Mood Stabilizer Interaction Checker
Check Your Medication Interaction
Select your mood stabilizer and another medication to see potential interactions and safety recommendations.
Select your medications to see interaction details.
When you're managing bipolar disorder, finding the right mood stabilizer is just the first step. The real challenge often comes later-when other medications, even common ones like ibuprofen or blood pressure pills, start changing how your mood stabilizer works. Lithium, valproate, and carbamazepine are the three oldest and still most widely used mood stabilizers. But they don’t play well with everything. A simple over-the-counter painkiller can push lithium into dangerous territory. A seizure drug might make your carbamazepine stop working-or make you dizzy and unsteady. These aren’t rare side effects. They’re predictable, well-documented, and often preventable-if you know what to look for.
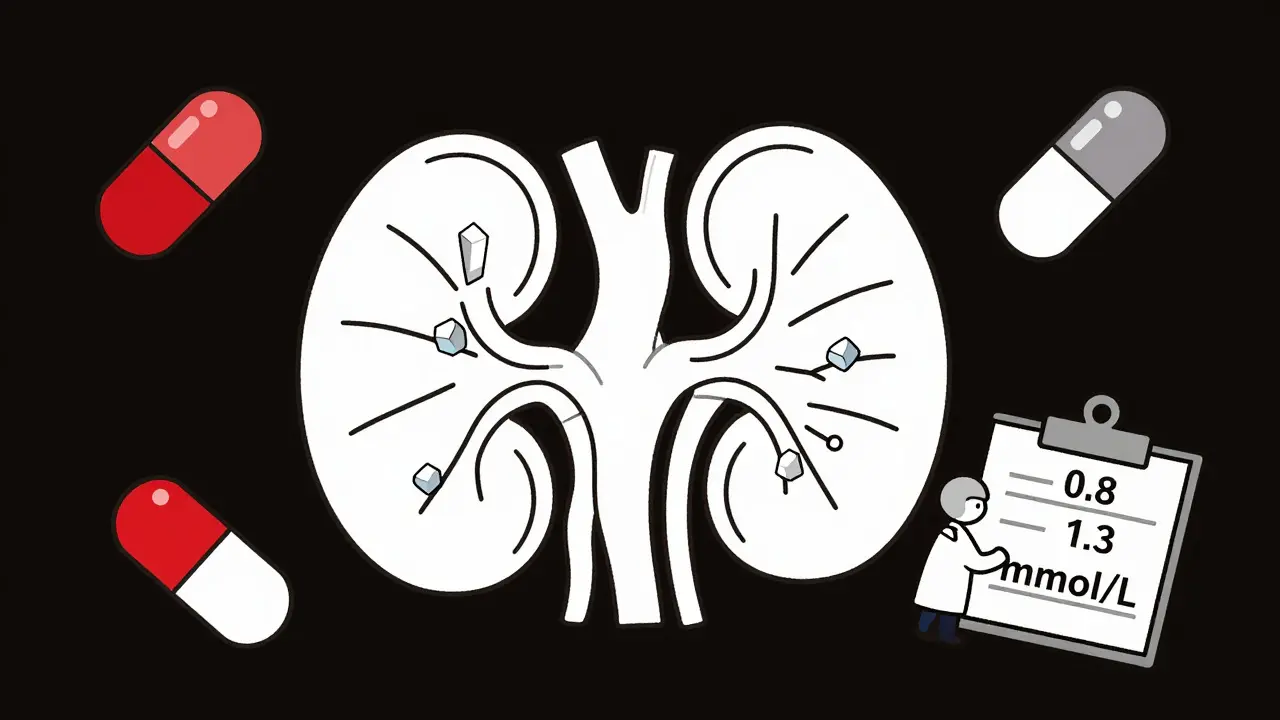
Lithium: The Kidney-Sensitive Stabilizer
Lithium is unique. Unlike most drugs, it doesn’t get broken down by the liver. It leaves your body through your kidneys, unchanged. That’s why anything that affects your kidney function or sodium balance can change lithium levels in your blood-sometimes in just a few days.
