
Sodium isn’t the villain everyone makes it out to be - your body needs a little of it to function. But for more than half of people with high blood pressure, too much sodium is quietly pushing their numbers higher. And it’s not just from the salt shaker. Most of the sodium in your diet comes from packaged foods, restaurant meals, and even bread you think is harmless. The good news? Cutting back doesn’t mean eating bland food. It means eating smarter.
Why Sodium Raises Blood Pressure
When you eat too much sodium, your body holds onto extra water to dilute it. That increases the volume of blood flowing through your vessels. More blood in the same space means more pressure on your artery walls. Your heart has to work harder to pump it all around. Over time, that extra strain stiffens your arteries and damages your blood vessels. Research from the CARDIA-SSBP study in late 2023 showed that just one week of cutting sodium dropped systolic blood pressure by an average of 8 mm Hg in middle-aged and older adults. Even people without high blood pressure saw improvements. About 46% of participants were "salt sensitive," meaning their blood pressure reacted strongly to sodium changes. That’s not rare - roughly half of people with hypertension and one in four with normal blood pressure fall into this group. It’s not just about pressure. High sodium also reduces nitric oxide, a molecule that helps your blood vessels relax. Less nitric oxide means stiffer arteries, worse circulation, and higher risk of heart attack and stroke. The European Society of Cardiology found that cutting sodium by 1.75 grams per day (about 3/4 teaspoon of salt) lowered blood pressure by 4.2/2.1 mm Hg on average. For those with hypertension, the drop was even bigger: 5.4/2.8 mm Hg.Where Most Sodium Really Comes From
You might think you’re eating too much salt because you add it to your food. But here’s the truth: 70 to 75% of the sodium in your diet comes from processed and restaurant foods. That’s right - the bread, canned soup, deli meat, frozen pizza, and even cereal you eat for breakfast are loaded with sodium you never even noticed. A single fast-food burger can have 1,500 mg of sodium. A bowl of canned chicken noodle soup? Up to 1,200 mg. One serving of restaurant pasta with marinara sauce? Often over 1,000 mg. Meanwhile, a homemade meal using fresh ingredients might have just 400 to 600 mg for the whole plate. Even "healthy" options can trick you. A salad with bottled dressing, croutons, and shredded cheese can easily hit 1,200 mg. A "low-fat" yogurt? Sometimes more sodium than full-fat. The FDA now requires nutrition labels to bold the sodium percentage based on a 2,300 mg daily limit. Always check that number - it’s your best tool.Practical Ways to Cut Back - No Taste Sacrifice
You don’t need to give up flavor. You just need to change how you get it.- Read labels like a detective. Look for "sodium" or "salt" in the ingredients. Watch out for hidden names like monosodium glutamate (MSG), sodium benzoate, sodium nitrate, baking soda, and disodium phosphate. Pick products with less than 140 mg per serving - that’s considered low sodium.
- Swap salt for flavor bombs. Use citrus juice, vinegar (balsamic, apple cider, rice wine), garlic, onion, fresh herbs (basil, cilantro, rosemary), spices (cumin, paprika, black pepper), and chili flakes. A squeeze of lemon on grilled fish or a sprinkle of smoked paprika on roasted veggies adds depth without salt.
- Try potassium-based salt substitutes. Products like Mrs. Dash or NoSalt replace sodium with potassium, which helps relax blood vessels. One meal can save you 300-500 mg of sodium. But if you have kidney disease or take certain blood pressure meds, check with your doctor first - too much potassium can be dangerous.
- Choose fresh or frozen without sauce. Fresh vegetables, fruits, lean meats, and plain frozen fish are naturally low in sodium. Avoid anything with "seasoned," "marinated," or "ready-to-eat" on the label. Cook your own sauces - tomato sauce, teriyaki, and salad dressings are easy to make with no salt added.
- Go slow with reduction. Don’t try to cut from 3,500 mg to 1,500 mg overnight. Your taste buds adapt. Start by reducing added salt by 10% each month. After a few weeks, you’ll notice that salty foods taste too strong. That’s your taste buds resetting.
