
Every year, thousands of workers breathe in dust and fibers they never should have touched. By the time they feel the cough, the tightness in their chest, or the breathlessness climbing the stairs, it’s often too late. Silicosis and asbestosis aren’t rare anomalies-they’re preventable tragedies, still happening in 2026 because safety isn’t treated like a priority, but an afterthought.
What Silicosis and Asbestosis Actually Do to Your Lungs
Silicosis comes from breathing in crystalline silica dust. You’ll find it in sand, stone, concrete, and brick. When you cut, grind, or drill these materials-especially without water-the dust becomes airborne. Tiny particles, smaller than a red blood cell, slip deep into your lungs. Your body tries to fight them off. It sends immune cells. They die. More cells come. Over time, scar tissue builds up. Your lungs stiffen. You can’t expand them like you used to. You’re not just out of breath-you’re losing lung function, permanently.
Asbestosis is similar, but the culprit is asbestos fibers. These are long, thin, and sharp. Once inhaled, they don’t break down. They poke into lung tissue and trigger chronic inflammation. The scarring isn’t just on the surface-it spreads through the lung’s structure. People who worked in shipyards, insulation installation, or demolition before the 1980s are most at risk. But even today, asbestos lingers in old buildings. When you’re renovating a 1970s school or tearing down a factory, those fibers can still be released.
Both diseases show up slowly. You might work for 10, 20, even 30 years without symptoms. Then, one day, climbing a flight of stairs leaves you gasping. A doctor runs a scan and finds the scars. By then, the damage is done. There’s no cure. Only management. Only slowing it down.
Why Prevention Works-And Why It’s Still Failing
Here’s the hard truth: we’ve known how to stop these diseases for decades. The tools exist. The science is clear. The regulations are written. But enforcement? Culture? Training? Those are where it falls apart.
Engineering controls are the gold standard. Wet cutting-using water to suppress dust when cutting stone or concrete-cuts silica exposure by 90%. Local exhaust ventilation on power tools pulls dust away before it becomes airborne. Sealing off work areas traps 95% of the particles. These aren’t fancy gadgets. They’re practical, proven, and affordable. A good ventilation system costs $2,000 to $5,000 per workstation. But over 18 to 24 months, it pays for itself in fewer worker’s comp claims, less downtime, and lower insurance premiums.
Yet, in 2021, OSHA cited over 1,000 construction companies for silica violations. Why? Because dry cutting is faster. Because water makes the workspace messy. Because foremen don’t want to slow things down. Because workers are told, ‘Just breathe through it.’
And then there’s PPE-respirators. N-95 masks filter 95% of particles. P-100s? 99.97%. But here’s the catch: they only work if they fit. And if they’re uncomfortable. And if you’re wearing them in 90-degree heat on a roof with no shade. One industrial hygienist on Reddit said compliance drops to 40% in summer. Workers modify them. They tape them. They wear them loose. The CDC found 68% of complaints about respirators were about fit and comfort. That’s not negligence-it’s a system failure.
