When your kidneys stop working, it’s not just about feeling tired or swollen. It’s about your body losing its ability to clean your blood, balance fluids, and control blood pressure. By the time most people notice symptoms, their kidneys have already lost 85-90% of their function. This is called end-stage renal disease, or ESRD. And the three biggest reasons this happens? Diabetes, hypertension, and glomerulonephritis.
Diabetes: The Silent Kidney Killer
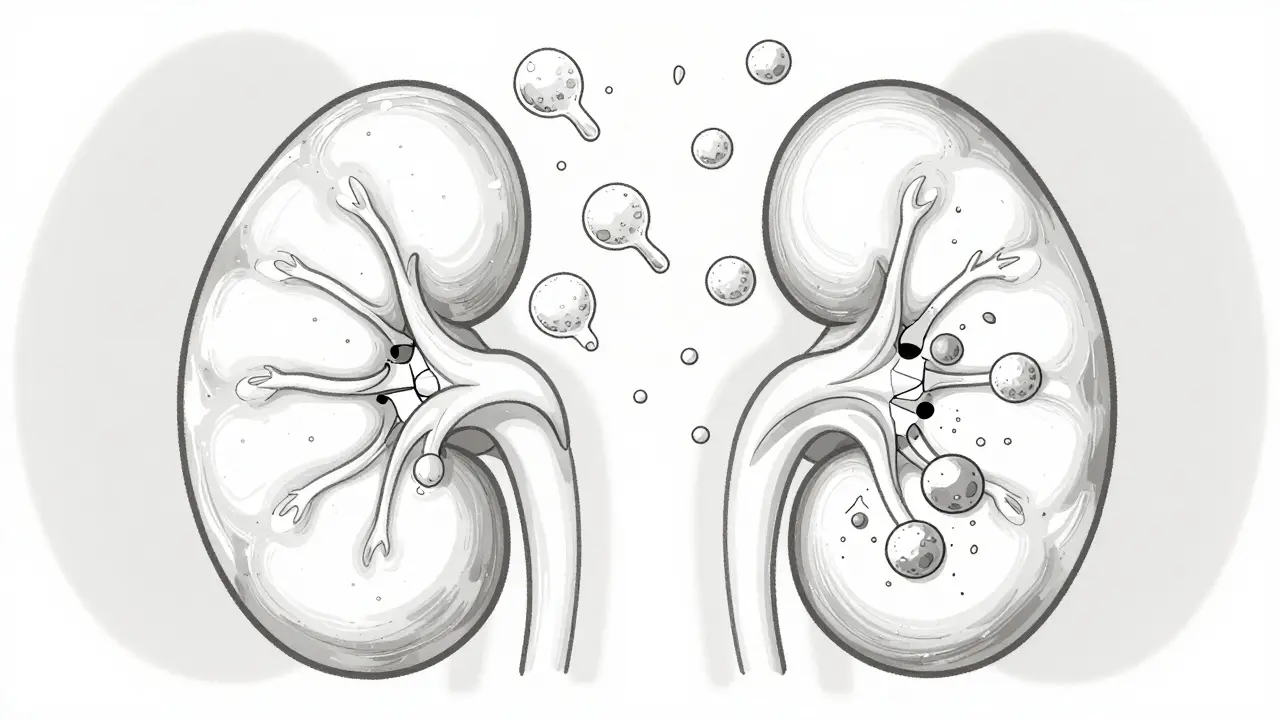
Diabetes doesn’t just affect your blood sugar-it slowly destroys your kidneys. In the U.S., nearly half of all new kidney failure cases come from diabetes. That’s not a coincidence. High blood sugar over years forces your kidneys to work too hard. At first, they compensate by filtering more blood than normal-a state called hyperfiltration. But this extra strain damages the tiny filters inside your kidneys, called glomeruli.
