
When someone is prescribed medication for depression, bipolar disorder, or schizophrenia, the goal is simple: take it as directed. But for many, that’s not what happens. Studies show medication non-adherence affects between 40% and 60% of people with serious mental illness. That’s more than half of those trying to get better. And it’s not because they don’t care. It’s because the system, the medication, and the life they’re living all make it hard to stick with treatment.
Why People Stop Taking Their Mental Health Medication
It’s easy to assume people stop taking meds because they feel fine. But that’s not the whole story. Many stop because of side effects-weight gain, drowsiness, shaking, or feeling emotionally numb. Others don’t believe they’re sick. If you’re hearing voices or feeling deeply hopeless, being told you have a brain disorder can feel like an insult, not help. Dosing frequency is another big factor. If you have to take three pills a day, every day, it’s easy to miss one. Miss one, miss the next. Soon, you’re off the regimen entirely. People with unstable housing, no transportation, or no one to remind them are especially at risk. Homeless individuals with psychiatric conditions have adherence rates as low as 26%-far below the 80% needed for treatment to work. And then there’s cost. A single antipsychotic pill can cost $10 to $30 out-of-pocket. For someone on disability, that’s a meal. Insurance doesn’t always cover it. Even when it does, prior authorizations, pharmacy delays, and copay increases make adherence feel like a full-time job.What Works: The Evidence Behind Real Solutions
Not all interventions are created equal. Some apps send reminders. Some clinics hand out pill organizers. But the data shows only a few approaches move the needle-significantly. The most effective solution? Pharmacist-led care. When pharmacists work directly with psychiatrists and patients, adherence jumps. One 2025 study found patients in a collaborative care model improved their adherence by 142% more than those getting standard care. That’s not a small bump. That’s life-changing. How? These pharmacists don’t just hand out pills. They sit down with patients. They ask: “What’s stopping you from taking this?” They adjust doses. They switch from three pills a day to one long-acting injection. They help patients apply for patient assistance programs. They call pharmacies to make sure the script is filled. They track refills before the patient even misses one. Kaiser Permanente saw a 32.7% increase in adherence in just 90 days after launching a pharmacist-led program. Hospitalizations dropped by 18.3%. That’s not just numbers-it’s people avoiding emergency rooms, staying out of psychiatric units, and keeping their jobs.Simplifying the Regimen Makes a Huge Difference
One pill a day. That’s the sweet spot. A National Alliance on Mental Illness survey found that 87% of patients stayed on track when they had a once-daily dose. Only 52% did when they had multiple daily doses. Yet, 73% of patients said their doctor never even asked if they could simplify their regimen. Long-acting injectables (LAIs) are a game-changer. A 2023 JAMA Psychiatry study showed patients on LAIs had an 87% adherence rate-compared to 56% for oral pills. That’s not magic. It’s logistics. One shot every two weeks means no daily reminders, no pills to lose, no stigma of carrying a pill bottle. The FDA now explicitly promotes LAIs as a tool to improve adherence. And with newer formulations lasting up to three months, the barrier to daily management is almost gone.
