For years, doctors have told people with high blood pressure to aim for 120/80 - the number that’s been stamped into public health posters, doctor’s office charts, and even fitness trackers. But if you’ve walked out of a clinic lately wondering whether that number still applies to you, you’re not alone. The truth is, the old one-size-fits-all target is fading fast. Today, the debate isn’t whether 120/80 is good - it’s whether it’s right for everyone.
Why 120/80 Got So Popular
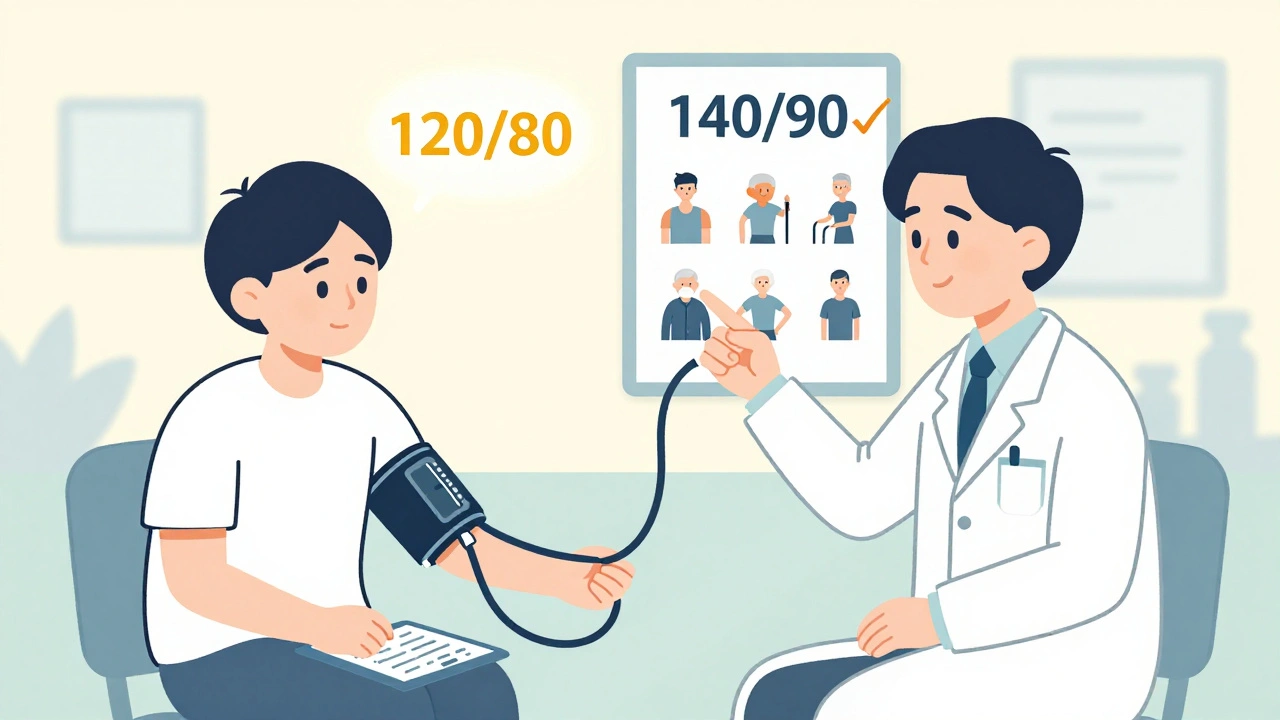
The 120/80 mm Hg target didn’t come out of nowhere. It’s the cutoff that separates normal blood pressure from elevated, according to the American Heart Association and American College of Cardiology’s 2017 guidelines. That’s when they redefined what counts as high blood pressure. Before that, 140/90 was the line. Now, anything above 130/80 is stage 1 hypertension - and that means millions more people are being told they need to do something. The push for lower numbers came largely from the SPRINT trial in 2015. This study followed nearly 9,400 adults without diabetes or stroke history, randomly assigning them to either a strict target of under 120 mm Hg systolic or the standard under 140 mm Hg. The results were striking: those who hit the lower target had 25% fewer heart attacks, strokes, and heart failure events - and 27% fewer deaths over just under four years. It was a game-changer. Hospitals, clinics, and even insurance companies started treating 120/80 like a goalpost you had to cross. But here’s the catch: SPRINT didn’t include people over 75 with multiple health problems, those with a history of falls, or people with diabetes. In other words, it didn’t reflect most real-world patients. So when guidelines started pushing 120/80 for everyone, primary care doctors began seeing more dizziness, fainting, kidney issues, and falls - especially in older adults.The Backlash: Why Some Experts Say 140/90 Is Still Fine
