When your doctor suspects a heart problem, two tests often come up: cardiac MRI and echocardiography. Both show your heart in detail, but they’re not the same. One uses sound waves. The other uses magnets. One is fast and available in most clinics. The other is slower, more expensive, but gives a level of detail you can’t get anywhere else. So which one do you actually need?
What Echocardiography Can and Can’t Do
Echocardiography, or echo, has been the go-to heart test for over 70 years. It’s the ultrasound of the heart. A technician moves a small device across your chest. It sends out high-frequency sound waves that bounce off your heart and create moving images on a screen. You can see your heart beating in real time - valves opening and closing, walls thickening or thinning, blood flowing through chambers.
It’s cheap. Most places charge between $500 and $1,500. It’s quick - usually under 30 minutes. And it’s everywhere. Even small hospitals and emergency rooms have an echo machine. That’s why over 15 million echocardiograms are done in the U.S. every year.
Normal echo numbers? Left ventricle size between 37-56 mm. Wall thickness 6-11 mm. Ejection fraction (EF) - how well your heart pumps - should be 50-75%. But here’s the catch: echo makes assumptions. It guesses the shape of your heart to calculate volume. If your heart isn’t a perfect oval (and most aren’t), those numbers can be off. A 2023 study in the American Journal of Cardiology found echo measurements were consistently 19% higher than cardiac MRI for wall thickness. That’s not a small error - it can mean misdiagnosing thickening or missing early disease.
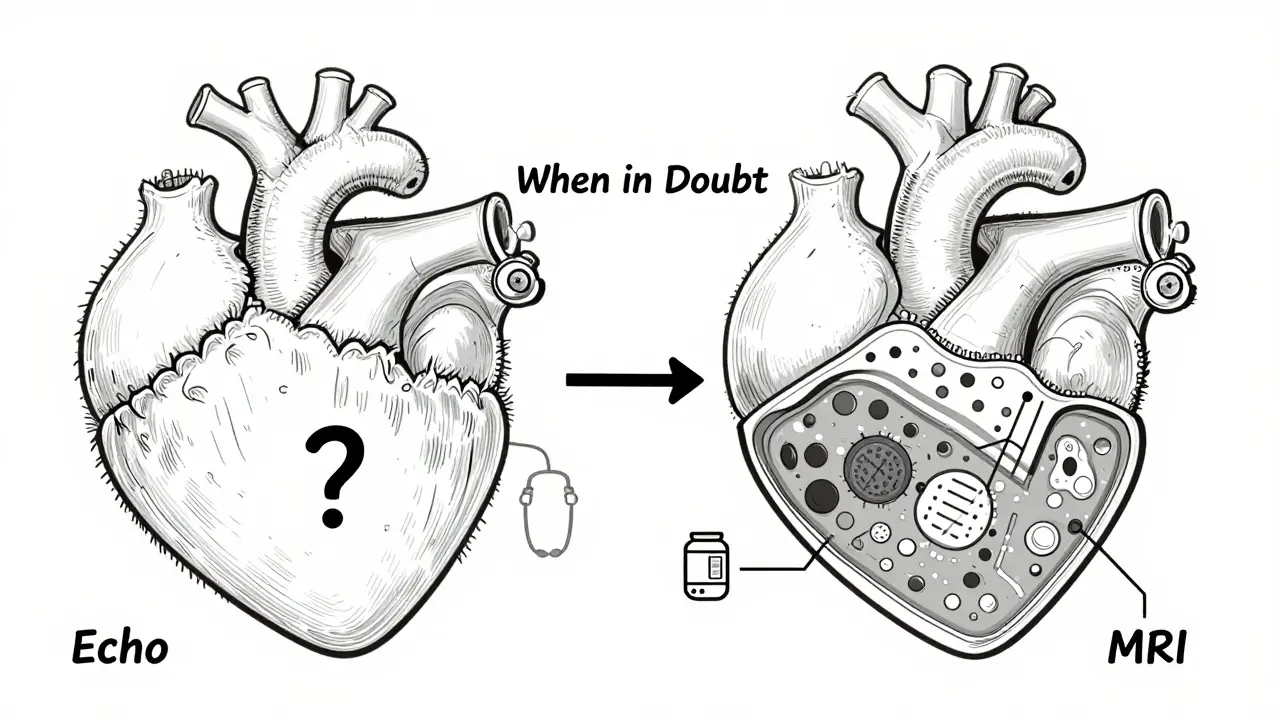
Another issue? Acoustic windows. If you’re overweight, have lung disease, or your ribs block the view, the images get blurry. I’ve seen cases where a patient had a normal echo but still felt terrible. Their heart was actually failing - the echo just couldn’t see it clearly. That’s when MRI steps in.
Why Cardiac MRI Is the Gold Standard
Cardiac MRI doesn’t use sound. It uses a powerful magnet - usually 1.5 to 3 Tesla - along with radio waves to build a 3D picture of your heart. No guessing. No assumptions. It counts every pixel. It measures volume directly, slice by slice. That’s why it’s called the reference standard.