The DASH Diet: Proven to Work
The Dietary Approaches to Stop Hypertension (DASH) diet isn’t a fad - it’s one of the most studied eating plans for lowering blood pressure. It focuses on vegetables, fruits, whole grains, lean proteins, nuts, and low-fat dairy - all naturally low in sodium and high in potassium, magnesium, and fiber. In clinical trials, people following DASH while limiting sodium dropped their systolic blood pressure by 8 to 14 mm Hg. That’s as good as or better than many blood pressure medications. The 2022 OmniHeart Trial showed even better results when you swap some carbs for healthy fats and proteins - like replacing white rice with quinoa and swapping butter for olive oil. You don’t have to go full DASH overnight. Start with one change: swap your morning cereal for oatmeal with berries. Replace your afternoon chips with sliced bell peppers and hummus. Add a serving of spinach to your scrambled eggs. Small steps add up fast.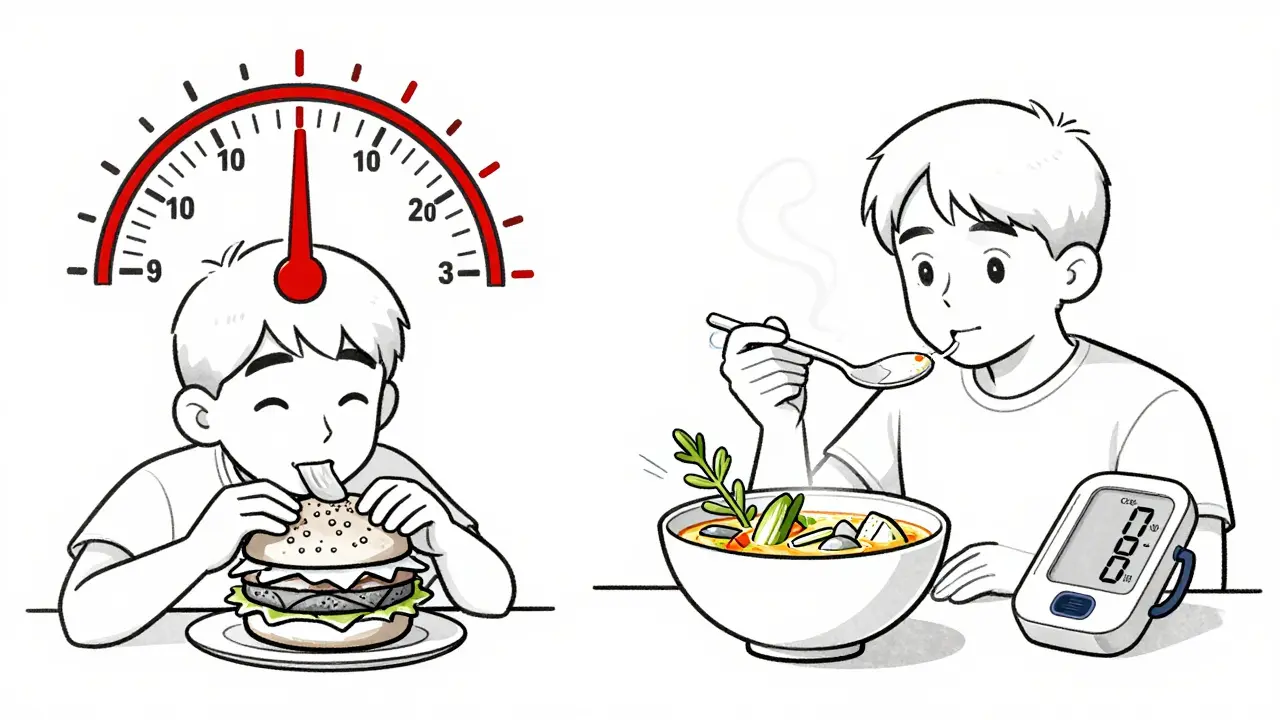
Eating Out Without the Sodium Trap
Dining out doesn’t have to be a sodium minefield. Here’s how to navigate it:- Ask for sauces and dressings on the side. You can control how much you use. This alone can cut 300-500 mg per meal.
- Choose grilled, baked, or steamed over fried. Frying often involves breading soaked in salty solutions. Grilled chicken saves 200-400 mg compared to fried.