The American Academy of Family Physicians (AAFP) took a hard look at the data in late 2022 and came to a different conclusion. They found that lowering systolic pressure below 140 mm Hg didn’t significantly reduce deaths - but it did increase side effects. For every 33 people treated to get below 120 mm Hg, one would experience a serious problem like fainting, low blood pressure, or kidney trouble. Their recommendation? Stick with 140/90 as the primary target for most adults. They argue that the benefits of going lower are small - for example, you’d need to treat 137 people for nearly four years just to prevent one heart attack. Meanwhile, the cost and complexity go up. People need more medications, more doctor visits, more blood tests. For someone managing diabetes, arthritis, and depression on five pills a day, adding another medication just to shave off 10 points from their systolic number isn’t always worth it. The AAFP doesn’t say 120/80 is bad. They say it’s not always necessary. After you’ve brought your blood pressure down to 140/90, they suggest having a conversation: Do you feel fine? Are you on one pill? Is your kidney function stable? Then maybe we don’t need to push lower. This is shared decision-making - not a lack of care, but a smarter kind of care.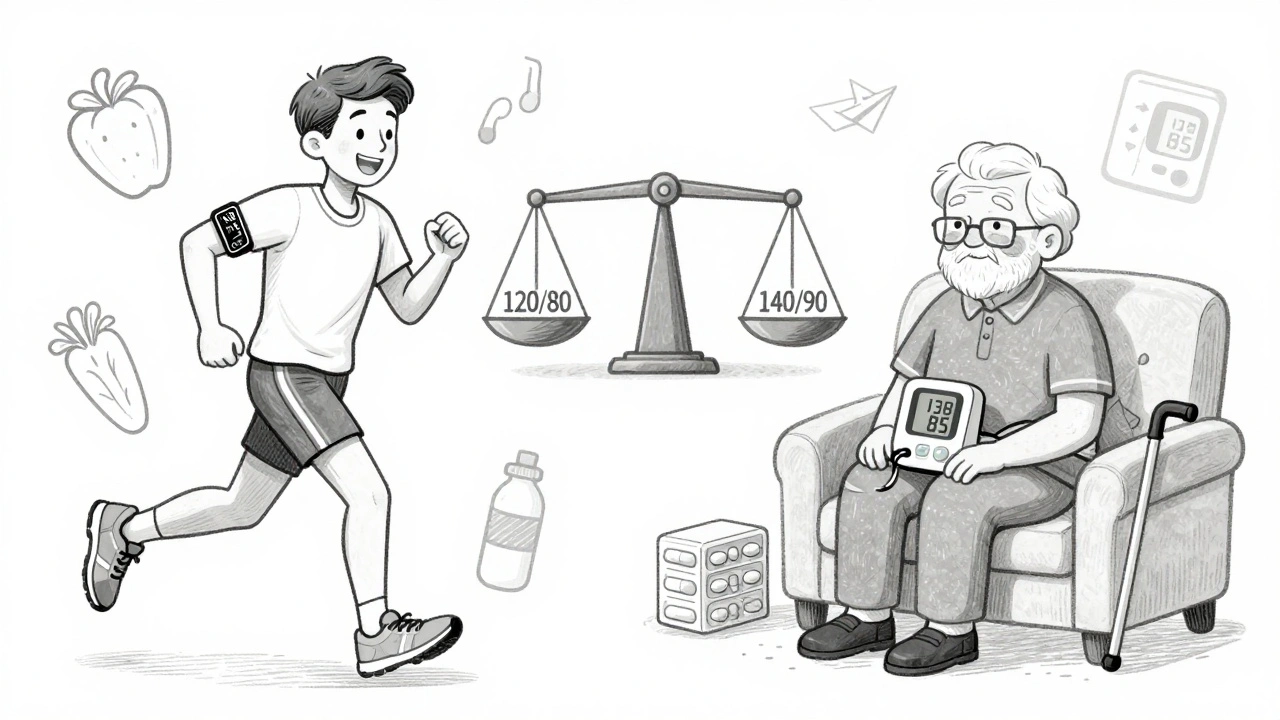
Where the World Stands Now
Global guidelines are all over the map - and that’s telling. In Japan, the 2025 guidelines dropped the old 140/90 target for seniors and now say everyone - young or old, healthy or frail - should aim for under 130/80. Their reasoning? A massive analysis of over 1 million patients showed that every 5 mm Hg drop in systolic pressure reduces heart events by 10%, no matter your age. They’re betting that better monitoring - more frequent check-ins, home devices, and faster lab results - makes aggressive targets safer than ever. Europe’s approach is more nuanced. The European Society of Hypertension says: under 129/79 for people under 65, under 139 for those 65 to 79, and under 150 for those over 80. They’re not ignoring risk - they’re adjusting for tolerance. Older bodies handle pressure changes differently. A 120 systolic might be perfect for a 45-year-old cyclist, but dangerous for an 82-year-old with weak arteries. In the U.S., the AHA/ACC still pushes for 130/80 - and even 120 if you can handle it. But they’ve