (QALY) - meaning better health for less long-term cost. In Australia, the PBS (Pharmaceutical Benefits Scheme) subsidizes some DOACs, but not all. Many patients still pay hundreds per month.
And here’s the hidden risk: cost leads to nonadherence. The 2023 Medicare Current Beneficiary Survey found 34% of Medicare patients skipped or cut their DOAC doses because of cost. Only 12% did the same with warfarin. Skipping doses? That’s how strokes happen. So even if DOACs are better, they’re only better if you take them.
What’s Next?
The future of anticoagulation is moving fast. Lower doses are now approved for older, lighter, or kidney-impaired patients - like apixaban 2.5mg twice daily. The RECOVER ENCORE trial showed rivaroxaban 10mg daily worked just as well as the standard 20mg dose for long-term clot prevention - with 33% less bleeding. That’s huge for people who need to stay on blood thinners for years.
And new drugs are coming. Milvexian, a factor XIa inhibitor, showed 46% less bleeding than apixaban in a 2023 trial. It doesn’t affect the body’s ability to stop bleeding after injury - a game-changer. If approved, it could replace DOACs entirely.
For now, the message is clear: for most people with atrial fibrillation or blood clots, DOACs are the better choice. They’re safer, more convenient, and just as effective. But warfarin still has its place - especially for those with mechanical valves, severe kidney failure, or who can’t afford DOACs. And when emergencies strike, knowing which reversal agent to use - and whether your hospital has it - could be the difference between life and death.
Are DOACs safer than warfarin?
Yes, for most people. Large studies show DOACs reduce the risk of major bleeding by 17% and stroke by 22% compared to warfarin. They also have fewer drug and food interactions. Apixaban, in particular, has shown the best safety profile, cutting major bleeding by 35%. But they’re not safer for everyone - people with mechanical heart valves or very severe kidney disease still need warfarin.
Do I need blood tests if I’m on a DOAC?
No, routine blood tests like INR aren’t needed for DOACs. Unlike warfarin, DOACs have predictable effects, so your doctor doesn’t need to monitor them regularly. But in emergencies - like major bleeding or before surgery - doctors can use special blood tests (anti-Xa assays or ecarin clotting time) to check drug levels. Most community doctors still don’t know this - a 2023 survey found 47% incorrectly believed DOACs require routine INR checks.
Can I switch from warfarin to a DOAC?
Yes, if you don’t have a mechanical heart valve, severe kidney failure (eGFR <15), or antiphospholipid syndrome. Your doctor will stop warfarin, wait until your INR is below 2.0, then start the DOAC. The transition is safe and common. Many patients feel more confident and less stressed after switching - no more weekly blood tests or worrying about spinach.
What if I have a serious bleed while on a DOAC?
Call emergency services immediately. If you’re on dabigatran, the antidote is idarucizumab (Praxbind). For rivaroxaban, apixaban, or edoxaban, andexanet alfa (Andexxa) is used. If those aren’t available, 4-factor PCC may be given as a backup. Not all hospitals carry these antidotes - especially in rural areas. Knowing which DOAC you’re on and keeping a list of your medications can help emergency teams act faster.
Why is warfarin still used if DOACs are better?
Three main reasons: cost, specific medical conditions, and access. Warfarin costs as little as $4 a month. DOACs can cost $500. For people without good insurance, that’s a barrier. Also, DOACs don’t work for mechanical heart valves or severe antiphospholipid syndrome. And in some rural hospitals, reversal agents for DOACs aren’t stocked, making warfarin the safer option in those settings.


Comments
MANI V
Let me get this straight - you’re telling me we’re now recommending expensive, untested drugs over a 80-year-old miracle drug just because some pharma rep told you to? Warfarin works. It’s cheap. It’s predictable if you actually follow the rules. But no, we gotta push DOACs because they make more money. Classic. And don’t even get me started on those ‘reversal agents’ - $17k for a vial? That’s not medicine, that’s a robbery with a stethoscope.
Andrew Jackson
While the empirical data presented herein is undeniably compelling, one must not overlook the fundamental epistemological tension between pharmaceutical innovation and the entrenched ethos of clinical prudence. The ascendancy of DOACs, though statistically laudable, constitutes a paradigmatic shift predicated not upon ontological superiority, but upon market-driven hegemony. One must ask: is the reduction in INR monitoring truly a clinical advancement, or merely an aesthetic convenience? The human body, after all, is not a machine to be optimized - it is a complex, evolving organism requiring vigilance, not automation.
John Watts
Look - I’ve been on a blood thinner for 7 years. I switched from warfarin to apixaban after my third ER trip for a ‘random’ bleed. No more weekly blood draws. No more stressing over spinach. No more wondering if my cold medicine is gonna turn me into a human pincushion. And yeah, the cost sucks - but I paid $20/month with my insurance. That’s cheaper than my coffee habit. DOACs aren’t perfect, but they’re the closest thing we’ve got to a ‘set it and forget it’ life-saver. If you’re not on one and you’re eligible, talk to your doc. Your future self will thank you.
Also - if you’re still using warfarin because ‘it’s cheaper’ but you’re skipping doses or missing tests? That’s not saving money. That’s gambling with your brain. Just sayin’.
