Antibiotic-Birth Control Interaction Checker
Check Your Antibiotic Safety
This tool is based on current scientific evidence. Only rifampin has strong proof of reducing birth control effectiveness.
Select an antibiotic to see if it affects your birth control.
The truth about antibiotic interactions with birth control pills is simpler than you think. Most people worry that taking antibiotics like amoxicillin or doxycycline will make birth control fail. But science says otherwise. Only one antibiotic-rifampin-has solid proof of reducing effectiveness. Let’s break down exactly what the research shows.
What Science Says About Different Antibiotics
| Antibiotic | Proven Interaction? | Reason |
|---|---|---|
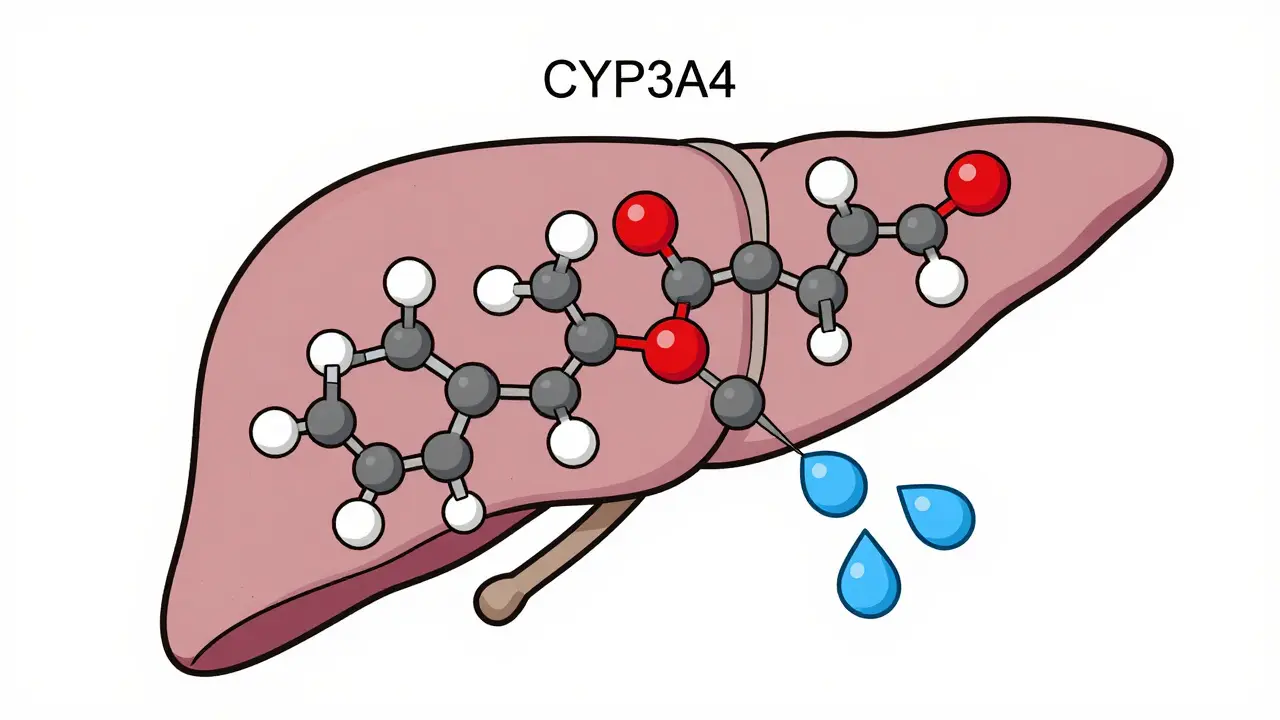
| Rifampin | Yes | Strongly induces CYP3A4 enzymes, reducing estrogen levels by 40-60% |
| Rifabutin | Yes (weaker) | Moderate enzyme induction; 25% reduction in estrogen levels |
| Amoxicillin | No | Multiple studies show no significant hormone changes |
| Doxycycline | No | No impact on birth control hormones in clinical studies |
| Other antibiotics | No | Current evidence shows no clinically relevant interactions |
Oral Contraceptive Pills are hormonal birth control methods containing estrogen and progestin that prevent pregnancy by stopping ovulation and thickening cervical mucus. They’re widely used by over 10 million American women. For decades, doctors warned that antibiotics could make them less effective. But modern research tells a different story.