- Avoid "healthy" menu traps. Salads with croutons, bacon bits, and processed cheese can have more sodium than a burger. Opt for plain greens with olive oil and vinegar.
- Request no added salt. Most kitchens will honor this. Say "no salt, no soy sauce, no seasoning packets." It’s not rude - it’s your health.
- Split meals or take half home. Restaurant portions are huge, and so is the sodium. You’ll save calories and salt.
What About Potassium?
Potassium helps your body get rid of excess sodium and eases tension in your blood vessel walls. Yet most people don’t get enough. The recommended daily amount is 3,500-5,000 mg. You’d need about 4 bananas, 2 sweet potatoes, a cup of spinach, and a cup of beans to hit that. Focus on whole foods: bananas, oranges, potatoes, tomatoes, beans, lentils, yogurt, salmon, and avocados. A 2022 follow-up of the PREMIER trial found that combining low sodium with high potassium cut systolic blood pressure 7.2 mm Hg more than sodium reduction alone. But if you have kidney disease or take ACE inhibitors, ARBs, or potassium-sparing diuretics, talk to your doctor before increasing potassium. Too much can be dangerous.Real People, Real Results
People who’ve cut sodium report similar stories. One user on Reddit’s r/HighBloodPressure said it took three weeks for their taste buds to adjust. "Now, the food I used to love tastes way too salty," they wrote. Another user tracked sodium for 30 days using the American Heart Association’s app and saw their systolic pressure drop by 6.3 mm Hg on average. The biggest complaints? Cost and time. Fresh food often costs more than processed. Prepping meals takes effort. But many found workarounds: batch-cooking on weekends, using frozen veggies (just check the label), and making big pots of soup or chili to freeze in portions. One week of prep saved 3-4 hours during the week. There’s also a small group - about 5% - who see their blood pressure rise when they cut sodium. This "inverse salt sensitivity" is rare but real. If you’re trying to cut back and your pressure goes up, don’t panic. Talk to your doctor. You might need a different approach.
What’s the Goal?
The American Heart Association says 1,500 mg of sodium per day is ideal. The World Health Organization says no more than 2,000 mg. Most experts agree: even cutting 1,000 mg a day makes a difference. Think of it like this: every 1,000 mg you cut lowers your stroke risk by about 8% and your heart disease risk by 6% over 10 years, according to Dr. Paul Whelton’s research. That’s not just numbers - it’s years of life, better energy, fewer meds, and less worry. You don’t need to be perfect. Just better. Start with one meal. Swap one processed item for a fresh one. Read one label. That’s enough to begin.What About Salt Substitutes and Herbal Salts?
Herbal salts - like garlic salt or onion salt - still contain sodium chloride. They’re just mixed with herbs. They’re not lower in sodium. Same with sea salt, Himalayan salt, or kosher salt. They’re still sodium. The mineral content doesn’t make them healthier for blood pressure. Potassium chloride salt substitutes (like NoSalt or Nu-Salt) are the only ones proven to help lower blood pressure. But again - check with your doctor if you have kidney issues or take certain medications.It’s Not Just About Salt - It’s About Food Quality
Lowering sodium isn’t just a trick. It’s a gateway to eating better overall. When you cut processed foods, you naturally eat more vegetables, fruits, whole grains, and lean proteins. You drink less sugary soda. You cook more at home. You reconnect with real food. That’s the real win. You’re not just lowering blood pressure. You’re building a lifestyle that protects your heart, your brain, your kidneys - your whole body.Can I still eat out if I’m trying to lower my sodium intake?
Yes, but you need to be strategic. Ask for sauces and dressings on the side, choose grilled over fried, skip processed toppings like cheese and croutons, and request no added salt. Many restaurants will accommodate these requests - it’s not unusual anymore. A simple change like swapping a burger for grilled chicken with steamed veggies can cut 800-1,000 mg of sodium from your meal.
How long does it take to see results from reducing sodium?
You can see changes in as little as one week. The CARDIA-SSBP study showed an average 8 mm Hg drop in systolic blood pressure after just seven days on a low-sodium diet. Most people notice a difference in energy and swelling (like puffy ankles or face) within days. Taste buds adapt over 2-4 weeks, and after that, salty foods start to taste overpowering.