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen are the most common culprits. They reduce blood flow to the kidneys, which means less lithium gets filtered out. Studies show this can raise lithium levels by 25-30%. One patient on NAMI’s forum saw their lithium level jump from 0.8 to 1.3 mmol/L after starting ibuprofen for a headache. That’s not just a number-it’s tremors, confusion, nausea, and the risk of seizures.
Diuretics (water pills) like hydrochlorothiazide are another silent danger. They make you lose sodium, and your kidneys respond by holding onto lithium instead. Research from the 1980s showed lithium levels can rise 25-40% with these drugs. Even ACE inhibitors, common for high blood pressure, can do the same. In one 2002 case series, patients on lisinopril saw lithium levels climb by about 25%.
The fix? Don’t stop your painkiller or blood pressure med-just monitor. Guidelines now recommend checking lithium levels 5-7 days after starting any new medication that affects the kidneys. Keep your lithium level on the lower end of safe (0.6-0.8 mmol/L) if you’re taking these drugs. Stay hydrated. Avoid extreme heat or heavy sweating. And if you feel shaky, confused, or nauseous, get your level checked immediately.
Valproate: The Protein-Binding Wildcard
Valproate works differently. It’s highly bound to proteins in your blood-up to 90% at normal levels. But here’s the twist: when levels go above 100 mcg/mL, that binding starts to saturate. More free valproate floats around, increasing the risk of side effects like drowsiness or liver stress-even if your total level looks “normal.”
Valproate also interferes with how other drugs are broken down. It’s a strong inhibitor of UGT enzymes, which means it can double or even triple the levels of drugs like lamotrigine. One Reddit user reported their lamotrigine dose had to be cut in half-from 400 mg to 200 mg-after switching from carbamazepine to valproate. That’s not an anomaly. It’s standard pharmacology.
But valproate isn’t immune to being affected itself. Carbamazepine, a powerful enzyme inducer, speeds up valproate’s breakdown. Studies show carbamazepine can reduce valproate levels by 30-50%. That means someone on both drugs might seem stable-but if you stop carbamazepine, valproate levels can spike, causing toxicity. That’s why switching between these two requires careful planning and frequent blood tests.
