
Bowel Function Index Calculator
The Bowel Function Index (BFI) is a simple 3-question survey used by healthcare providers to measure the severity of opioid-induced constipation. Answer the questions honestly to understand how much your symptoms need medical attention.
Your Bowel Function Index Score
Your score will appear here
When you start taking opioids for chronic pain, you’re often warned about drowsiness, nausea, or the risk of dependence. But one of the most common and persistent side effects rarely gets talked about until it’s already ruining your life: opioid-induced constipation. Up to 60% of people on long-term opioids develop it - and it doesn’t go away with time like other side effects. It gets worse. And if you’re not prepared, you’ll spend months struggling with bloating, straining, and the feeling that your bowels just won’t cooperate - even when you’re doing everything "right."
Why Opioids Cause Constipation (And Why Laxatives Often Fail)
Opioids don’t just block pain signals in your brain. They also latch onto receptors in your gut, slowing down everything from stomach emptying to bowel movements. This isn’t just "slow digestion." It’s a full shutdown of normal gut rhythm. Muscles in your intestines relax. Water gets sucked out of stool. Your anal sphincter tightens. Even when you feel the urge to go, your body can’t push effectively.
That’s why regular laxatives often don’t work. Most over-the-counter options - like senna or stool softeners - are designed for occasional constipation caused by diet or inactivity. Opioid-induced constipation (OIC) is a biological blockade. A 2023 study found that 68% of patients on chronic opioids reported little to no relief from standard laxatives alone. You can take fiber, drink water, and walk every day - and still be stuck.
Prevention: Start Laxatives on Day One
The biggest mistake? Waiting for constipation to happen before acting. Experts agree: if you’re starting opioids, you should start a laxative the same day. It’s not about being overly cautious - it’s about stopping the problem before it takes root.
Two types of laxatives work best for prevention:
- Osmotic laxatives - especially polyethylene glycol (PEG). These pull water into the colon to soften stool without irritating the gut. Take one dose daily, even if you’re not feeling constipated.
- Stimulant laxatives - like bisacodyl or senna. These trigger muscle contractions in the bowel. Use them every other day to avoid dependency, but keep them on hand for when PEG isn’t enough.
Pharmacists who work with chronic pain patients report a 43% increase in proper laxative use when they proactively hand out prescriptions at the same time as opioids. Don’t wait for your doctor to bring it up. Ask for a prescription for PEG 17g daily and bisacodyl 5mg every other day. That’s the baseline for most adults.
When Laxatives Aren’t Enough: Enter PAMORAs
If you’ve been on laxatives for more than 2-4 weeks and still feel blocked, it’s time to consider a different class of drugs: peripherally acting μ-opioid receptor antagonists, or PAMORAs. These are the only medications that directly reverse the gut-slowing effect of opioids - without touching your pain relief.
Here are the three main PAMORAs approved for OIC:
| Medication | Form | How Often | Onset | Key Benefit | Major Risk |
|---|---|---|---|---|---|
| Methylnaltrexone (Relistor®) | Injection | Every other day | 30 minutes | Fastest relief; used in palliative care | Abdominal pain, risk of perforation |
| Naldemedine (Symproic®) | Oral tablet | Daily | 24-48 hours | Reduces nausea too; approved for cancer patients | Diarrhea, abdominal pain |
| Naloxegol (Movantik®) | Oral tablet | Daily | 24-48 hours | Once-daily convenience | Headache, diarrhea, abdominal cramps |
Naldemedine is now the top choice for cancer patients starting opioids, thanks to 2024 ASCO guidelines that highlight its ability to improve quality of life - not just bowel function. For others, oral options like naldemedine or naloxegol are preferred because they’re easier to take than daily injections.
But here’s the catch: PAMORAs aren’t magic. They can cause diarrhea, cramps, or even - rarely - a tear in the bowel wall. That’s why they’re only recommended after laxatives fail. And they’re absolutely not safe if you have a history of bowel obstruction, Crohn’s disease, or recent abdominal surgery.
Real Patient Experiences: What Works and What Doesn’t
Online forums are full of stories from people who’ve been through this. One Reddit user wrote: "Relistor injection worked within 30 minutes when nothing else did - even after 3 weeks of constipation." Another said: "Naldemedine let me stay on my pain meds without constant bathroom struggles. I didn’t think that was possible."
But cost is a huge barrier. Without insurance, these drugs cost $500-$900 a month. In Australia, Medicare doesn’t cover them for non-cancer pain, and private insurers often require prior authorization or step therapy - meaning you have to try and fail with laxatives first, even if you know they won’t work.
A 2023 survey of 1,500 patients found that 57% stopped PAMORAs within six months - not because they didn’t work, but because they couldn’t afford them. Some patients switch back to laxatives and live with daily discomfort. Others give up on opioids entirely, even if it means more pain.