Tori Thenazi
Wait… wait… wait… so you’re telling me that the government and Big Pharma are secretly pushing DOACs because they want us to die in emergency rooms without reversal agents?! I read this article on TruthFeed - it said that Andexxa was pulled from 37 hospitals in 2022 because the FDA knew it caused ‘delayed clotting rebound’! And don’t get me started on ciraparantag - it’s a mind-control chemical disguised as a drug! My cousin’s neighbor’s nurse said she saw a guy turn blue after they gave him Praxbind… and then the hospital covered it up! Why won’t anyone talk about this?! I have a spreadsheet.
Elan Ricarte
Let’s be real - warfarin’s like your ex who still texts you at 2 a.m. ‘Hey, remember when we were cool?’ Nah, bro. We ain’t goin’ back. DOACs are the new GF: low maintenance, no drama, and they don’t ghost you after you eat kale. But here’s the kicker - the real villain ain’t the drug. It’s the insurance companies. They’ll cover apixaban at $5/month… but only if you jump through 14 hoops and submit a notarized letter from your priest. Meanwhile, warfarin’s $4 - but you gotta drive 45 minutes to a clinic that only has one phlebotomist who hates Mondays. So yeah, DOACs win on paper. But in real life? We’re all just stuck in a bureaucratic purgatory where the only thing thinner than our blood is our access to care.
Angie Datuin
Thanks for writing this. I’ve been on rivaroxaban for 3 years and never realized how much I didn’t know about reversal agents. I just assumed if something happened, they’d know what to do. Now I’m kinda nervous. Maybe I should ask my doctor if my hospital has Andexxa. I didn’t even know they were that expensive. That’s wild.
Camille Hall
I’m a nurse in a rural ER, and I’ve seen this play out. We don’t have idarucizumab. We don’t have Andexxa. We have PCC - and we use it anyway. It’s not perfect, but it’s better than nothing. I’ve had patients on DOACs come in with intracranial bleeds, and we’re scrambling to call 3 other hospitals to see if they can send the antidote. It’s not a matter of ‘better drugs’ - it’s a matter of ‘better systems.’ If we’re going to rely on these drugs, we need to make sure every ER - even in places like eastern Kansas - has access. Otherwise, we’re just creating a two-tiered system where city folks live and rural folks gamble.
Ritteka Goyal
OMG I’m from India and we have this problem so bad here - warfarin is like 50 rupees a month but the hospitals don’t even have INR machines in most towns! And DOACs? We can’t even get them without a prescription from a cardiologist in Delhi - and then they cost 3000 rupees! So people just stop taking them. I had a neighbor who had a stroke because he skipped his pills for 3 weeks because he couldn’t afford it. And now he’s paralyzed. Why don’t we make DOACs cheaper? Why don’t we have government subsidies? Why is this even a choice? We need to fix this. This isn’t science - this is survival. And in India, survival means choosing between food and medicine. I cry every time I think about it.
Monica Warnick
So… I’m curious - if DOACs are so much better… why do doctors still prescribe warfarin to so many people? Is it just because they’re lazy? Or is there some secret protocol I don’t know about? I read somewhere that some docs think DOACs are ‘too new’ and don’t trust them… like, what? We’ve had them since 2010. That’s 14 years. My grandma’s had a pacemaker since 2008 and she’s on apixaban. I just… I don’t get it. Are we being lied to? Is there a conspiracy? I need answers.
Ashlyn Ellison
My dad’s on warfarin. He hates it. He’s 78. He skips his INR tests. He eats spinach like it’s a sport. He’s got a 12-page list of ‘things not to take’ taped to his fridge. Last week he had a nosebleed that lasted 45 minutes. We went to the ER. They gave him vitamin K and PCC. He was fine. But I’m not sleeping. I keep thinking - what if next time it’s not just a nosebleed? I’m switching him. No more warfarin. No more tests. No more fear. I’m calling his doctor tomorrow.
Jonah Mann
Just wanted to say - if you’re on a DOAC and you’re worried about bleeding? Don’t panic. Most people never bleed. But if you do, and you’re in a hospital without the antidote? They’ll still use PCC. It’s not ideal, but it works. Also - don’t trust those ‘you need to stop DOACs 24 hours before surgery’ rules. It’s not true for everyone. Ask for an anti-Xa level test. It’s cheap, fast, and tells you if the drug’s still active. Most docs don’t know this. I’m a pharmacist. I’ve corrected 12 people this month. You’re welcome.
Tricia O'Sullivan
I find it profoundly concerning that the discourse around anticoagulation has devolved into a binary choice between cost and convenience, when the underlying imperative should be equity of access. The fact that reversal agents remain inaccessible in 38% of U.S. hospitals is not merely a logistical oversight - it is a moral failure. We must not confuse innovation with inclusion. A drug that saves lives in Boston but condemns patients in Boise is not progress. It is a fracture.
Alex Ogle
I’ve been on warfarin for 12 years. I’ve had 40+ INR tests. I’ve had 3 hospitalizations. I’ve missed birthdays because I had to wait for my INR to be normal. I’ve cried in parking lots after labs. I’ve eaten the same damn salad every week for a decade. And now? Now I’m switching. Not because I’m scared. Not because I’m trendy. But because I’m tired. Tired of being a statistic. Tired of being told ‘just follow the rules’ when the rules change every month. I’m tired of being told I’m lucky I’m alive. I’m not lucky. I’m just done. I’m on apixaban now. No more needles. No more spinach anxiety. Just a pill. And for the first time in over a decade - I feel like I’m living, not just surviving.