Tretinoin vs Topical Alternatives Calculator
Your Skin Profile
Recommended Option
Key Takeaways
- Tretinoin 0.025% offers the strongest clinical evidence for both acne and anti‑aging, but it also carries the highest irritation risk.
- Adapalene 0.1% is a gentler retinoid ideal for beginners and sensitive skin.
- Tazarotene 0.05% works faster on severe acne but can be harsh and is prescription‑only.
- Retinol and over‑the‑counter alternatives (azelaic acid, niacinamide) provide milder results with fewer side‑effects.
- Choosing the right product depends on skin type, concern, tolerance, and budget.
What Is Tretinoin 0.025%?
When you see Tretinoin 0.025% is a prescription‑strength topical retinoid derived from vitamin A. It works by binding to retinoic acid receptors (RAR‑β and RAR‑γ) in the skin, accelerating cell turnover, reducing keratin plug formation, and stimulating collagen synthesis. The 0.025% concentration is the lowest approved dose in many markets, designed to balance efficacy with tolerability.
Because it directly supplies the active form of retinoic acid, it bypasses the conversion steps required by milder retinoids like retinol. This makes it especially powerful for treating comedonal acne, reducing fine lines, and improving overall texture.
How Tretinoin Stacks Up Against Other Retinoids
Not all retinoids are created equal. The main differences lie in three areas:
- Potency - how strongly the molecule activates retinoic acid receptors.
- Conversion pathway - whether the product is already active (like tretinoin) or needs to be metabolized (like retinol).
- Formulation - creams, gels, or microsphere‑based systems that affect absorption and irritation.
Below is a snapshot of where the most common alternatives sit on those axes.
Alternative Topical Options
Each alternative brings a unique mix of effectiveness, side‑effects, and cost. Here’s a quick rundown.
- Adapalene 0.1% - a synthetic retinoid with a focus on anti‑inflammatory action. Available OTC in many countries.
- Tazarotene 0.05% - a third‑generation retinoid approved for both acne and psoriasis. Prescription‑only.
- Retinol (0.5%‑1%) - the over‑the‑counter cousin of tretinoin. Needs two‑step conversion to become active.