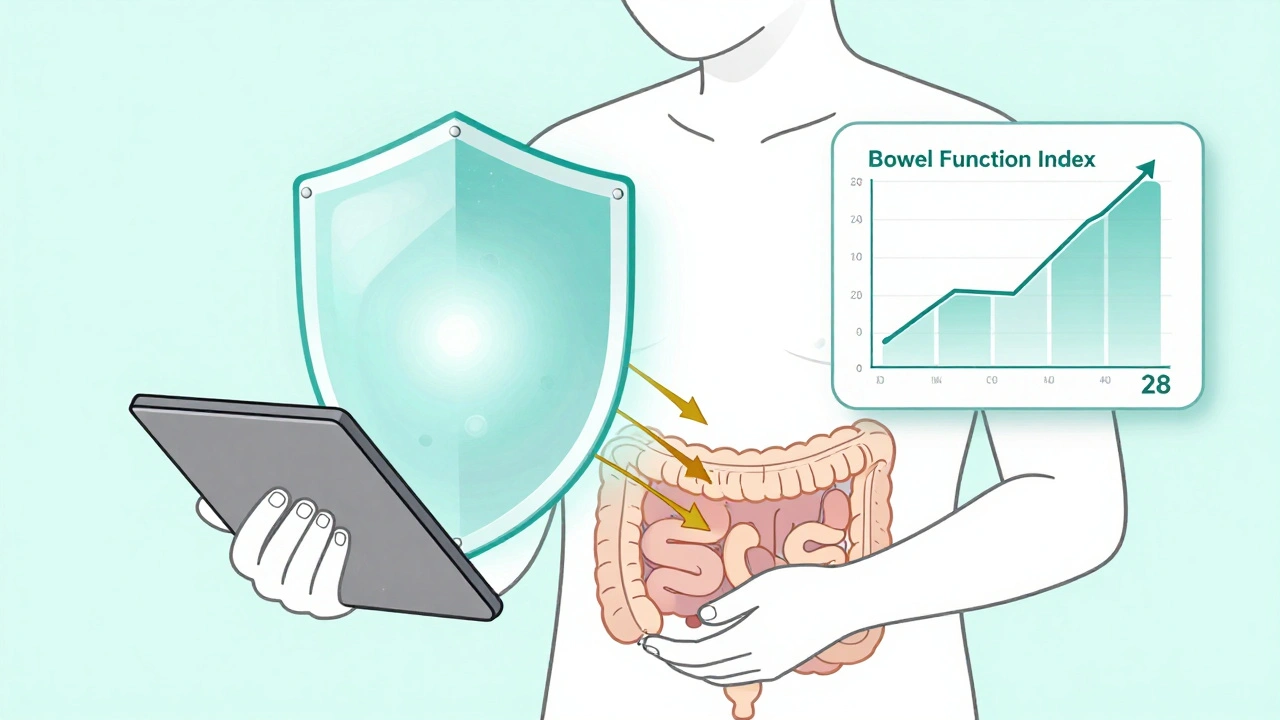
Monitoring Progress: The Bowel Function Index
How do you know if your treatment is working? Don’t just guess. Use a simple tool called the Bowel Function Index (BFI). It’s a three-question survey doctors use to measure constipation severity.
Rate yourself on:
- How difficult is it to pass stool? (1 = easy, 10 = impossible)
- How often do you feel incomplete emptying? (1 = never, 10 = always)
- How much effort do you need to have a bowel movement? (1 = none, 10 = extreme)
Add the scores. If your total is above 30, your constipation is significant and needs stronger treatment. Many patients don’t realize they’re in this range - they think "it’s just part of being on pain meds." But 30+ means you’re at risk for fecal impaction, nausea, vomiting, or even hospitalization.
What’s Next: The Future of OIC Treatment
There’s good news on the horizon. In 2023, a once-weekly injection of methylnaltrexone was approved - cutting down from daily shots to one per week. That’s a game-changer for people who struggle with injections.
Researchers are also testing combination pills that mix low-dose PAMORAs with gentle laxatives. And by 2026, genetic testing may help predict who responds best to which drug - meaning you won’t have to trial-and-error your way through months of discomfort.
But until then, the key is early action. Start laxatives with your first opioid dose. Track your bowel habits. If you’re still struggling after 2-4 weeks, talk to your doctor about PAMORAs. Don’t accept constipation as inevitable. It’s a treatable side effect - not a punishment for needing pain relief.
When to Call Your Doctor
Seek immediate help if you experience:
- No bowel movement for 4+ days despite treatment
- Severe abdominal pain or bloating
- Vomiting or inability to keep food down
- Blood in stool or rectal bleeding
- Signs of fever or chills with abdominal pain
These could signal a bowel obstruction or perforation - both medical emergencies.