There’s another layer: valproate can displace other protein-bound drugs like warfarin or phenytoin, making them more active. A patient on warfarin for atrial fibrillation could suddenly be at risk of bleeding if valproate is added without adjusting the dose. It’s not just about mood-it’s about the whole body.
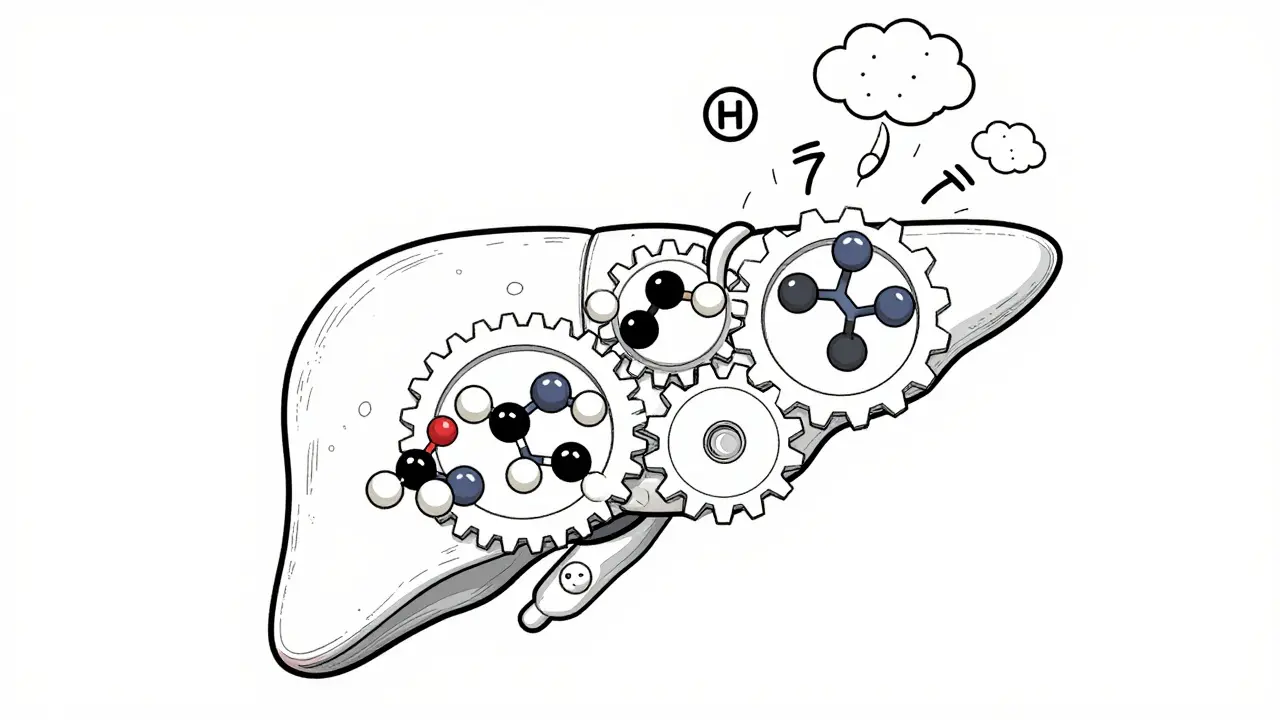
Carbamazepine: The Metabolism Changer
Carbamazepine is a metabolic powerhouse. It doesn’t just get broken down-it forces your liver to make more of the enzymes that break it down. This is called autoinduction. At first, your carbamazepine level might be stable. After 3-5 weeks, your body starts clearing it faster. The dose you started with may no longer be enough.
But the real complexity comes with valproate. For years, doctors thought valproate only blocked the enzyme that breaks down carbamazepine’s active metabolite (CBZ-E). New research shows it’s more complicated. Valproate also blocks the next step-turning CBZ-E into an inactive form. That means CBZ-E builds up. And CBZ-E is what causes dizziness, nausea, and loss of coordination. A 1997 study found CBZ-E levels jumped 40-60% when valproate was added-even though carbamazepine levels stayed the same.
Carbamazepine also speeds up the breakdown of many other drugs. Oral contraceptives? Their effectiveness drops by 50-70%. Antidepressants like sertraline? Levels fall. Antipsychotics like risperidone? Can drop by 40-60%. One patient on carbamazepine and birth control ended up pregnant despite perfect adherence. That’s not a failure of the pill-it’s a drug interaction.
Doctors now monitor both carbamazepine and CBZ-E levels when valproate is added. The goal? Keep CBZ-E below 3.5 mcg/mL. If it’s higher, reduce the carbamazepine dose by 25% and retest. This isn’t guesswork. It’s protocol.
Putting It All Together: What to Watch For
Here’s a quick reference for the biggest red flags:
- Lithium + NSAIDs, diuretics, or ACE inhibitors → Risk of toxicity. Check levels in 5-7 days.
- Valproate + lamotrigine → Lamotrigine levels double. Cut lamotrigine dose in half and monitor for rash.
- Carbamazepine + valproate → CBZ-E spikes. Monitor both drugs and reduce carbamazepine by 25%.
- Carbamazepine + birth control, antipsychotics, or antidepressants → Levels drop. Dose increases may be needed.
- Valproate + warfarin or phenytoin → Free drug levels rise. Watch for bleeding or seizures.
There’s no one-size-fits-all. Two people on the same drugs can have wildly different reactions. That’s why therapeutic drug monitoring isn’t optional-it’s essential. Blood tests for lithium, valproate, and carbamazepine aren’t just routine. They’re safety checks.