Back in the 1970s, when birth control pills had high estrogen doses (50-100 mcg), a few case reports suggested interactions. Today’s pills use much lower doses (20-35 mcg), making interactions far less likely. A 2018 review of 1,852 women found pregnancy rates were almost identical between those taking antibiotics and those not-0.69 per 100 woman-years versus 0.54. That’s not statistically significant.
Why Rifampin Is the Exception
Rifampin is an antibiotic used to treat tuberculosis and other infections. It works by inhibiting bacterial RNA synthesis and is the only antibiotic proven to reduce birth control effectiveness. Rifampin speeds up liver enzymes (CYP3A4) that break down estrogen. Studies show it cuts ethinylestradiol levels-ethinylestradiol is the synthetic estrogen in most birth control pills-by 40-60%. This means your body processes the hormones too quickly, leaving you unprotected.
For example, a 1984 study in Contraception found rifampin reduced ethinylestradiol concentrations by up to 60%. Later research confirmed this. The CYP3A4 enzyme is part of the liver’s system for metabolizing drugs is the key player here. When rifampin activates it, birth control hormones get broken down faster than normal.
Other Antibiotics: No Real Risk
Common antibiotics like amoxicillin a penicillin-based antibiotic often used for infections like strep throat or doxycycline a tetracycline antibiotic for acne or respiratory infections don’t affect birth control. A 2003 study in Clinical Pharmacology & Therapeutics tested amoxicillin for 10 days with birth control pills. No significant changes in hormone levels. Similarly, a 2010 study in the British Journal of Clinical Pharmacology found doxycycline had no impact.
Even levonorgestrel a progestin used in some birth control pills and emergency contraception isn’t affected. The 2018 review analyzed 17 studies and found zero evidence that non-rifamycin antibiotics lower progestin levels. Gut flora changes-often blamed for interactions-don’t seem to matter either. Research shows the body quickly recovers from antibiotic-induced gut changes, with no real effect on hormone absorption.
Where the Confusion Comes From
Why do so many doctors still warn about antibiotics and birth control? Historical habits. In the 1970s-1990s, case reports of unintended pregnancies during antibiotic use spread fear. But those reports were flawed. They didn’t control for other factors like vomiting or missed pills. Modern studies are far more rigorous.
Pharmacists also play a role. A 2017 survey found 68% of community pharmacists recommend backup contraception for amoxicillin, even though evidence says not to. Meanwhile, 98% correctly warn about rifampin. This mismatch creates real confusion. A Planned Parenthood survey showed 62% of birth control users use backup during antibiotics unnecessarily.
What Experts Say Now
The CDC Centers for Disease Control and Prevention, which sets medical guidelines for contraceptive use says only rifampin is a Category 4 risk (unacceptable health risk). All other antibiotics get a Category 1 rating (no restrictions). The ACOG American College of Obstetricians and Gynecologists, a leading professional organization for women’s health states clearly: "Only rifampin has been shown to decrease the effectiveness of combined hormonal contraception." The UK’s Faculty of Sexual and Reproductive Healthcare a UK-based organization providing clinical guidance on contraception says it plainly: "There is no evidence for an interaction between combined hormonal contraception and broad-spectrum antibiotics (excluding rifampicin and rifabutin)." The FDA still lists "antibiotics" as potential interactors in pill packaging-without specifics. But in 2022, the FDA Draft Guidance acknowledged these warnings are "misleading and non-evidence-based." The EU updated all birth control labels in January 2023 to remove non-specific antibiotic warnings.

Real-World Impact
This myth costs billions. In the US alone, $147 million is spent yearly on unnecessary emergency contraception purchases due to antibiotic concerns. A 2021 Guttmacher Institute analysis found women buy emergency contraception 30% more often when prescribed antibiotics, even when not needed. This isn’t just expensive-it’s stressful. Imagine paying $50 for Plan B when you didn’t need it.
