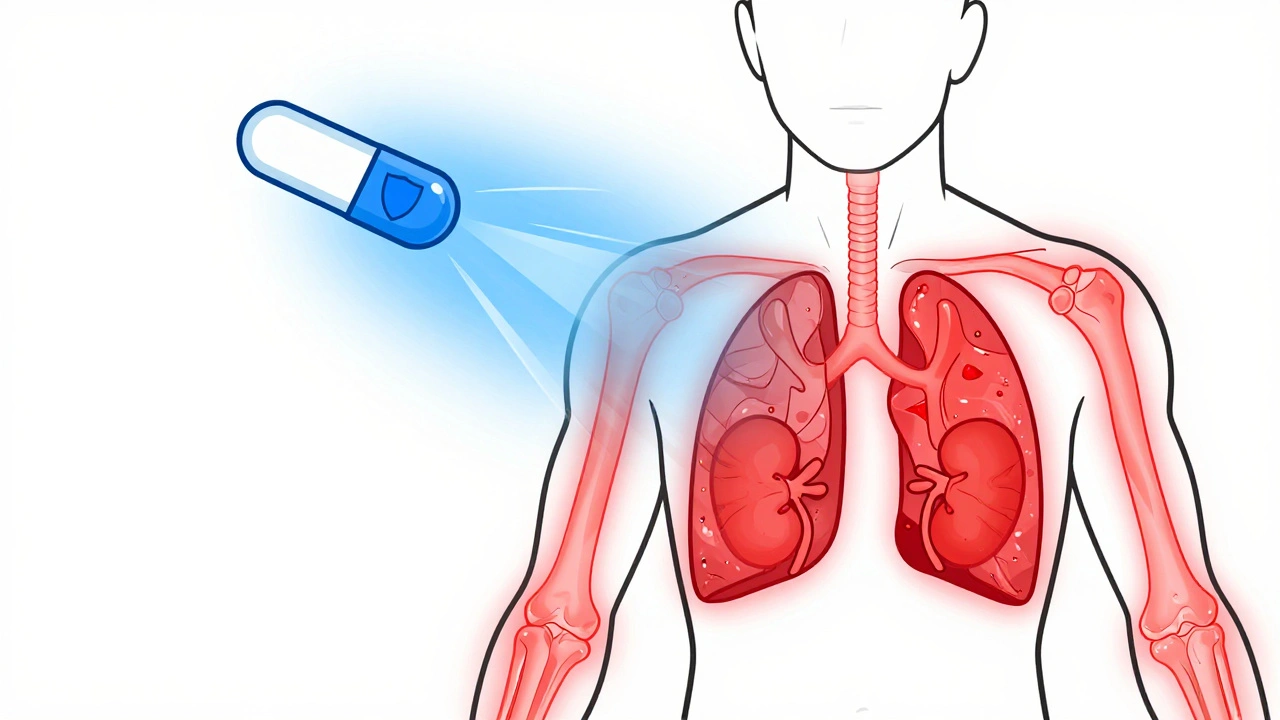
When your immune system turns on your own body, things get messy fast. Autoimmune diseases like lupus, rheumatoid arthritis, and vasculitis don’t just cause pain-they can wreck organs, damage nerves, and shut down systems. That’s where corticosteroids come in. These aren’t the bodybuilding steroids you hear about in sports. They’re synthetic versions of cortisol, your body’s natural stress hormone, and they’re one of the fastest, most powerful tools doctors have to calm down an out-of-control immune response.
How Corticosteroids Stop Inflammation in Its Tracks
Corticosteroids like prednisone and methylprednisolone don’t just mask symptoms-they rewire the inflammation process at a cellular level. Within hours of taking a dose, they bind to receptors inside nearly every cell in your body. That triggers a chain reaction: genes that produce inflammatory proteins like TNF-alpha and interleukins get switched off. Enzymes like phospholipase A2, which fuel the fire of swelling and pain, get blocked. The result? Swelling drops, joints stop screaming, and breathing gets easier-sometimes within a day.