Why These Interactions Matter More Than Ever
Prescribing patterns are changing. Lithium use has dropped from 35% of new starts in 2012 to just 15% in 2022. Valproate, once the most common, is now used less in women of childbearing age because of its 10.7% risk of major birth defects. Carbamazepine holds steady at 10%-but its interaction profile makes it a last-resort option for many.
Meanwhile, lamotrigine, which has far fewer interactions, now accounts for 35% of new mood stabilizer prescriptions. That’s not because it’s more effective-it’s because it’s easier to manage. It doesn’t need frequent blood tests. It doesn’t interact with most other drugs. For many patients, that simplicity is worth more than the slightly higher cost.
But for those who still need lithium, valproate, or carbamazepine, understanding these interactions isn’t academic. It’s life-saving. A single NSAID can land someone in the ER. A missed blood test can lead to a manic episode. A poorly timed switch can cause seizures.
What You Can Do
If you’re on one of these drugs:
- Keep a list of every medication you take-prescription, over-the-counter, supplements, even herbal teas.
- Ask your doctor or pharmacist: “Could this interact with my mood stabilizer?” before starting anything new.
- Know your target levels: lithium (0.6-1.2 mmol/L), valproate (50-125 mcg/mL), carbamazepine (4-12 mcg/mL).
- Don’t ignore early warning signs: tremors, confusion, dizziness, nausea, or unusual fatigue.
- Make sure your blood tests are scheduled regularly. Don’t skip them just because you “feel fine.”
These drugs saved lives. But they’re not safe by default. Their power comes with responsibility. The best outcomes happen when patients, doctors, and pharmacists work together-not just to treat mood, but to protect the whole system.
Can I take ibuprofen if I’m on lithium?
Taking ibuprofen while on lithium can raise lithium levels by 25-30%, increasing the risk of toxicity. Symptoms include tremors, confusion, nausea, and dizziness. If you need pain relief, acetaminophen (Tylenol) is a safer choice. If you must use ibuprofen, get your lithium level checked within 5-7 days and keep your dose at the lower end of the therapeutic range (0.6-0.8 mmol/L).
Why does valproate make lamotrigine levels go up?
Valproate blocks the enzyme (UGT) that breaks down lamotrigine. This can increase lamotrigine levels by 100-200%. If you switch from carbamazepine to valproate, your lamotrigine dose may need to be cut in half. Watch for skin rash, which can be a sign of a serious reaction. Always adjust lamotrigine under medical supervision.
Does carbamazepine reduce the effectiveness of birth control?
Yes. Carbamazepine speeds up the breakdown of hormones in birth control pills, patches, and rings, reducing their effectiveness by 50-70%. This can lead to unintended pregnancy. If you’re on carbamazepine, use a non-hormonal method like an IUD or condoms. If you must use hormonal birth control, your doctor may need to increase the dose-but this isn’t always reliable.
Can I take valproate and carbamazepine together?
Yes, but with caution. This combination increases levels of carbamazepine’s active metabolite (CBZ-E), which can cause dizziness, loss of coordination, and nausea. Doctors usually reduce the carbamazepine dose by 25% when starting valproate and monitor both drug levels. CBZ-E should stay below 3.5 mcg/mL. This combo is used when other options fail, but it requires close monitoring.
How often should I get my mood stabilizer levels checked?
When starting or changing a medication, check levels within 5-7 days. Once stable, most patients need checks every 3-6 months. But if you start a new drug, get sick, change your diet, or notice new symptoms, get tested immediately. Lithium levels should be checked more frequently than valproate or carbamazepine because they change faster and are more sensitive to small changes.


Comments
Bryan Wolfe
Just wanted to say this post saved my life last year when I started on lithium and kept grabbing ibuprofen for headaches-didn’t realize how dangerous it was until I got dizzy and nearly passed out. Got my levels checked and switched to Tylenol. Now I keep a note on my phone: "NO NSAIDS WITH LITHIUM." Thank you for making this so clear!