added new rules: if you’re over 65, have kidney disease, or have a high risk of heart problems, start medication at 130/80. If you’re young and healthy with just stage 1 hypertension? Try lifestyle changes first - weight loss, walking 30 minutes a day, cutting salt, reducing alcohol. No pills needed yet.What Does This Mean for You?
If you’re reading this because your doctor just changed your target, here’s what to ask:- What’s my 10-year risk of heart disease or stroke? (Ask for the PREVENT calculator result.)
- Am I on more than two blood pressure meds already? If so, how much harder will it be to go lower?
- Have I had dizziness, falls, or kidney issues since starting or changing meds?
- Is my blood pressure consistently high at the clinic but normal at home? (That’s white coat hypertension - no need to over-treat.)
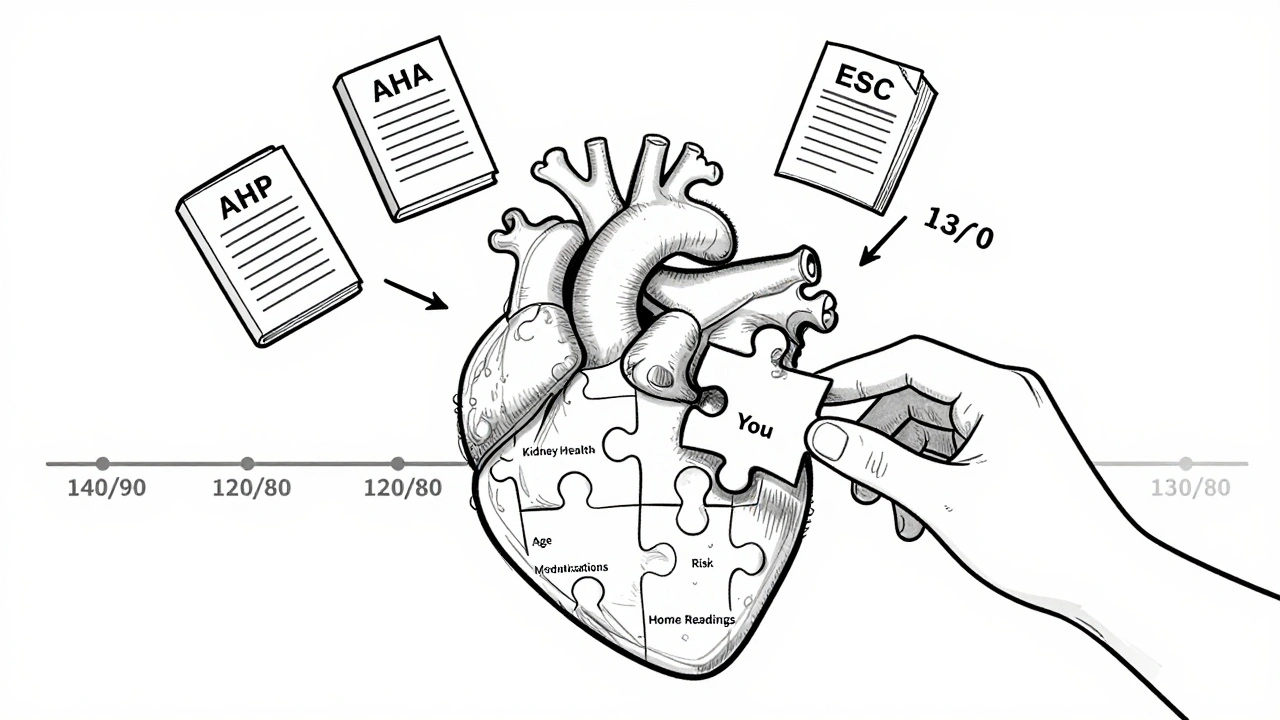
The Real Goal Isn’t a Number - It’s a Life
High blood pressure isn’t just a number on a screen. It’s a sign that your heart is working too hard, your arteries are under stress, and your risk of stroke or kidney failure is climbing. But the goal of treatment isn’t to hit 120/80 at all costs. It’s to live longer, feel better, and avoid hospitalization. Some people do great on a single pill and hit 118/76. Others need three meds, still sit at 138/85, and feel perfectly fine - with no signs of heart damage. That’s not failure. That’s individualized care. The future of blood pressure management isn’t about rigid targets. It’s about smart monitoring, personal risk profiles, and listening to the patient. New tools are emerging - apps that track home readings, AI models that predict how you’ll respond to different drugs, even genetic tests that show who’s more likely to have side effects. But none of that matters if you’re too dizzy to get out of bed.What to Do Next
If you’re managing high blood pressure:- Get your home blood pressure monitor and check it twice a week. Write down the numbers.
- Ask your doctor: “Based on my age, health, and risk score, what’s the right target for me?”
- If you’re on meds and feel lightheaded, especially when standing - tell your doctor. That’s not normal.