That speed is why they’re still first-line treatment for aggressive autoimmune flare-ups. In conditions like Goodpasture’s syndrome or rapidly progressive glomerulonephritis, doctors don’t wait. They hit hard with high-dose IV methylprednisolone pulses, often paired with cyclophosphamide, to stop kidney failure before it starts. For someone with severe lupus nephritis or active vasculitis, this isn’t just treatment-it’s life-saving.
When Corticosteroids Work-and When They Don’t
They’re not magic bullets. Corticosteroids work brilliantly for diseases driven by acute inflammation: rheumatoid arthritis, inflammatory bowel disease, severe asthma, psoriasis, and autoimmune hemolytic anemia. In fact, combining them with drugs like rituximab has pushed relapse-free survival rates higher than prednisone alone in some cases.
But they don’t fix everything. For advanced type 1 diabetes, Hashimoto’s thyroiditis, Graves’ disease, or late-stage primary biliary cholangitis, corticosteroids offer little to no benefit. Why? Because the damage is already done. If the pancreas cells are gone, or the thyroid is a scarred shell, turning off inflammation won’t bring them back. The same goes for advanced multiple sclerosis-steroids can reduce a flare, but they won’t repair damaged nerve pathways.
Here’s the catch: early-stage type 1 diabetes and early primary biliary cholangitis might still respond. That’s because some cells are still alive and just under attack. In those cases, steroids can buy time-slowing destruction until other therapies kick in.

The Hidden Cost: Long-Term Side Effects
Every benefit comes with a price. The longer you take corticosteroids-especially at doses over 7.5 mg of prednisone daily-the more your body pays. Bone density starts dropping within months. Up to 30% of long-term users develop osteoporosis, and fractures become common. That’s why doctors now routinely prescribe calcium, vitamin D, and bisphosphonates alongside steroids.
Cataracts? Common. After two years of daily use, nearly 1 in 5 people develop clouded lenses. Glaucoma risk rises too. Your skin thins, bruises easily, and may darken or develop stretch marks. Blood sugar spikes-steroids can trigger or worsen diabetes. Fluid retention leads to puffy cheeks, a moon face, and weight gain around the midsection. Mood swings, insomnia, and even depression aren’t rare.
And then there’s adrenal insufficiency. Your body gets lazy. If you’ve been on steroids for more than three weeks, your adrenal glands stop making cortisol on their own. Stop suddenly? You could crash-low blood pressure, vomiting, confusion, even death. That’s why tapering isn’t optional. It’s mandatory. Doctors slowly reduce the dose over weeks or months, letting your body relearn how to produce its own hormone.
How to Use Them Safely
The goal isn’t to avoid steroids-it’s to use them smart. Modern guidelines focus on the lowest effective dose for the shortest possible time. For someone with mild rheumatoid arthritis, that might mean 5 mg of prednisone daily for three months, then off. For severe lupus, it could be 30 mg daily for six weeks, then a slow taper.
Dosing matters. Taking steroids in the morning mimics your body’s natural cortisol rhythm. Evening doses? They’re more likely to mess with sleep and suppress your adrenal glands. If you’re on long-term therapy, your doctor should check your morning cortisol levels and bone density yearly.
Topical versions help avoid systemic side effects. Inhaled steroids for asthma, creams for eczema, and nasal sprays for allergies deliver the drug right where it’s needed-minimal absorption, minimal risk. That’s why asthma patients now use inhalers instead of pills whenever possible.
The Future: Less Steroids, More Precision
Doctors aren’t happy relying on steroids long-term. That’s why the field is shifting hard toward combination therapy. Rituximab, methotrexate, azathioprine, and newer biologics like belimumab are now used upfront to reduce steroid doses. In some cases, patients get off steroids entirely within a year.
Research is also exploring drugs that mimic the anti-inflammatory effects of steroids without the side effects. One promising target is GILZ, a protein that mediates how steroids suppress inflammation. If scientists can develop a GILZ-based drug, it could offer the benefits of steroids without the bone loss or cataracts.