- Azelaic Acid 15% - a dicarboxylic acid that normalizes keratinization and reduces inflammation. Often used for rosacea and mild acne.
- Benzoyl Peroxide 2.5%‑5% - not a retinoid but a common acne partner that kills P. acnes bacteria.
- Salicylic Acid 2%‑5% - a beta‑hydroxy acid that exfoliates inside pores.
- Vitamin C (L‑Ascorbic Acid) 10%‑20% - antioxidant that brightens skin and supports collagen.
- Niacinamide 4%‑10% - a form of vitamin B3 that reduces redness and strengthens the barrier.
- Hydroquinone 2%‑4% - a depigmenting agent for hyperpigmentation, often paired with retinoids.
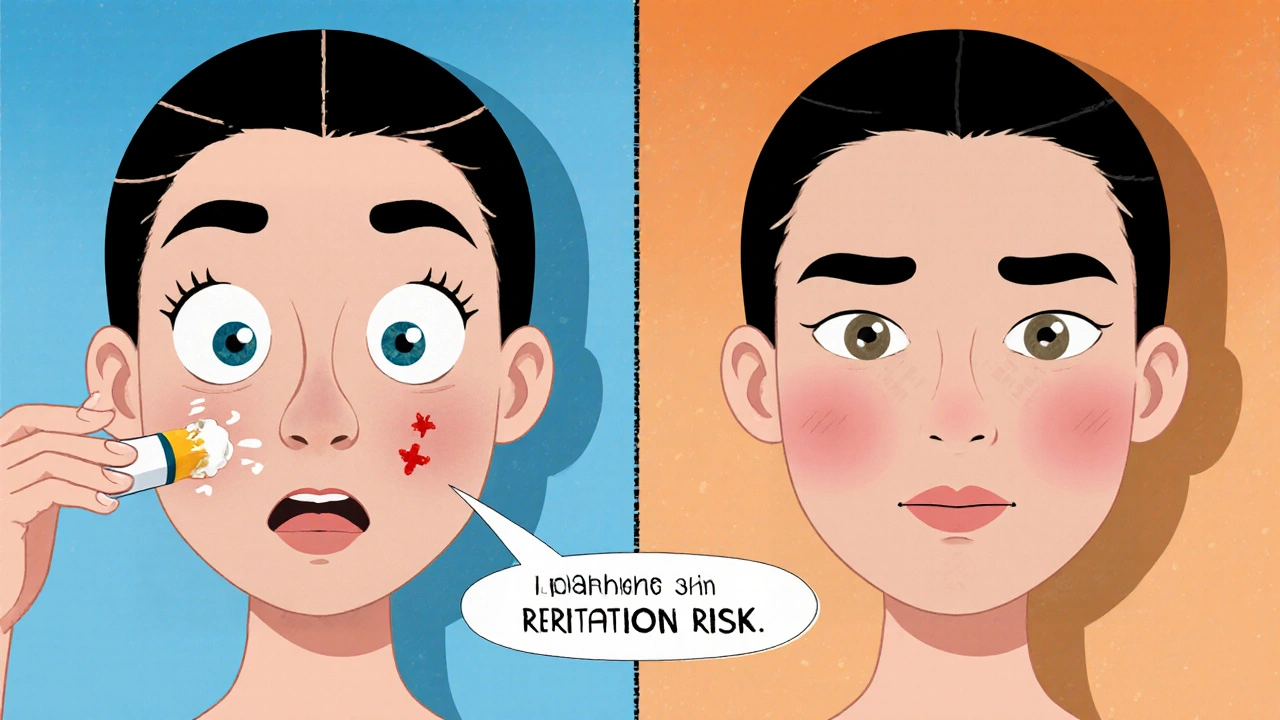
Side‑Effect Profile Comparison
Understanding irritation risk is key because it dictates how quickly you can see results.
| Product | FDA Status | Mechanism | Typical Use | Strength (Typical) | Irritation Risk | Cost (AU$ per month) |
|---|---|---|---|---|---|---|
| Tretinoin 0.025% | Prescription | Direct retinoic acid receptor agonist | Acne, anti‑aging | 0.025% | High (dryness, peeling) | 30‑45 |
| Adapalene 0.1% | OTC (US) | Selective RAR‑β agonist, anti‑inflammatory | Mild‑moderate acne | 0.1% | Moderate (mild redness) | 15‑25 |
| Tazarotene 0.05% | Prescription | Pan‑retinoic acid receptor agonist | Severe acne, psoriasis | 0.05% | Very high (severe peeling) | 45‑70 |
| Retinol 0.5%‑1% | OTC | Vitamin A precursor, two‑step conversion | Anti‑aging, light acne | 0.5%‑1% | Low‑moderate | 20‑35 |
| Azelaic Acid 15% | Prescription/OTC (varies) | Keratinization normalizer, antimicrobial | Acne, rosacea, hyperpigmentation | 15% | Low (minimal irritation) | 25‑40 |
Decision Criteria: Which Product Fits Your Needs?
Use the following checklist to narrow down the best choice.
- Skin sensitivity - If you’ve struggled with redness or eczema, start with adapalene or azelaic acid.
- Desired speed of results - Tazarotene and tretinoin show visible improvements in 4‑6 weeks; retinol may take 8‑12 weeks.
- Prescription access - If you can’t get a script, opt for OTC retinol, adapalene, or azelaic acid.
- Budget - OTC options stay under $35/month, while prescription retinoids often exceed $45.
- Target concern - For pure anti‑aging, tretinoin or tazarotene are top; for hyperpigmentation, combine azelaic acid or hydroquinone with a mild retinoid.