Normal MRI numbers? Left ventricular volume: 67-155 mL for men, 55-105 mL for women. Mass: 49-115 g for men, 37-81 g for women. These numbers are more accurate because MRI doesn’t rely on geometry. It sees the whole thing.
But MRI’s real superpower is tissue. It can spot scar tissue, inflammation, and early fibrosis - things echo can’t touch. Late gadolinium enhancement (LGE) shows where heart muscle has been damaged. In conditions like myocarditis or sarcoidosis, echo might look normal. MRI shows the inflammation before your heart even starts to weaken.
A 2023 study in JACC: CardioOncology found that 2D echo underestimated ejection fraction by 3% on average - and sometimes by as much as 15%. That’s critical for cancer patients. If you’re on chemo that’s hard on the heart, you need to know if your EF is dropping. Echo missed it in 10% of cases. MRI caught it.
Reproducibility? MRI wins again. Inter-observer variability (how much different doctors agree on measurements) is 2.6% for MRI. For echo, it’s 6.8%. That means two cardiologists might give you different EF numbers on echo. On MRI? They’ll likely say the same thing.
When Echo Falls Short - And MRI Saves the Day
Here’s where the real-world difference matters.
One patient I read about had chest pain and shortness of breath. Echo showed normal EF - 60%. But she was exhausted. A cardiac MRI revealed patchy scarring in her heart muscle. She had early myocarditis. She started treatment. Six months later, her symptoms were gone.
Another case: a 52-year-old man with a family history of sudden cardiac death. Echo showed normal walls. MRI showed a thickened septum with fibrosis - classic hypertrophic cardiomyopathy. Without MRI, he’d have been told he was fine. He got an ICD implanted. He’s alive today.
Surveys show 76% of cardiologists use MRI when echo is inconclusive. In academic centers, MRI is standard for diagnosing myocarditis (used in 85% of cases), cardiac sarcoidosis (92%), and before ablation for arrhythmias (76%).
But MRI isn’t perfect. It’s slow. A full scan takes 45-60 minutes. You have to lie still. If you have an irregular heartbeat, it gets harder. Some patients panic in the tube. And if you have a pacemaker, defibrillator, or certain metal implants, you might not be able to have one at all.
Cost, Access, and the Real-World Gap
Cardiac MRI costs $1,500 to $3,500. Echo? Half that. In community hospitals, 78% have echo available the same day. Only 35% offer MRI within a week. Wait times for non-urgent MRI? Often over 14 days. A 2023 survey found 68% of cardiologists in the U.S. had to wait longer than two weeks for a patient’s scan.
That’s why echo still rules. It’s the first step. The screening tool. The emergency tool. If you’re in the ER with chest pain, you get echo. If you’re stable and your echo is unclear? Then MRI.
Technology is closing the gap. New 3D echo systems now match MRI for EF accuracy in many cases. Philips’ EPIQ CVx uses AI to auto-calculate volumes, cutting variability to 4.2%. Siemens introduced a 0.55T MRI in 2023 - low enough to safely scan patients with older pacemakers. That’s a game-changer.
But even with these advances, MRI still leads in tissue detail. No echo system can show fibrosis like LGE. No echo can quantify myocardial strain with the same precision as MRI’s tagging sequences.
What Your Doctor Really Thinks
Dr. Raymond Kwong from Brigham and Women’s says MRI’s low variability makes it superior for tracking heart function over time. If you’re on a drug that affects your heart - like chemo or certain blood pressure meds - you want MRI for follow-ups.
Dr. Susan Joseph from Johns Hopkins puts it bluntly: “Echo tells you the heart is working. MRI tells you why it’s working - or why it’s not.”
But Dr. Michael Chen from the American Society of Echocardiography reminds us: “3D echo has closed the gap. If you have access to it, use it first.”
The truth? It’s not an either/or. It’s a sequence. Echo first. MRI if needed.
Which Test Should You Get?
Here’s a simple guide:
- Get echocardiography if: You’re having symptoms like shortness of breath, fatigue, or palpitations for the first time. You’re being checked after a heart attack. You’re monitoring known valve disease. You’re in an emergency.
- Get cardiac MRI if: Echo was inconclusive. You have unexplained heart failure. You’re being evaluated for myocarditis, sarcoidosis, or inherited cardiomyopathy. You’re on heart-toxic chemotherapy. You’ve had a sudden cardiac arrest with no clear cause. You need precise measurements for surgery or transplant evaluation.
Bottom line: Echo is your starting point. MRI is your deep dive. One isn’t better - they’re complementary. The best care uses both when needed.
What’s Coming Next
By 2030, experts predict hybrid protocols will be standard. Imagine: You get a quick echo in the clinic. It shows something odd. You go to MRI the next day for tissue mapping. The two images are fused. Your doctor sees both structure and scar in one view.
Parametric mapping - measuring T1, T2, and ECV - is already here. It quantifies tissue changes before symptoms appear. In early-stage amyloidosis, MRI can detect protein buildup in the heart wall years before echo shows thickening.
AI is helping both. Automated echo analysis cuts human error. AI-driven MRI reconstruction cuts scan time. The future isn’t choosing one over the other. It’s using them together.


Write a comment