- Don’t rush to add another pill. Lifestyle changes - walking, sleep, reducing processed food - still work better than most people think.
- If your doctor pushes for 120/80 and you’re over 70, ask: “What’s the risk of fainting or kidney injury if I go lower?”
Is 120/80 still the best blood pressure target for everyone?
No. While 120/80 is considered ideal for healthy adults under 65, it’s not always the right goal for older adults, those with multiple health conditions, or people who experience side effects from medication. Guidelines now recommend individualized targets based on age, risk factors, and tolerance. For many, 130/80 or even 140/90 may be safer and just as effective.
What if my blood pressure is 135/85 but I feel fine?
If you’re under 65 and have no diabetes, kidney disease, or heart problems, your doctor may recommend lifestyle changes first - like reducing salt, walking daily, or losing weight - before adding medication. If you’re over 65 or have other health issues, your target may be higher. Feeling fine doesn’t mean your risk is low, but it also doesn’t mean you need more pills. Ask for your 10-year cardiovascular risk score to make a better decision.
Why do some doctors say 140/90 is fine while others push for 120/80?
It’s a clash of evidence and patient populations. The AHA/ACC guidelines are based on trials like SPRINT, which showed big benefits in a selected group of healthier people. The AAFP looks at real-world primary care, where patients are older, sicker, and on more meds. They found that pushing lower often causes more harm than good in these groups. Both sides agree on the goal - reducing heart disease - but disagree on the safest path to get there.
Can I lower my blood pressure without medication?
Yes - and it’s often the first step. Losing just 5-10 pounds can drop systolic pressure by 5-20 mm Hg. Walking 30 minutes a day lowers it by 4-9 mm Hg. Cutting salt, limiting alcohol, and eating more potassium-rich foods (like bananas, spinach, and potatoes) also help. For many people with stage 1 hypertension (130-139/80-89), lifestyle changes alone bring numbers into a healthy range without drugs.