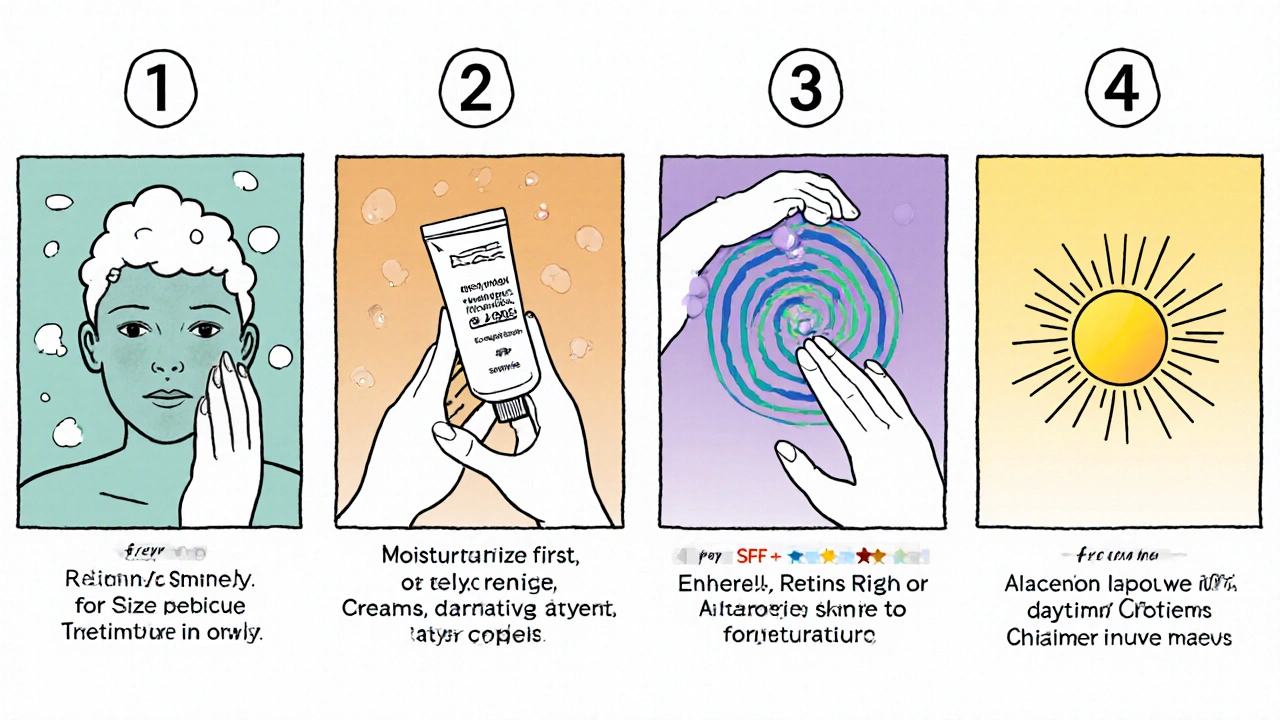
Practical Tips for Using Tretinoin 0.025% and Its Alternatives
- Start slow - Apply a pea‑size amount every other night for the first two weeks.
- Moisturize first - A barrier‑supporting cream (e.g., ceramide‑rich) before the retinoid reduces peeling.
- Sun protection - Broad‑spectrum SPF 30+ is non‑negotiable; retinoids increase photosensitivity.
- Avoid harsh actives - Skip benzoyl peroxide or high‑strength AHAs on the same night.
- Adjust frequency - If irritation spikes, revert to twice‑weekly application before gradually increasing.
These steps work for tretinoin, adapalene, and tazarotene alike. For milder options like retinol or azelaic acid, you can often move to nightly use sooner.
When to Seek Professional Help
If you notice any of the following, book a dermatologist appointment:
- Severe peeling that cracks or bleeds.
- Persistent redness lasting more than two weeks.
- Unexpected darkening of patches (possible post‑inflammatory hyperpigmentation).
- Signs of infection (pus, swelling, warmth).
Clinicians can prescribe lower‑strength formulations, add topical steroids for short‑term calming, or suggest adjunct therapies like chemical peels.
Mini FAQ - Your Burning Questions Answered
Is tretinoin 0.025% safe for daily use?
Most dermatologists recommend starting every other night and only moving to daily use after the skin builds tolerance. Daily use can be okay for seasoned users but always pair with moisturizer and sunscreen.
Can I combine tretinoin with benzoyl peroxide?
It’s better to separate them: use benzoyl peroxide in the morning and tretinoin at night, or alternate nights. Mixing can inactivate both ingredients and increase irritation.
How long does it take to see results with tretinoin?
Visible improvement in acne usually appears after 4‑6 weeks, while anti‑aging benefits (fine line smoothing) become noticeable around 8‑12 weeks.
Is adapalene as effective as tretinoin for anti‑aging?
Adapalene is primarily an acne work‑horse. It does improve texture, but its collagen‑boosting effects are milder than tretinoin’s. For dedicated anti‑aging, tretinoin or tazarotene remain the gold standard.
Can pregnant women use any of these retinoids?
No. Oral and topical retinoids, including tretinoin, adapalene, and tazarotene, are classified as category C or D for pregnancy. Stick to safer options like azelaic acid under medical guidance.
Next Steps - Tailor Your Routine Today
1. Assess your skin’s current tolerance level.
2. Choose a product from the table that matches your concern and budget.
3. Follow the starter protocol (alternate nights, moisturizer first, SPF daily).
4. Track progress in a simple diary - note redness, dryness, and any breakouts.
5. After 4‑6 weeks, decide if you can increase frequency or need to switch to a milder alternative.
Remember, the best retinoid is the one you can use consistently without burning out your skin.


Comments
dennis turcios
Tretinoin is overhyped; most people would be better off with a simple niacinamide regimen.