Technology Helps-but Only If It’s Used Right
There are apps. Smart pillboxes. Wearables. But most digital tools only help a little. One study found mobile apps improved adherence by just 1.8% for psychiatric meds. That’s barely noticeable. The real value comes when tech is paired with human support. A 2025 Nature Mental Health study used smartphone sensors to track movement, sleep, and voice patterns. The AI predicted when a patient was about to miss a dose-with 82.4% accuracy-up to 72 hours ahead. That’s not surveillance. That’s early warning. When clinicians got that alert, they reached out. Not to scold. To ask: “Are you okay? Can we help?” The result? Adherence improved by 28% in the group that got proactive outreach. The problem? Most digital tools are built for compliance, not connection. If the app just says “Take your pill!” without context, it’s ignored. But if it says, “Your pharmacist noticed you haven’t picked up your med. Can we talk about what’s going on?”-that’s different.The Hidden Barrier: Insurance and Access
Here’s the ugly truth: the best interventions fail if patients can’t access them. A Reddit survey from March 2025 found that 78% of users improved adherence when working with a medication specialist. But 64% said their insurance wouldn’t cover it. Pharmacist consultations? Often not in-network. LAIs? Require prior authorization that takes weeks. Even when approved, patients are told to pick it up at a specialty pharmacy 40 miles away. Medicare and Medicaid are slowly changing. CMS now ties 7 out of 13 quality payments to medication adherence. UnitedHealthcare’s 2025 contracts penalize providers if their patients’ adherence drops below 80%. That’s pushing systems to act. But real change needs more than financial pressure. It needs policy. It needs funding. It needs clinics to hire pharmacists-not as afterthoughts, but as core team members.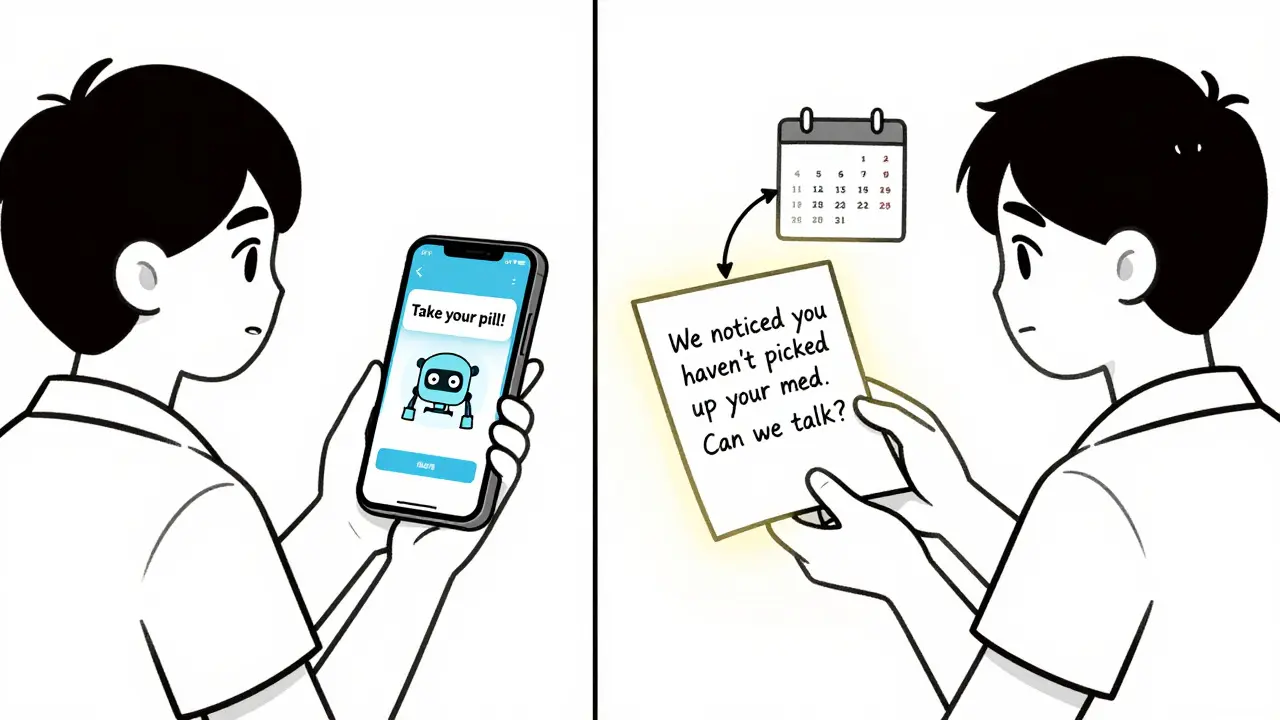
What Patients Need Most: Dignity, Not Dictates
The most effective programs don’t treat adherence like a math problem. They treat it like a human one. They don’t say, “You missed three doses.” They say, “I noticed you haven’t been picking up your med. What’s been going on?” They don’t assume the patient is non-compliant. They assume something’s blocking them. They ask about housing, food, trauma, transportation, stigma. They adjust treatment based on what the patient says-not what the chart says. One patient in Melbourne, who’d been hospitalized six times in two years, finally stabilized after her pharmacist helped her switch from three daily pills to a monthly injection. She didn’t need reminders. She didn’t need lectures. She needed someone who listened.What’s Next: The Future of Adherence
By 2026, Epic’s electronic health records will include real-time adherence analytics. CMS plans to raise the weight of adherence metrics in Medicare Star Ratings from 10% to 15%. The medication adherence tech market will hit $58.7 billion. But none of this matters if we keep treating adherence as a patient problem instead of a system problem. The data is clear: medication non-adherence isn’t about laziness. It’s about complexity, cost, and care gaps. The solutions exist. We just need to scale them. The next time someone says, “Why won’t they take their meds?”-ask instead: “What’s stopping them?” The answer might change everything.Why is medication adherence so low in mental health compared to other chronic illnesses?