Is sea salt or Himalayan salt better than table salt for blood pressure?
No. All types of salt - table, sea, kosher, Himalayan - are made of sodium chloride. They all raise blood pressure the same way. The trace minerals in sea salt or Himalayan salt are too small to make a health difference. If you’re trying to lower sodium, switch to herbs, citrus, or potassium-based salt substitutes instead.
Should I use salt substitutes like Mrs. Dash?
Mrs. Dash and similar herb blends are sodium-free and safe for most people. They’re excellent for flavoring food without adding sodium. But if you’re using potassium chloride substitutes like NoSalt, check with your doctor first - especially if you have kidney disease or take blood pressure meds like ACE inhibitors or spironolactone. Too much potassium can be dangerous in those cases.
What if my blood pressure goes up when I cut salt?
This happens in about 5% of people, called "inverse salt sensitivity." It’s rare but real. It doesn’t mean salt is good for you - it means your body may be reacting to other changes, like dehydration, stress, or medication adjustments. Don’t resume high salt intake. Talk to your doctor. You might need a different approach, like adjusting medications or checking for other health issues.
Next Steps: Start Today
Pick one thing to change this week:- Swap your breakfast cereal for oatmeal with fruit.
- Check the sodium label on your favorite canned soup - pick one with less than 140 mg per serving.
- Make a big pot of vegetable soup or chili with no added salt and freeze portions.
- Keep a bowl of fresh herbs on your counter and use them on everything.


Comments
Jay Ara
i read this and just made a pot of beans from scratch no salt just cumin and garlic. my blood pressure dropped 5 points in 3 days. its not magic its just food that dont fight you
Kuldipsinh Rathod
i used to think salt was the enemy till i started cooking at home. now i use lemon juice and chili flakes and my food actually tastes better. who knew?
Jody Kennedy
this is the most practical guide i’ve read in years. stop overcomplicating it. one swap. one meal. one label. that’s how you win. you got this.
Michael Bond
the potassium point is critical. most people focus on cutting salt but ignore the flip side. your body needs balance, not just deprivation.
david jackson
i spent six months tracking every gram of sodium like a forensic accountant. i started at 4200mg a day. now i’m at 1800. the change wasn’t just in my BP-it was in how i felt waking up. no more brain fog, no more swollen ankles, no more needing a nap after lunch. it’s like my body finally remembered how to breathe. and yeah, i still eat out. but now i ask for no salt, no sauce, no mercy. and guess what? chefs respect it. they’ve seen it all. they’re not offended. they’re impressed.
carissa projo
this isn’t about restriction-it’s about rediscovery. the vibrant tang of lime on grilled fish, the earthy whisper of smoked paprika, the crisp bite of fresh herbs. when you strip away the sodium crutch, you don’t lose flavor-you uncover it. your taste buds aren’t broken, they’re just asleep. wake them up slowly. they’ll thank you with every beat of your heart.
SHAKTI BHARDWAJ
this whole thing is a scam. i cut salt for 2 weeks and my bp went UP. turns out my body hates being controlled. they say 5% of people react inversely but i think its more. they just dont want you to know the truth: your body knows better than some study. why are we all being forced to eat cardboard? i miss salt. i miss flavor. i miss life
Sarah Holmes
Your article is a textbook example of medical paternalism disguised as wellness. You assume everyone has the luxury of time, money, and access to fresh produce. What about single parents working two jobs? What about food deserts? What about the elderly on fixed incomes who rely on canned goods because they can’t carry heavy bags? Your solutions are not practical-they’re performative. And you call this 'empowerment'? It’s elitist. And frankly, insulting.
Matthew Ingersoll
In India, we’ve been doing this for centuries. Masala blends, tamarind, asafoetida, ginger, green chilies-none of it needs salt to sing. My grandmother cooked without a pinch for 60 years. Her BP was perfect. Her food was divine. We didn’t need labels or apps. We had wisdom. Maybe we should look to traditions before we reinvent the wheel.
josue robert figueroa salazar
you think this works? i tried it. lost 10 lbs in a month. turned into a zombie. no energy. depressed. my doctor said my sodium was too low. now i eat salt like its my job. this whole low sodium thing is a cult. you’re not healing. you’re starving your cells.