For now, the best strategy is this: use steroids to get control fast, then layer in other drugs to hold the line. Think of them as a fire extinguisher-not the HVAC system.
What Patients Need to Know
If you’re on corticosteroids:
- Never stop cold turkey. Always taper with your doctor’s plan.
- Take them in the morning unless told otherwise.
- Get bone scans, eye exams, and blood sugar checks yearly.
- Use sunscreen-your skin is more sensitive to UV damage.
- Carry a medical alert card if you’ve been on them longer than three weeks. Emergency rooms need to know.
- Report mood changes, vision problems, or unexplained bruising right away.
It’s not about fear. It’s about awareness. Steroids saved millions of lives since the 1940s. But they’re a double-edged sword. The smarter you are about how you use them, the less they’ll hurt you in the long run.
Can corticosteroids cure autoimmune diseases?
No. Corticosteroids don’t cure autoimmune diseases. They suppress the immune system’s attack on the body, which reduces inflammation and eases symptoms. Once you stop taking them, the immune system often resumes its attack. That’s why they’re used to control flares, not to eliminate the disease. Long-term control requires other medications like methotrexate or biologics.
How long can you safely take prednisone?
There’s no fixed safe time, but the risk of serious side effects rises sharply after three months. For short-term flares (under two weeks), side effects are usually mild. For treatment lasting longer than three months, doctors aim to taper down to the lowest possible dose or switch to other drugs. Some patients stay on low doses (5 mg or less) for years, but only with close monitoring for bone loss, eye issues, and blood sugar.
Do corticosteroids make you gain weight?
Yes, and it’s not just water weight. Corticosteroids increase appetite and change how your body stores fat, especially around the abdomen, face, and back. They also cause fluid retention. This weight gain is common, even at low doses, and can be hard to reverse. Diet and exercise help, but the main fix is reducing the steroid dose under medical supervision.
Are there natural alternatives to corticosteroids?
No natural remedy can match the power of corticosteroids to stop severe autoimmune inflammation. Supplements like turmeric or fish oil have mild anti-inflammatory effects, but they won’t control a lupus flare or prevent kidney damage in vasculitis. Relying on them instead of prescribed steroids can lead to irreversible organ damage. They may help as complementary support, but never as replacements.
Why do doctors prescribe steroids for asthma if they have so many side effects?
Because inhaled steroids deliver the drug directly to the lungs, with very little entering the bloodstream. This means they control airway inflammation with minimal side effects. Oral steroids are only used for severe flare-ups, and even then, for just a few days. The benefit-preventing hospitalization and breathing failure-far outweighs the risk when used correctly.
Can corticosteroids cause mental health issues?
Yes. Steroids can cause mood swings, anxiety, irritability, insomnia, and even psychosis at high doses. These effects are more common in people with a history of mental health conditions. If you notice sudden changes in mood or sleep, tell your doctor. Lowering the dose or switching medications often helps. Never ignore these symptoms-they’re treatable.
Is it safe to get vaccines while on corticosteroids?
Inactivated vaccines (like flu, pneumonia, or COVID-19 shots) are generally safe. Live vaccines (like MMR or shingles) are not recommended if you’re on high-dose or long-term steroids because your immune system is suppressed. Always check with your doctor before any vaccination. Timing matters-some doctors pause steroids briefly around vaccine dates to improve response.
What happens if I miss a dose of my steroid?
If you miss one dose, take it as soon as you remember-unless it’s close to your next scheduled dose. Don’t double up. If you’ve been on steroids for more than three weeks, missing doses can trigger adrenal insufficiency symptoms like dizziness, nausea, or fatigue. Call your doctor if you miss more than one dose or if you’re sick and can’t take them. You may need a temporary boost.


Comments
Yasmine Hajar
Corticosteroids saved my life when I had a lupus flare that was eating my kidneys-no joke. I was on IV methylprednisolone for five days, and within 48 hours, my creatinine dropped like a rock. But then came the moon face, the insomnia, the crying at commercials. Worth it? Yeah. Would I do it again? Only if I had to.