Can I just use Miralax for opioid-induced constipation?
Miralax (polyethylene glycol) is one of the best first-line options for opioid-induced constipation. It’s safe for daily use and doesn’t cause dependency. But many people take too little - only 1-2 teaspoons. For OIC, you often need the full 17g dose (about 1 heaping tablespoon) every day. If you’re still constipated after 10 days at full dose, Miralax alone won’t be enough. You’ll need to add a stimulant laxative or consider a PAMORA.
Do PAMORAs reduce pain relief?
No. That’s the whole point. PAMORAs are designed to block opioid receptors only in the gut - not in the brain. Studies show they restore normal bowel function without affecting pain control. In fact, patients often report better pain tolerance because they’re not distracted by constipation or nausea. If your pain gets worse after starting a PAMORA, it’s likely due to another cause - talk to your doctor.
Is OIC more common in older adults?
Yes. Older adults are at higher risk because their digestive systems naturally slow down with age. They also tend to take more medications that worsen constipation, like anticholinergics or calcium channel blockers. Plus, they’re less likely to drink enough water or move around. If you’re over 65 and on opioids, proactive laxative use is even more critical. Start with PEG daily and monitor closely.
Can diet and exercise fix opioid-induced constipation?
Diet and exercise help - but not enough. Eating fiber, drinking water, and walking are essential for overall gut health. But opioids override these benefits by directly shutting down gut motility. You can eat all the prunes and do yoga every day - and still be blocked. Think of diet and movement as support, not the main treatment. They should be paired with medication, not used instead of it.
Why don’t doctors talk about OIC more?
Many doctors focus on pain control and assume constipation is "just a side effect" patients should handle on their own. Others don’t know the latest guidelines. A 2015 study showed only 32% of primary care providers proactively prescribe laxatives with opioids - compared to 85% in palliative care. It’s not that they’re ignoring you. It’s that they’re not trained to see OIC as a medical issue that needs a plan. Bring the info to them. Ask for PEG and bisacodyl on day one.
Final Takeaway
Opioid-induced constipation isn’t something you just have to live with. It’s a predictable, preventable, and treatable condition - but only if you act early. Start with osmotic laxatives on day one. Track your bowel habits. If you’re still struggling after a few weeks, ask about PAMORAs. Don’t wait until you’re in pain, bloated, and desperate. The tools exist. The science is clear. You deserve to manage your pain without losing your quality of life to constipation.


Comments
Heidi Thomas
Stop wasting time with laxatives. If you're on opioids long-term and still constipated, you're doing it wrong. PAMORAs aren't optional - they're the only thing that actually works. Stop letting doctors gaslight you into thinking it's just "part of the deal."
Alex Piddington
Thank you for this comprehensive overview. It's vital that patients understand this is not a lifestyle issue but a pharmacological one. Proactive management with PEG and bisacodyl from day one is evidence-based and should be standard practice. Let's advocate for better protocols in primary care.
With respect, Alex
Libby Rees
I've been on oxycodone for five years. Started PEG on day one. Never had a problem. My doctor didn't mention it. I read it online. I wish more people knew this wasn't normal suffering. It's preventable. Don't wait until you're in agony.
Dematteo Lasonya
This post saved me. I was ready to quit my pain meds because I couldn't go to the bathroom without crying. Started PEG and bisacodyl like you said. Two days later I felt human again. Thank you for not making me feel broken for needing help.
Rudy Van den Boogaert
I'm curious if anyone's tried combining naldemedine with magnesium citrate? My GI doc said it's not contraindicated, but I haven't seen anyone mention it here. I'm on day 12 and still struggling even with the full PEG dose.
Gillian Watson
In the UK we're lucky if our GP even knows what a PAMORA is. My mum's on opioids for arthritis and they gave her senna and told her to drink more water. She's been stuck for months. It's a scandal.
Jordan Wall
Honestly? This is just Big Pharma’s latest cash grab. PAMORAs cost $900/month? LOL. They’re just repackaging naloxone and calling it a breakthrough. Meanwhile, your average patient is stuck choosing between pain and poop. Capitalism at its finest 🤡💸
Gareth Storer
So let me get this straight. You’re telling me the solution to a side effect caused by a drug designed to shut down pain is... another drug that shuts down the drug’s side effect? Brilliant. We’re just playing whack-a-mole with biology now. Next up: opioid-induced opioid-induced constipation.
Pavan Kankala
They don't want you to know this because if people realized constipation was fixable, they'd stop blaming the opioid crisis on addicts. It's not addiction - it's corporate negligence. The real crisis is that pharma knew this would happen and buried the research. You're being used.