Sumit Sharma
Incorrect. The 25-30% increase in lithium levels with NSAIDs is not universally applicable-it's pharmacokinetic variability dependent on CYP2D6 and renal perfusion status. You're oversimplifying clinical pharmacology. The real issue is lack of TDM adherence, not drug class associations. Always correlate with serum creatinine and eGFR before attributing toxicity to NSAIDs alone.
Jay Powers
I’ve been on carbamazepine for 12 years and valproate for 3. The dizziness? Real. The confusion? Real. I thought I was just getting older until my psychiatrist checked CBZ-E levels and found them at 4.1. We dropped my carbamazepine by 25% and boom-clarity returned. This isn’t theoretical. It’s lived. Keep testing. Keep asking. You’re not paranoid if your meds are acting weird.
Lawrence Jung
Everyone talks about the drugs but nobody talks about the system. Why do we rely on blood tests to catch what should be obvious? Why is it still the patient’s job to memorize interactions while doctors scroll through their phones during 10-minute visits? This isn’t medicine. It’s triage with a prescription pad. We’re not patients-we’re data points with lithium levels
Alice Elanora Shepherd
Important note: Valproate’s protein-binding saturation above 100 mcg/mL is often missed because labs report total levels, not free. If you’re feeling unusually drowsy or nauseated despite "normal" levels-ask for a free valproate level. It’s not always covered by insurance, but it’s critical. Also, avoid grapefruit juice with all three-CYP3A4 inhibition is real.
Christina Widodo
Wait-so if I’m on lamotrigine and my doctor switches me from carbamazepine to valproate, do I just cut my dose in half immediately? Or do I taper? I’ve read conflicting stuff online. My last psychiatrist just said "trust me" and I ended up with a rash that scared the hell out of me.
Prachi Chauhan
My mom was on lithium and took Advil for her arthritis. She ended up in hospital. I didn’t know anything about meds back then. Now I’m studying pharmacy. This post? It’s everything. I’m going to make sure no one else’s mom goes through that. Thank you for writing it.
Katherine Carlock
Just had my first blood test in 8 months because I started taking melatonin for sleep. My doctor said it’s fine, but now I’m paranoid. Should I get checked anyway? I don’t want to be that person who shows up with a meltdown because I didn’t ask. Also-anyone else feel like their meds are a full-time job?
Sona Chandra
THIS IS WHY PEOPLE DIE. I lost my cousin because he was on carbamazepine and his doctor gave him sertraline without adjusting. He had a seizure at work. No one told him. No one checked his levels. Now he’s in a wheelchair. Don’t be that doctor. Don’t be that patient. READ THE FUCKING INTERACTIONS.
Jennifer Phelps
Can someone explain why CBZ-E matters more than carbamazepine itself? I keep seeing that number but no one ever says what it actually does to your body. Is it just dizziness or is it damaging something?
beth cordell
Thank you for this 🙏 I’m on lithium + lisinopril and was terrified to ask my doctor because I didn’t want to sound "neurotic." Now I know to get tested in 5 days. Also-TYSM for mentioning hydration. I drank so much water after reading this. My kidneys are crying tears of joy 💧❤️
Lauren Warner
Let’s be real-most of these interactions are avoidable if doctors actually read the damn drug monographs. But they don’t. They rely on pharmacy alerts that are outdated or buried under 200 other pop-ups. The real problem isn’t patients. It’s a broken system that treats pharmacology like a suggestion box.
Craig Wright
While the information presented is technically accurate, the tone is overly alarmist. In the UK, we manage these interactions routinely under the NHS with structured monitoring protocols. The suggestion that patients must constantly self-monitor borders on irresponsible. Trust your clinician. The system works-if you follow it.
Bryan Wolfe
^This. I actually had my GP adjust my lisinopril dose after seeing the lithium interaction-she didn’t even blink. We just checked levels 5 days later. It’s not about fear. It’s about partnership. You’re not alone in this.