These filters are made of delicate cells and membranes. Over time, the basement membrane thickens from a normal 300-400 nm to 450-650 nm. The cells that hold back protein-called podocytes-start dying off. Protein leaks into your urine, the first real warning sign. That’s why doctors test for albumin in your urine every year if you have diabetes. If you’re leaking more than 30 mg/g, you’re in the early danger zone. At 300 mg/g or higher, your risk of kidney failure in five years jumps to 44%.
And here’s the scary part: many people don’t know they have diabetic kidney damage until it’s advanced. Type 2 diabetes often starts silently. By the time someone is diagnosed with diabetes, up to 40% already have signs of kidney damage. The good news? Getting your HbA1c below 7% within the first five years of diagnosis cuts your risk of kidney disease by 54%. Medications like SGLT2 inhibitors (empagliflozin, dapagliflozin) don’t just lower blood sugar-they reduce kidney failure risk by 32%. These drugs work by making your kidneys flush out extra sugar and salt, which takes pressure off the filters.
Hypertension: The Hidden Pressure Cooker
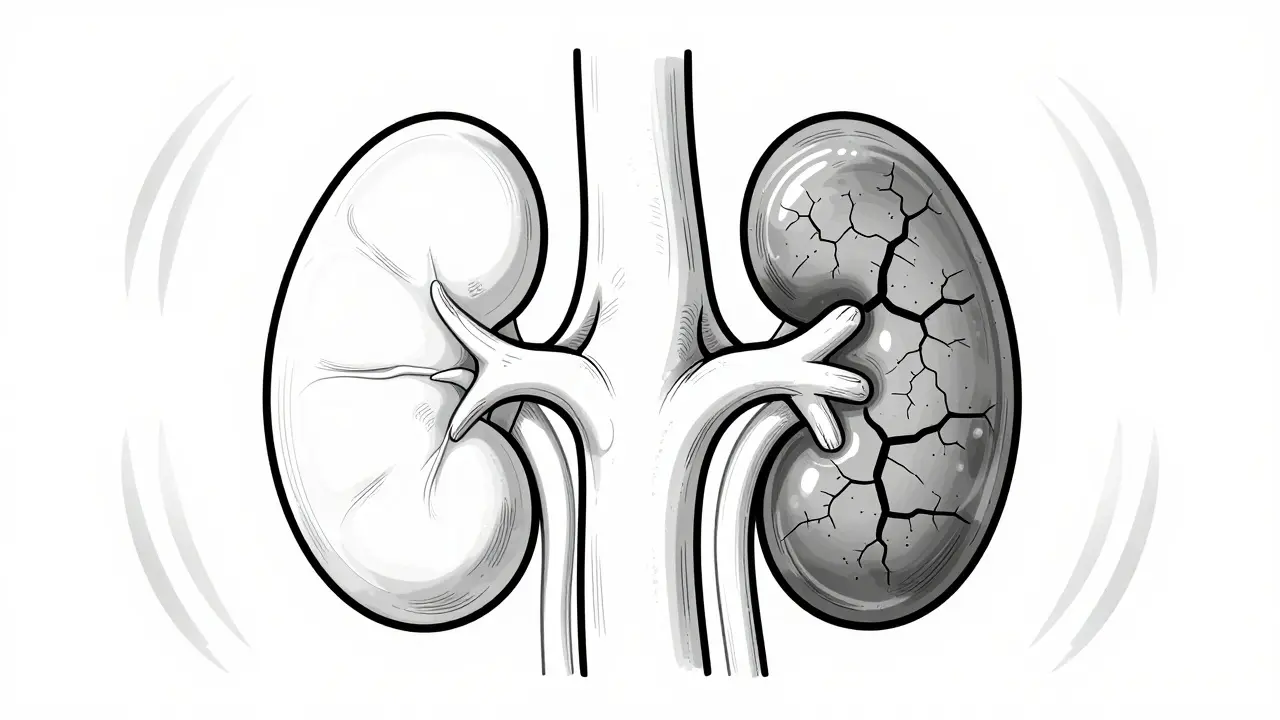
High blood pressure is the second biggest cause of kidney failure. And it’s sneaky. You might not feel it. No headaches, no dizziness-just slowly crushing your kidneys from the inside. When your blood pressure stays above 140/90 mmHg, the small arteries feeding your kidneys start to harden and narrow. This is called nephrosclerosis. Less blood reaches the glomeruli. They starve. And when they starve, they scar.