Martyn Stuart
Just a quick note: never, ever stop steroids cold turkey-especially after three weeks. I did it once, thought I was ‘fine,’ and ended up in the ER with hypotension and vomiting. Adrenal insufficiency isn’t a myth-it’s a silent killer. Always taper. Always. Your doctor isn’t being paranoid; they’re saving your life.
zac grant
Let’s be real-steroids are the fire extinguisher of autoimmune care. You don’t live in the house after you put out the fire. You fix the wiring. That’s why biologics and DMARDs are the future. Steroids buy you time; they don’t give you a cure. Smart docs know this. Dumb docs keep you on 10mg for five years. Don’t be that patient.
Jake Deeds
Some people treat steroids like candy. ‘Oh, I’ll just take a pill when I feel tired.’ No. No, no, no. You’re not ‘just’ a patient-you’re a biological system under siege. And if you’re cavalier about this, you’re not just risking osteoporosis-you’re risking your dignity. Your skin, your bones, your mind-they all remember.
Heidi Thomas
‘Natural alternatives’? Please. Turmeric won’t stop vasculitis. Fish oil won’t save your lungs from a severe asthma attack. If you’re looking for magic herbs instead of science, you’re not healing-you’re gambling with your organs. Stop romanticizing ‘natural’ and start respecting pharmacology.
Libby Rees
Topical and inhaled steroids are the unsung heroes. My son has asthma. He’s been on fluticasone for three years. Zero weight gain. Zero mood swings. Just clean airways. Systemic steroids are blunt instruments. Local delivery is precision engineering. Why we don’t push this harder is beyond me.
Alex Piddington
For anyone on long-term steroids: get a medical alert bracelet. Seriously. I was in a car crash last year. Paramedics didn’t know I was on prednisone. I went into adrenal crisis. They gave me IV fluids. Didn’t give me hydrocortisone. I nearly died. Don’t make my mistake.
Karl Barrett
The GILZ protein pathway is the holy grail. Steroids bind to glucocorticoid receptors, which then activate GILZ, which then suppresses NF-kB and AP-1-key transcription factors in inflammation. If we can pharmacologically mimic GILZ without the genomic side effects, we’ve cracked the code. The real breakthrough won’t be a new steroid-it’ll be a steroid without the baggage.
Rudy Van den Boogaert
My rheumatoid arthritis flares up every winter. I’ve been on 5mg prednisone for two years now. I take it in the morning, I do weight-bearing exercise, I get bone scans yearly. It’s not perfect, but it’s manageable. The key? Consistency. Not fear. Not guilt. Just routine. And a good doctor who doesn’t treat you like a statistic.
Dematteo Lasonya
It’s weird how people think steroids are ‘bad’ but don’t blink at chemo. Both are toxic. Both are necessary. The difference? Chemo gets a pass because it’s for cancer. Steroids? They’re for ‘just’ autoimmune stuff. But if your kidneys fail because you refused a short course, who’s the fool then?
Carolyn Ford
Oh, so now we’re blaming patients for not knowing enough? I’ve been on steroids for 12 years. I know the side effects. I know the risks. But I’m still here. My joints still move. My lungs still work. You don’t get to judge me because you haven’t lived in my skin. I’m not lazy-I’m surviving.
Gillian Watson
My mom had Graves’ and was on steroids for six months. She lost 15 pounds of muscle, got cataracts, and couldn’t sleep. But she didn’t die. And she still walks her dog every morning. Steroids aren’t the enemy. Giving up on treatment is.
John Filby
Just took my morning dose. ☕️ Also just ate a whole pizza. 😅 My body’s like ‘you’re literally asking for trouble’ and I’m like ‘I know, but I’m also alive.’
Benjamin Sedler
What if we just… didn’t use steroids at all? What if we just let the immune system do its thing? Maybe the body knows better than we do. Maybe inflammation isn’t the enemy-maybe it’s the body trying to heal. Maybe we’re the ones being the bullies here.
michael booth
I’ve been off prednisone for 18 months. Still get the occasional joint ache. Still check my bone density. Still take calcium. Still remember. Always remember.