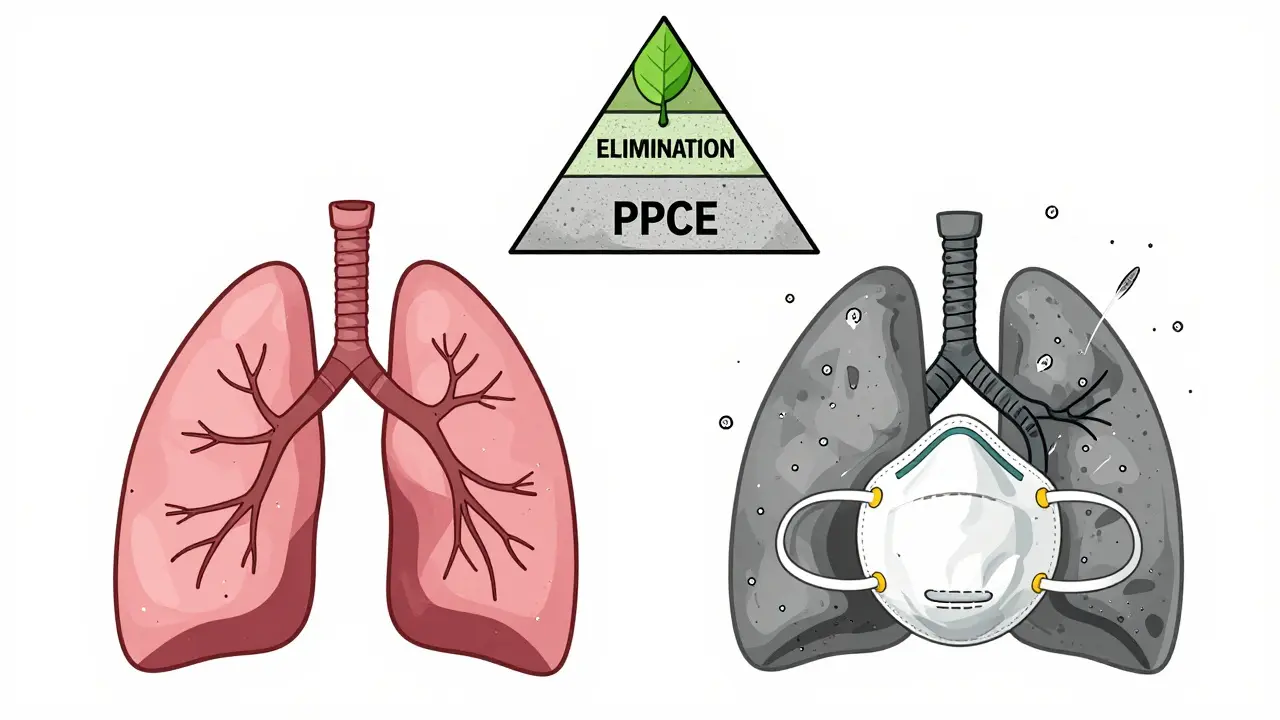
The Hierarchy of Controls: What Actually Saves Lives
There’s a proven order of how to protect workers. It’s called the hierarchy of controls. And it’s not a suggestion-it’s the only logical way to prevent disease.
- Elimination: Don’t use silica or asbestos. Replace concrete with a low-silica alternative. Use fiberglass instead of asbestos insulation. This is the best solution-but rarely done.
- Substitution: Use a safer material. Some newer cutting blades release less dust. Some sealants are asbestos-free.
- Engineering controls: Wet cutting, ventilation, enclosed systems. This reduces exposure by 80-90%.
- Administrative controls: Rotate workers, limit time in dusty areas, schedule high-risk tasks for low-traffic hours. This cuts exposure by 50-70%.
- PPE: Respirators, masks, goggles. Only 40-60% effective if used perfectly-and most aren’t.
Too many workplaces stop at PPE. They hand out masks and call it a day. That’s not safety. That’s luck.
Who’s at Risk-and Who’s Being Left Behind
Construction workers. Miners. Tile installers. Demolition crews. Auto mechanics. Even landscapers who use sand or crushed stone. These aren’t niche jobs. They’re everywhere.
But the biggest gap? Small businesses. In Wisconsin, 78% of companies with fewer than 20 employees didn’t have a proper respiratory protection program. Why? No safety officer. No budget. No time. But here’s the thing: OSHA doesn’t care how big you are. If you’re exposing workers to silica or asbestos, you’re breaking the law.
And it’s not just about new workers. The average construction worker is now over 55. Many have asthma, COPD, or old injuries. Exposure hits them harder. Their lungs are already worn down. One more breath of dust can tip them into irreversible decline.
What You Can Do-Even If You’re Not a Boss
You don’t have to be in charge to make a difference.
- Ask for wet cutting. If you’re cutting stone or concrete, demand water. If they say no, ask why. Document it.
- Get fit tested. If you’re given a respirator, insist on a proper fit test. OSHA requires it annually. If you haven’t had one in two years, you’re not protected.