Studies show that within five years of uncontrolled hypertension, kidney blood flow drops by 15-25%. About 60-70% of people with long-term high blood pressure show signs of glomerulosclerosis-where entire filtering units turn to scar tissue. The damage is often worse when it teams up with diabetes. In fact, 75% of people with diabetes also develop high blood pressure. Together, they accelerate kidney decline by more than 75% compared to diabetes alone.
Targeting blood pressure isn’t just about preventing heart attacks. For people with kidney disease, aiming for under 120/80 mmHg slows progression by 27%. But it’s not one-size-fits-all. Older adults or those prone to dizziness need careful balancing. ACE inhibitors and ARBs are the go-to medications-not just because they lower pressure, but because they directly protect the kidney filters. They reduce protein leakage and slow scarring. Still, only 58% of patients stick with these meds after a year. Why? Side effects like cough, fatigue, or the feeling that “I feel fine, so why take pills?”
Glomerulonephritis: When Your Immune System Attacks Your Kidneys
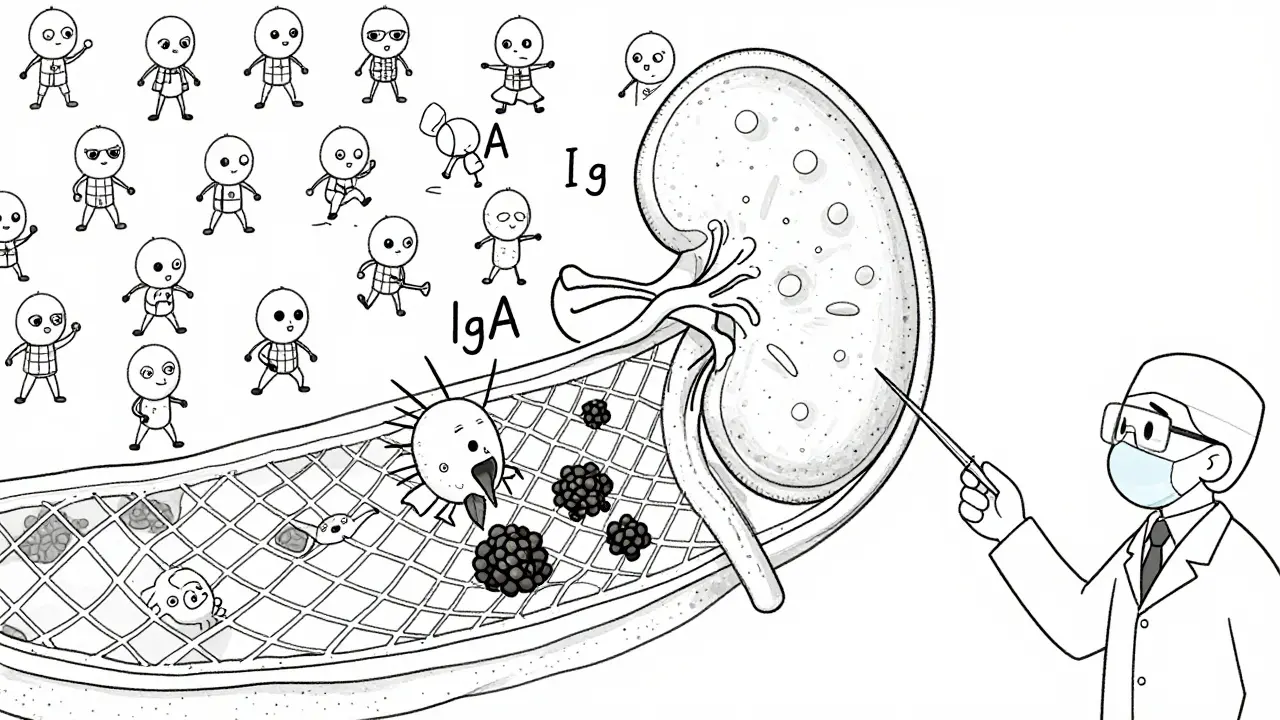
Unlike diabetes and hypertension, which creep in over decades, glomerulonephritis can strike suddenly. It’s not caused by lifestyle-it’s caused by your own immune system. Your body makes antibodies that attack the glomeruli, thinking they’re foreign invaders. The most common form is IgA nephropathy, which affects 2.5-4.5 people per 100,000 each year. It’s more common in Asia and often shows up in young adults after a cold or sore throat.