What are the signs my blood pressure treatment is causing harm?
Watch for dizziness, especially when standing up; feeling faint or lightheaded; unusual fatigue; confusion; or reduced urine output. These can signal low blood pressure, kidney strain, or electrolyte imbalances. If you notice these after starting or increasing a blood pressure medication, contact your doctor. You may need a dose adjustment or different drug - not necessarily a higher target.
There’s no universal number that fits every heart. The best target is the one that protects your health without stealing your quality of life. Ask questions. Track your numbers. And remember - your body’s response matters more than any guideline.


Comments
olive ashley
Okay but have you seen the pharmaceutical ads? They’re pushing 120/80 like it’s a miracle cure while hiding that half the people who hit it end up falling in the shower. I’m not saying the science is fake-I’m saying the profit motive is. They don’t care if you’re dizzy, as long as you refill that script.
Brooke Evers
I’ve been managing my BP for 12 years now and honestly, the number that matters most is the one where I don’t feel like I’m going to pass out when I stand up. My doc tried to push me to 120/80 after SPRINT came out, but I kept getting lightheaded, my kidneys flagged, and I was exhausted all the time. We backed off to 138/84 and now I’m hiking, sleeping through the night, and actually enjoying life. The guidelines are great for population studies, but your body? It’s not a statistic. It’s yours. Listen to it. And if your doctor won’t, find one who will.
Ibrahim Yakubu
Let me tell you something about American medicine-they treat numbers like gods. In Nigeria, we don’t have the luxury of chasing 120/80. We have people who can’t afford to eat three meals a day, let alone buy five different pills. And yet here in the U.S., doctors are scolding patients for being at 135/85 like it’s a moral failure. This isn’t healthcare-it’s performance art. You want to lower BP? Fix the food deserts. Fix the stress. Fix the sleep. Not just slap on another beta-blocker and call it progress.
Nava Jothy
OMG I can’t believe people are still arguing about this 😭 Like, the science is CLEAR. SPRINT was a landmark study. If you’re not aiming for 120/80, you’re basically letting your arteries rot. And don’t even get me started on the AAFP-they’re just lazy and don’t want to do the work. You want to live to 90? Then BEHAVE like it. Stop making excuses. I’ve been at 118/76 for 3 years on one pill. It’s not hard. You’re just choosing comfort over longevity. 🙄
Kenny Pakade
120/80? That’s a globalist, elitist, CDC lie. The real reason they lowered the target is so they could drug more people and make more money. I’ve got a cousin in Ohio-he was healthy, got his BP checked, got labeled ‘hypertensive’ overnight, and now he’s on three pills and can’t climb stairs. That’s not medicine. That’s control. Wake up. The system is rigged.
brenda olvera
Just wanted to say thank you for this post I’ve been so confused by all the conflicting info but this made it click for me 🙌 I started checking my BP at home and turns out I only spike at the clinic so my doc said we’re good at 136/86 and honestly I feel better than ever no meds no stress just walking and eating more veggies life is good 💛
Myles White
I work in a primary care clinic and I see this every single day. The people who do best aren’t the ones who hit 120/80-they’re the ones who have a conversation with their doctor, track their numbers consistently, and make small sustainable changes. One patient, 72, diabetic, on two meds, BP at 134/82, walks his dog every morning, eats home-cooked meals, and sleeps 7 hours. He’s happier than any of my 118/76 patients who are on four meds and terrified of salt. The goal isn’t the number. It’s the life behind it. And that’s what gets lost in all the guidelines. We’re treating a number, not a person.
Jackie Petersen
They’re lying. 120/80 is a scam. The SPRINT trial was funded by Big Pharma. The people who benefited? All young, healthy, white, insured men. No one over 70, no one on dialysis, no one on Medicaid. That’s not science. That’s propaganda. And now they want to make you take more pills just so insurance can charge you more. Wake up. This isn’t about your health. It’s about profit.