Felix Chan
Hey, I get the skepticism, but a low‑dose tretinoin can be a game‑changer for stubborn acne when you pair it with a good moisturizer. Start slow and you’ll probably see fewer breakouts without the drama.
Thokchom Imosana
The pharmaceutical industry has been quietly steering dermatologists toward prescription‑only retinoids like tretinoin and tazarotene under the guise of “clinical superiority.” What most consumers don’t realize is that the same companies own the majority of the over‑the‑counter market for retinol, niacinamide, and even azelaic acid. This creates a feedback loop where the most profitable products are constantly marketed as the “gold standard,” while cheaper, safer alternatives are downplayed. If you dig into the FDA approval dossiers, you’ll see that the safety data for low‑dose tretinoin is barely more robust than the data for high‑quality retinol serums. Moreover, the “prescription‑only” label is often a relic of an old patent strategy designed to lock out generic competition. In practice, dermatologists are incentivized to write a script because they receive a marginal rebate from the manufacturer. The result is that many patients are exposed to unnecessary irritation, peeling, and the dreaded post‑inflammatory hyperpigmentation that could have been avoided with a gentler regimen. Meanwhile, the same skin‑care giants are funding research that glorifies “rapid turnover” as the holy grail of anti‑aging. They publish glossy studies showing statistically significant improvements within six weeks, but those studies rarely account for the long‑term barrier damage caused by chronic irritation. The narrative is reinforced by influencer marketing, where “my dermatologist prescribed me tretinoin” becomes a badge of authenticity. Yet the influencers themselves are often paid to promote these products, blurring the line between genuine endorsement and paid advertisement. If you ask a dermatologist who isn’t tied to a pharmaceutical rep, many will recommend starting with a well‑formulated retinol or adapalene to gauge tolerance. The underlying chemistry tells the same story: retinol must be converted to the active form, which actually mimics the body’s natural pathway and tends to be gentler on compromised skin barriers. So before you jump on the prescription bandwagon, consider whether the perceived “fast results” are worth the hidden costs. In the end, a critical consumer should read the fine print, question the incentives, and remember that the best retinoid is the one you can use consistently without burning out your skin.
Latasha Becker
From a pharmacodynamic perspective, tretinoin exhibits a higher affinity for the RAR‑β and RAR‑γ isoforms, which accounts for its superior collagen‑inducing potential relative to adapalene. However, the associated increase in keratinocyte turnover also predisposes to transepidermal water loss, especially in individuals with compromised barrier function. Clinical guidelines therefore stratify patients based on the Fitzpatrick scale and baseline erythema index before initiating therapy. In contrast, azelaic acid operates via inhibition of tyrosinase and modulation of inflammatory mediators, offering a markedly lower irritancy profile. It is worth noting that the half‑life of topical tretinoin on the stratum corneum is approximately 6‑8 hours, necessitating consistent nightly application to maintain therapeutic concentration. For patients with a history of rosacea, the concomitant use of a ceramide‑rich emollient can mitigate barrier disruption. Moreover, studies have demonstrated that a bi‑weekly tapering schedule can reduce the incidence of post‑inflammatory hyperpigmentation in phototypes III–VI. Ultimately, the therapeutic index hinges on a delicate balance between efficacy and tolerability, underscoring the importance of individualized regimen design.
parth gajjar
Okay I get the science but seriously this whole “tolerability” debate feels like a soap opera for your face you’re basically telling people to suffer for the glow and it’s exhausting the skin cries out for mercy yet we’re sold the nightmare of peeling like it’s a badge of honor
Maridel Frey
When selecting a retinoid, it is essential to assess both the patient’s dermatologic objectives and their skin’s adaptive capacity. For newcomers, starting with a low‑strength adapalene or a high‑quality retinol formulation can provide meaningful improvements while minimizing adverse reactions. Encourage the use of a barrier‑supporting moisturizer applied prior to the active ingredient, and emphasize unwavering daily sunscreen use to protect against photosensitivity. Tracking parameters such as erythema, desquamation, and lesion count in a simple journal can guide incremental frequency adjustments. This systematic approach promotes sustainable results and fosters confidence in the therapeutic process.
Madhav Dasari
Yo totally vibe with that-just remember to keep the routine chill, like slap on a dab of moisturizer before the retinoid and never skip SPF, even if you’re just chilling at home. If your skin starts acting up, back off a day and you’ll be back on track before you know it.
DHARMENDER BHATHAVAR
In summary, the optimal retinoid choice aligns with the patient’s clinical priority, tolerance threshold, and access to prescription resources; a structured initiation protocol and diligent photoprotection are indispensable components of any regimen.