Under the microscope, you see IgA protein clumps stuck in the kidney’s filtering mesh. These trigger inflammation, swelling, and eventually scarring. Some people have mild disease and never progress. Others lose kidney function over 20 years. The risk depends on how much protein leaks into urine and how much scarring is already there. A high Oxford MEST-C score means worse odds-only 20% of those patients keep their kidneys after 20 years.
Lupus nephritis is another form, affecting up to 60% of people with systemic lupus. Class IV lupus nephritis has a 28.7% chance of leading to kidney failure within 10 years. The challenge? Diagnosis often takes over a year. Patients see seven doctors, get misdiagnosed as having a urinary infection or autoimmune flare, and lose precious time. One Reddit user shared: “I saw seven doctors over 18 months before someone finally did a biopsy and said, ‘It’s IgA nephropathy.’”
Treatment is complex. Steroids and immunosuppressants like rituximab can cut kidney failure risk by nearly half in high-risk cases. But they come with risks-especially in older patients. One expert warns aggressive treatment increases infection deaths by 18% without clear kidney benefit. Others argue that delaying treatment costs patients 3.2 years of dialysis time over a decade. There’s no easy answer, but early biopsy and personalized therapy make all the difference.
Why Early Detection Changes Everything
Here’s the truth: kidney failure doesn’t happen overnight. It’s a slow leak. And the earlier you catch it, the more you can stop it.
For diabetes: Get your urine tested for albumin every year. Start an SGLT2 inhibitor if you’re leaking protein-even if your blood sugar is under control. Don’t wait for creatinine to rise. By then, it’s too late.
For hypertension: Treat your blood pressure like your life depends on it-because it does. Use ACE inhibitors or ARBs. Check your kidney function annually. Don’t assume “no symptoms” means “no problem.”
For glomerulonephritis: If you have blood or protein in your urine after an infection, don’t brush it off. Push for a kidney biopsy. Know your MEST-C score. Ask about new drugs like sparsentan, which is expected to be approved soon and reduces protein leakage by nearly 50%.
The data is clear: early action saves kidneys. In one study, 31% of diabetic patients who started SGLT2 inhibitors within six months of spotting albuminuria stabilized their kidney function. That’s not a miracle-it’s science.
The Bigger Picture: Cost, Access, and the Global Gap
Kidney failure isn’t just a medical issue-it’s a financial and social one. In the U.S., treating a diabetic ESRD patient costs Medicare $96,000 a year. That’s nearly $20,000 more than treating someone whose kidney failure came from high blood pressure. Globally, 850 million people have some form of kidney disease. But in low-income countries, only 10% have access to dialysis or transplant. In high-income places, it’s 95%.
This isn’t just about money. It’s about justice. People with diabetes and hypertension in poor regions are dying because they can’t get the basic tests or meds that could have saved their kidneys. Meanwhile, new drugs like finerenone and sparsentan are hitting the market-expensive, effective, and out of reach for most.
But the future isn’t hopeless. The Lancet Commission predicts that if we scale up early screening, blood pressure control, and SGLT2 inhibitors globally, we could prevent 30-50% of all future kidney failures. That’s millions of lives.
What You Can Do Right Now
If you have diabetes or high blood pressure:
- Get your urine tested for albumin at least once a year.