A 2021 study in Contraception tested evidence-based counseling. When doctors explained the science, unnecessary backup use dropped from 79% to 22%. Pregnancy rates stayed the same (0.8% vs 0.7%). This proves clear communication works.
What You Should Do
If your doctor prescribes rifampin (for TB or certain infections), use backup contraception like condoms for 7 days after finishing the antibiotic. For all other antibiotics-amoxicillin, doxycycline, ciprofloxacin, or anything else-skip the backup. If you get diarrhea or vomiting during antibiotic treatment, that’s when to use backup-not because of the antibiotic itself.
Always talk to your doctor or pharmacist about your specific situation. If they recommend backup for non-rifamycin antibiotics, ask them to check the latest guidelines. You deserve accurate advice.
What’s Next in Research
The NIH is funding a $2.4 million study called ACILE (Antibiotic Contraceptive Interaction Longitudinal Evaluation). They’ll track 5,000 birth control users over three years to get definitive real-world data. Meanwhile, UCSF researchers are studying genetic differences in CYP3A4 enzymes to see if some women might be more vulnerable to interactions.
The EU’s label changes in 2023 set a good example. As evidence piles up, expect more updates to prescribing guidelines. But for now, the message is clear: most antibiotics don’t affect birth control. Only rifampin does.
Does amoxicillin affect birth control pills?
No. Multiple studies, including a 2003 Clinical Pharmacology & Therapeutics trial, found no significant changes in hormone levels when taking amoxicillin with birth control pills. This is true for all penicillin-based antibiotics.
What about doxycycline?
Doxycycline doesn’t affect birth control effectiveness. A 2010 study in the British Journal of Clinical Pharmacology confirmed no meaningful interaction between doxycycline and oral contraceptives. This applies to all tetracycline antibiotics.
Is rifampin the only antibiotic that matters?
Yes. Rifampin is the only antibiotic with strong evidence of reducing birth control effectiveness. It cuts estrogen levels by 40-60% by activating liver enzymes. Rifabutin has weaker effects (25% reduction), but all other antibiotics show no clinically relevant impact.
Why do some doctors still warn about antibiotics?
Historical habits. In the 1970s-90s, case reports of unintended pregnancies during antibiotic use spread fear. But those reports didn’t control for other factors like missed pills or vomiting. Modern studies prove most antibiotics don’t affect birth control. However, outdated advice persists due to ingrained habits and lack of updated training.
Should I use backup if I have diarrhea while on antibiotics?
Yes, but only because of the diarrhea-not the antibiotic. If antibiotics cause severe diarrhea or vomiting, your body might not absorb the birth control pill properly. In that case, use backup contraception for 7 days after symptoms stop. This applies to any medication, not just antibiotics.


Comments
Gregory Rodriguez
Wow, who knew antibiotics and birth control were this simple? Rifampin is the only one that matters. Everyone else is just a myth. But let's be real-doctors still act like it's the 70s. Maybe they should check the latest studies before scaring people into buying unnecessary Plan B. $147 million wasted yearly? That's just ridiculous. But hey, at least we're finally getting some clarity. Science wins again. #NotAllDoctors
Jenna Elliott
Science says nothing but rifampin matters. Doctors still scare people for no reason. It's like they don't care about facts. All this misinformation is dangerous. Stop spreading lies. Facts matter
lance black
Rifampin only. Others? No problem.
Pamela Power
Oh please. The fact that people still believe this myth is proof of how uneducated the general public is. Rifampin is the only antibiotic with proven interaction. Everyone else? Zero evidence. But no, doctors keep peddling outdated nonsense. It's pathetic. This is why we need better science education. Stop being gullible.
anjar maike
Only rifampin matters. Rifabutin has weaker effects but still yes. For others like amoxicillin, no problem. 😊
Cullen Bausman
According to the CDC and ACOG guidelines, only rifampin poses a risk. Other antibiotics do not. This is well-established science. Healthcare professionals must update their knowledge. Misinformation is harmful.