- Report unsafe conditions. OSHA’s whistleblower program protects you. You can report anonymously. If your coworker is coughing after a day of dry cutting, speak up. It could save their life.
- Don’t smoke. Smoking increases your risk of developing silicosis or asbestosis by 50-70%. If you’re exposed to dust and you smoke, you’re doubling your risk. Quitting isn’t just good for your lungs-it’s essential for survival.
Monitoring: Catching It Before It’s Too Late
Doctors can’t reverse scarring. But they can catch it early.
Spirometry-a simple breathing test-is the key. It measures how much air you can push out and how fast. If your lung function drops over time, it’s a red flag. The American Thoracic Society says testing every five years is the minimum. For high-risk workers? Annually. If you’ve been working with dust for more than five years and haven’t had a spirometry test, you’re flying blind.
Early detection doesn’t cure silicosis or asbestosis. But it can slow progression by 30-50%. That’s not just a number. That’s years of breath. Years of walking without gasping. Years of playing with your grandkids without stopping for air.
The Bigger Picture: A Movement, Not Just a Rule
The European Respiratory Society wants to eliminate occupational lung diseases by 2030. NIOSH just launched a free digital tool called ‘Prevent eTool’-it gives step-by-step guidance for 15 high-risk industries. Companies using it saw a 40% drop in respiratory incidents in six months.
This isn’t about regulation. It’s about dignity. No one should lose their ability to breathe because their job didn’t protect them. We have the tools. We have the data. We have the knowledge.
What’s missing is the will.
It’s not enough to say, ‘We follow the rules.’ You have to live them. Every day. In every job. In every worksite. In every breath.
Can you get silicosis from one exposure to silica dust?
No, silicosis doesn’t happen from a single exposure. It develops over years of repeated inhalation of silica dust. But acute silicosis can occur after intense exposure over weeks or months-like in sandblasting without protection. Even then, it’s rare. The real danger is chronic exposure-working with silica for 10, 15, or 20 years without proper controls.
Is asbestos still used today?
In the U.S., asbestos isn’t banned, but its use is heavily restricted. It’s still found in older buildings-homes, schools, factories built before 1980. Some products, like brake pads or roofing materials, can still legally contain small amounts. The real risk isn’t new asbestos-it’s disturbing old asbestos during renovation, demolition, or repair work.
Are N-95 masks enough for silica or asbestos?
N-95 masks filter 95% of particles, which is better than nothing. But for high-risk tasks like cutting concrete or removing old insulation, P-100 respirators are the standard. They filter 99.97% of particles, including oil-based ones. N-95s are fine for low-risk, occasional exposure-but not for daily work with dust or fibers.
How often should workers get lung function tests?
At least every five years for workers exposed to silica or asbestos. But if you’re working in high-risk roles-like demolition, mining, or stone cutting-annual testing is recommended. Workers with existing lung conditions should be tested yearly, no exceptions. Early detection is the only way to slow down the damage.
Can you sue your employer if you develop silicosis or asbestosis?
Yes, in many cases. Workers’ compensation usually covers medical costs and lost wages. But if your employer knowingly ignored safety rules, hid exposure risks, or didn’t provide proper training or equipment, you may have grounds for a personal injury lawsuit. Many cases have been won against companies that cut corners on dust control or failed to provide respirators.
What’s the difference between silicosis and COPD?
COPD is usually caused by smoking or long-term air pollution. It affects the airways and air sacs. Silicosis is caused by inhaling silica dust and causes scarring deep in the lung tissue. The symptoms feel similar-shortness of breath, cough-but the damage is different. Silicosis shows up on scans as dense, round scars. COPD shows up as enlarged air sacs and narrowed airways. They can also happen together, especially in smokers exposed to dust.
Is there a safe level of asbestos exposure?
No. The International Agency for Research on Cancer (IARC) states there is no safe level of asbestos exposure. Even a single fiber can potentially cause harm over time. That’s why the only safe approach is to eliminate exposure entirely-not reduce it. Any asbestos removal must be done by licensed professionals using sealed containment and negative air pressure.