- Ask your doctor if an SGLT2 inhibitor or ACE/ARB is right for you-even if your kidneys seem fine.
- Keep your blood pressure under 130/80 (or 120/80 if you have protein in your urine).
- Don’t ignore swelling, fatigue, or foamy urine. These aren’t normal.
If you’ve been told you have glomerulonephritis:
- Get a biopsy if you haven’t already.
- Ask about your MEST-C score and what it means for your risk.
- Find a nephrologist who specializes in immune kidney diseases.
Your kidneys don’t scream. They whisper. Listen before it’s too late.
Can you reverse kidney damage from diabetes?
Early kidney damage from diabetes can be slowed or even stabilized-but not fully reversed. If you catch it in the microalbuminuria stage (30-300 mg/g urine protein), tight blood sugar control and SGLT2 inhibitors can prevent progression. Once scarring sets in, the damage is permanent. The goal isn’t reversal-it’s stopping it from getting worse.
Does high blood pressure always cause kidney failure?
No. Many people live with high blood pressure for decades without kidney damage. But if it’s uncontrolled for more than 5-10 years, especially with other risk factors like diabetes or obesity, the risk rises sharply. The key is consistent management. Keeping pressure under 130/80, using ACE inhibitors, and monitoring kidney function yearly can prevent failure in most cases.
What are the early signs of glomerulonephritis?
Early signs are often silent. But some people notice foamy urine (from protein), blood in the urine (pink or cola-colored), swelling in the face or ankles, or high blood pressure that’s hard to control. After a throat infection or cold, if these symptoms appear, get a urine test. Many cases are found accidentally during routine checks.
Are SGLT2 inhibitors safe for people without diabetes?
Currently, SGLT2 inhibitors are approved for people with type 2 diabetes and chronic kidney disease-even if they don’t have diabetes. Studies show they protect kidneys in non-diabetic patients with proteinuria. But they’re not yet approved for general use in healthy people. Always consult a nephrologist before starting.
How often should I get my kidneys checked if I have high blood pressure?
At least once a year. Get a urine test for albumin-to-creatinine ratio (UACR) and a blood test for eGFR. If you have protein in your urine, or your blood pressure is hard to control, check every 3-6 months. Early detection is the only way to stop kidney failure before it starts.


Comments
Jason Xin
This post hit different. I’ve seen too many family members ignore the whispers until their kidneys gave out. That stat about 40% of Type 2 diabetics already having kidney damage at diagnosis? Chilling. I started getting my urine tested after my uncle ended up on dialysis. Best decision I ever made.
Also, SGLT2 inhibitors aren’t magic, but they’re the closest thing we’ve got. My doc put me on dapagliflozin last year-HbA1c dropped, albuminuria halved. No hype, just science.
Amy Insalaco
While the piece is superficially compelling, it fundamentally misrepresents the pathophysiological hierarchy of renal injury. The conflation of diabetic nephropathy with hypertensive nephrosclerosis as equivalent etiologies ignores the distinct molecular cascades-particularly the role of TGF-beta upregulation in podocyte apoptosis versus endothelin-mediated arteriolar remodeling. Moreover, the uncritical endorsement of SGLT2 inhibitors neglects the confounding influence of natriuresis-induced RAAS activation in non-proteinuric populations. The Oxford MEST-C scoring system, while statistically robust, remains a histological proxy lacking prospective validation in diverse ethnic cohorts. One must question the epistemic authority of guidelines that prioritize pharmacologic intervention over structural determinants of care access.
kate jones
Thank you for this. As someone who works with immigrant communities, I see how often kidney disease is missed because testing isn’t accessible or explained. People think if they don’t feel sick, they’re fine. But the real tragedy isn’t the disease-it’s the silence around it.
For those reading this: if you’re on Medicare or Medicaid, ask your provider about free annual UACR screening. It’s covered. No copay. You don’t need a referral. Just ask. And if you’re in a rural area, community health centers often have mobile labs. Don’t wait for symptoms. The kidneys don’t shout-they just stop working.