Adherence is lower in mental health because the symptoms themselves interfere with treatment. Depression can sap motivation. Psychosis can cause paranoia about pills. Side effects like weight gain or emotional blunting are often more immediate than the vague promise of future stability. Unlike diabetes or hypertension, where physical symptoms are visible, mental illness is invisible-making it easier to deny or dismiss. Plus, stigma and fragmented care make it harder to sustain regular care.
Can switching to a once-daily pill improve adherence?
Yes, dramatically. Research shows 87% of patients stick with a once-daily regimen, compared to only 52% on multiple daily doses. Simplifying the schedule removes logistical barriers-forgetting, misplacing pills, or feeling overwhelmed by the routine. Many patients report feeling more in control when they only have to remember one dose a day.
Are long-acting injectables better than oral pills for adherence?
For many patients, yes. A 2023 study found 87% adherence with long-acting injectables versus 56% with oral pills. Injections eliminate daily dosing, reduce stigma, and ensure consistent blood levels. They’re especially effective for people with unstable routines, memory issues, or who have previously stopped taking pills. While not for everyone, they’re a powerful tool when properly discussed and offered.
How do pharmacists improve medication adherence in mental health?
Pharmacists don’t just dispense pills-they build relationships. They identify barriers like cost, side effects, or transportation. They work with psychiatrists to simplify regimens, switch to injectables, or connect patients with financial aid. Studies show collaborative pharmacist-psychiatrist teams improve adherence by 142% more than standard care. Their role is proactive, personalized, and ongoing-not transactional.
Why don’t more doctors offer simplified dosing or injectables?
Many don’t know the options, or assume patients won’t accept them. Others are pressed for time or lack training in psychiatric pharmacology. Insurance hurdles and administrative delays also discourage providers from switching regimens. But research shows patients often prefer simpler options-when they’re offered. The gap isn’t patient resistance-it’s provider awareness and system support.
Can digital tools like apps fix medication non-adherence?
On their own, not really. Most apps improve adherence by less than 2%. But when combined with human outreach-like a pharmacist calling after a missed dose-they become powerful. The key isn’t the app. It’s the connection. A reminder that says, “We noticed you missed your dose. Want to talk?” is far more effective than one that just says, “Take your pill.”
Is medication non-adherence a personal failure?
Absolutely not. Non-adherence is a system failure, not a personal one. It’s caused by complex factors: cost, side effects, stigma, lack of support, poor communication, and fragmented care. Blaming patients ignores the real barriers. The solution isn’t more guilt-it’s better access, more empathy, and integrated care that meets people where they are.


Comments
tia novialiswati
Just wanted to say this hit home for me 😊 I was on three pills a day for years and kept missing them-not because I didn’t care, but because my life was chaos. Then my pharmacist switched me to a monthly shot. No more pill bottles in my purse, no more guilt. I haven’t been hospitalized in 18 months. Seriously, someone just asking ‘what’s stopping you?’ changed everything. 🥹