Nancy Maneely
OMG this is such a mess! Doctors still telling people to use backup for amoxicillin. Like wtf? It's not even true! The science says only rifampin matters. But they keep spreading lies. It's so frustrating. People waste so much money on Plan B unnecessarily. This needs to stop. Like, right now. #StopTheMadness
Phoebe Norman
Based on current evidence the interaction between most antibiotics and hormonal contraception is negligible. Rifampin is the exception due to enzyme induction. However the clinical significance varies. It's important to consider individual patient factors. But overall the risk is low for non-rifamycin antibiotics. Further research is needed but current guidelines support this.
Albert Lua
Interesting discussion! As someone from multiple cultures, I've seen this myth spread everywhere. But the science is clear: only rifampin matters. In my country, doctors are starting to update their advice. It's great to see the evidence finally getting through. Let's keep spreading the truth!
Katharine Meiler
From a clinical perspective, the evidence is robust. The 2018 review of 1,852 women showed no statistically significant difference in pregnancy rates between those taking antibiotics and those not. Rifampin is the exception due to its potent CYP3A4 induction, reducing estrogen levels by 40-60%, but all other antibiotics-amoxicillin, doxycycline, ciprofloxacin-have been thoroughly studied with no clinically relevant interactions. The confusion stems from outdated case reports from the 70s-90s that didn't account for missed pills or vomiting, leading to widespread misinformation. Current guidelines from the CDC, ACOG, and the UK's FSRH clearly state only rifampin and rifabutin require backup contraception. The EU's 2023 label updates removing non-specific antibiotic warnings are a step in the right direction. It's crucial for clinicians to educate patients accurately to prevent unnecessary anxiety and financial burden. For instance, a 2021 study in Contraception showed evidence-based counseling reduced unnecessary backup use from 79% to 22% without affecting pregnancy rates. The NIH's ongoing ACILE study will further clarify long-term effects, but for now, the message is clear: most antibiotics don't interfere with birth control. Always consult your provider for personalized advice, but rest assured that standard antibiotics are safe.
Danielle Vila
Oh sure, they say only rifampin matters. But what about all the other antibiotics? The FDA still lists antibiotics as potential interactors, so why are they suddenly saying it's not true? It's a cover-up! Big Pharma is in cahoots with the CDC to keep us in the dark. Think about it-how many times have you heard of someone getting pregnant while on antibiotics? It's not just rifampin. They're hiding the truth. Remember when they said smoking wasn't harmful? Or when they said vaccines cause autism? Now they're saying antibiotics don't affect birth control? It's all a scam. The truth is out there, but the government doesn't want us to know. Always use backup, just in case. Trust me, I've done the research.
Thorben Westerhuys
You're saying amoxicillin doesn't affect birth control. However, case studies and FDA warnings suggest otherwise. This seems oversimplified. Factors like gut flora and different pill types are overlooked. Not just rifampin. I'm concerned.
Lana Younis
Hey y'all, just wanted to chime in. The science is solid: only rifampin and rifabutin really mess with birth control. Like, the CDC and ACOG are on board with this. But you know what's wild? Doctors still tell people to use backup for amoxicillin. It's like they're stuck in the past. I've seen this happen in my own community. People get stressed out and spend money they don't need to on emergency contraception. It's a shame. But the good news is that studies show when doctors explain the facts, people stop using backup unnecessarily. Like, in one study, it dropped from 79% to 22%. That's huge! So maybe we need more education. Also, if you have diarrhea or vomit while on antibiotics, that's when you should use backup-not because of the antibiotic itself. Just a heads-up. Stay safe and informed! Also, the EU updated their labels in 2023 to remove those misleading warnings. The FDA is finally catching up, but it's taken way too long. I hope more healthcare providers get the memo. It's not just about saving money-it's about reducing unnecessary stress. So next time your doctor says to use backup for amoxicillin, ask them to check the latest guidelines. Trust me, it's not a big deal. But yeah, rifampin is the only one to watch out for. #ScienceWins