Kimberly Reker
Y’all need to stop waiting for the crash. I’m 34, prediabetic, BP’s been 135/88 for two years. My doc said, ‘You’re fine.’ I said, ‘Prove it.’ Got the urine test-albumin was 42 mg/g. She was shocked. Started me on an SGLT2 inhibitor. Two months later, down to 18. No side effects. No drama.
Just get tested. It takes five minutes. Your future self will hug you.
Rob Webber
This is why people die. You write a 2000-word essay on kidney damage and still don’t tell people to stop eating processed sugar and salt. You talk about meds like they’re magic pills. But no one says: ‘Cut out soda. Stop the fast food. Walk 30 minutes a day.’
Doctors are complicit. Pharma is complicit. We’re all just waiting for the next pill to fix what we refuse to change.
calanha nevin
Early detection saves kidneys. That’s not opinion. That’s data. Every year without a urine test is a gamble you can’t afford to lose. If you have diabetes or high blood pressure, you are at risk. Not maybe. Not potentially. You are at risk.
Get tested. Ask for the albumin-to-creatinine ratio. Don’t settle for ‘your kidneys look fine’ without numbers. Your life depends on the numbers.
Lisa McCluskey
I had IgA nephropathy diagnosed at 28. Took three years. Seven doctors. Two misdiagnoses. One biopsy that almost didn’t happen because my insurance said ‘no evidence of progression.’
My MEST-C score was C2, M1, E1, S1, T1. High risk. Started on steroids and ARBs. Lost 30% of kidney function in two years. Then I found a nephrologist who actually listened.
Don’t let bureaucracy steal your kidneys. Push. Keep pushing.
owori patrick
Back home in Nigeria, we don’t have SGLT2 inhibitors. We don’t even have regular urine tests. My cousin died of kidney failure at 36. No one knew he had diabetes until he was in the hospital. We use herbal tea and hope.
This article is important. But it’s written for people who have access. What about the 90% who don’t? We need cheap screening tools. Portable dipsticks. Community health workers. Not just fancy drugs.
Knowledge is power, but power means nothing if you can’t reach it.
Sheila Garfield
My mum’s on dialysis now. She’s 68. Had hypertension for 30 years. Never got tested for albumin. Thought ‘no swelling = no problem.’
She’s alive because she got lucky with a transplant. But 80% of people like her don’t. This isn’t just medical advice. It’s a lifeline. Please share this. With your parents. Your aunts. Your coworkers. Someone’s life is hanging on this.
Shawn Peck
Stop lying to people. SGLT2 inhibitors don’t fix bad habits. They just delay the inevitable. You think a pill lets you eat pizza every night? No. It just makes you feel better while your kidneys rot. The real solution? Stop being lazy. Stop eating junk. Move your ass. That’s it. No magic drugs. Just discipline.
Donna Fleetwood
Hey, if you’re reading this and you’re scared-good. That means you care. I was terrified when I got my first albumin result. But I didn’t panic. I asked questions. I changed my diet. I started walking. I took my meds.
My kidneys are stable now. Not perfect. But stable. You can do this. One step. One test. One conversation with your doctor. You’ve got this.
Blair Kelly
Glomerulonephritis isn’t ‘rare.’ It’s ignored. And the system is designed to ignore it. Biopsies are expensive. Nephrologists are overworked. Patients are told to ‘wait and see.’
That’s not medicine. That’s negligence. I’ve seen three patients die because their biopsy was delayed for 14 months. One was 22. One was 19. One was 31.
Stop waiting. Demand the biopsy. Now.
Lily Steele
My dad’s on SGLT2 inhibitors. He’s 72. Has diabetes and BP. Said he’d never take pills. Then he saw his urine test results. Now he takes them like clockwork. No drama. Just life.
Don’t wait for the crash. Just get tested. It’s one appointment. One cup of urine. One chance to keep your kidneys.