What should I do if I think I’ve been exposed to silica or asbestos?
Stop the exposure immediately. Get a medical evaluation, including a chest X-ray and spirometry test. Tell your doctor exactly what you did, how long, and whether you wore protection. Keep records of your job history and any safety training you received. If you’re still working in the same environment, demand better controls. Don’t wait for symptoms. By then, it’s often too late.
What Comes Next
If you’re a worker: speak up. Ask for wet cutting. Ask for fit testing. Ask for training. You have rights.
If you’re a supervisor: don’t just hand out masks. Model the behavior. Wear your PPE. Use the ventilation. Make safety non-negotiable. Your team will follow.
If you’re in management: invest in controls, not just compliance. The cost of a respirator is pennies compared to the cost of a worker’s life-or a lawsuit.
These diseases aren’t inevitable. They’re choices. And we’ve made the wrong ones for too long.


Comments
Carolyn Whitehead
Been a tile setter for 18 years and I still remember the first time I saw a guy cough up blood after a dry cut job. We didn’t even have masks back then just dust in our eyes and lungs
Now I wet cut everything even if it slows me down a bit. Better than ending up like my old boss who couldn’t climb his own stairs at 52
Diksha Srivastava
India has the same problem everywhere brick kilns and stone crushers with zero protection and workers breathing through cloth rags
My uncle worked in one for 25 years and now he’s on oxygen at 58. It’s not just America this is global
Sarah Blevins
According to OSHA data from 2023 there were 327 confirmed cases of silicosis in the US alone with an additional 142 suspected cases where documentation was incomplete. The underreporting rate remains high due to lack of routine spirometry and employer pressure to avoid diagnosis. This is not a safety issue it is a systemic failure of occupational health surveillance.
Jason Xin
Yeah and the funniest part is companies buy N-95s by the pallet then hand them out like candy and call it compliance
Meanwhile the same foreman who handed you that mask last week is still dry cutting concrete because ‘it’s faster’
It’s not ignorance it’s deliberate negligence dressed up as efficiency
Yanaton Whittaker
AMERICA IS STILL LETTING THIS HAPPEN???
WE HAVE THE TECHNOLOGY THE LAWS THE KNOWLEDGE
IF YOU’RE NOT DOING WET CUTTING YOU’RE NOT JUST LAZY YOU’RE A CRIMINAL
PUT THESE GUY’S NAMES ON TV AND SHAME THEM
USA STRONG!! 🇺🇸💪
Kathleen Riley
The ontological underpinnings of occupational safety are fundamentally contingent upon the epistemological privileging of capital over corporeal integrity. The human body is rendered as a disposable substrate within the neoliberal labor regime wherein respiratory health is subordinated to throughput metrics and profit margins. The persistence of silicosis and asbestosis is not an accident but a structural inevitability of late-stage industrial capitalism.
Donna Fleetwood
My dad was a demolition guy in the 80s and he never talked about it until he got diagnosed
But now I make sure my crew uses wet cutting and I check their respirator fit every Monday
It’s not about being perfect it’s about showing up and caring
And yeah I bring snacks too because nobody likes a mask that makes them hungry
Sazzy De
Just had my annual spirometry test last week
My numbers are still good
But I’m not taking any chances
Wet cut every time no matter what they say
And I’ve started asking coworkers if they’ve been tested too
Small things add up
Gaurav Meena
Here in India we don’t even have proper respirators in most places
But I started training my team on the basics - wet cutting even with a bucket of water
One guy said ‘it’s too much work’
I told him ‘your lungs are not disposable’
Now he does it without being asked
Change starts with one person
Jodi Olson
There is no such thing as a safe exposure. There is only denial dressed as pragmatism.
The body does not negotiate. It does not compromise. It does not understand ROI.
Scarring is not reversible. Breath is not renewable.
We have known this for a century.
And yet we still choose convenience over survival.
What does that say about us?