
SAMe & Antidepressant Interaction Risk Calculator
This tool estimates the potential risk of serotonin syndrome when combining SAMe with your antidepressant medication. Based on data from medical studies and FDA reports, this calculator provides an assessment of your specific situation.
Risk Assessment Result
Symptoms to Watch For
- Racing heart
- High blood pressure
- Muscle rigidity or twitching
- Confusion or hallucinations
- High fever
- Sweating or shivering
Critical Warning
DO NOT stop your antidepressant suddenly. Discontinuing antidepressants abruptly can cause withdrawal symptoms. Consult your doctor before making any changes to your medication regimen.
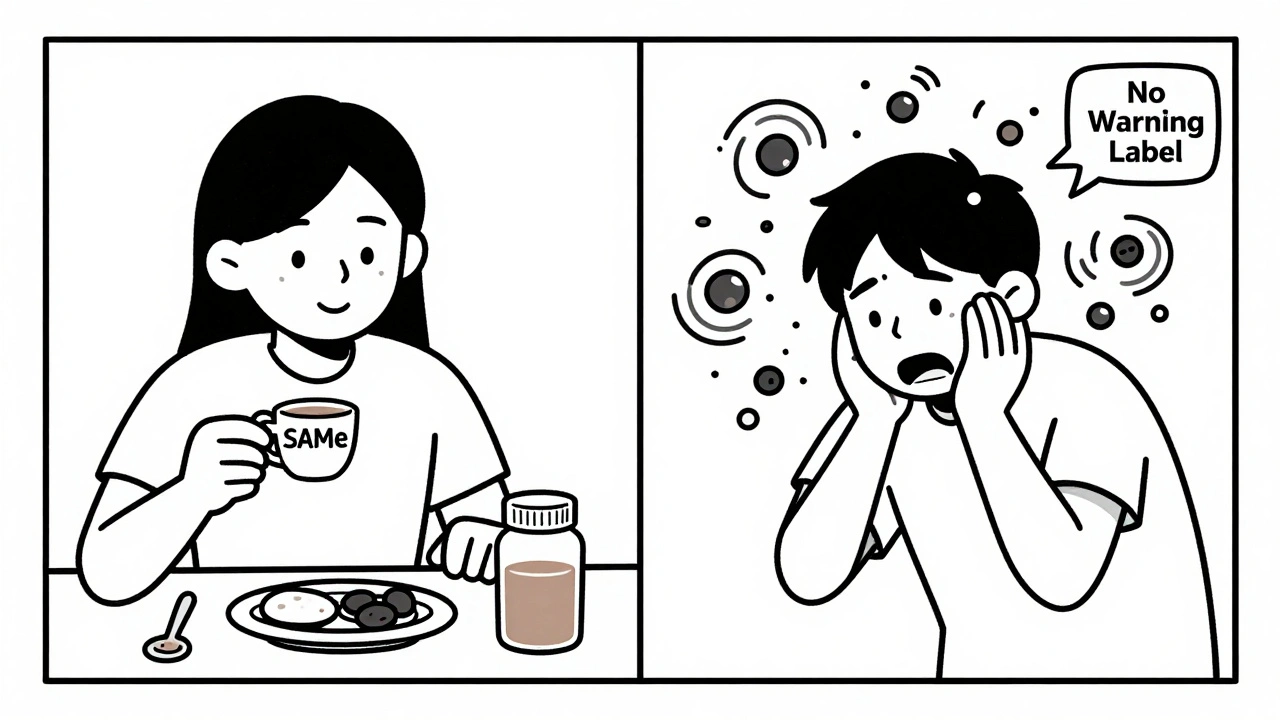
People turn to SAMe hoping for a natural lift when antidepressants aren’t enough. But combining SAMe with prescription antidepressants isn’t just risky-it can land you in the ER. This isn’t theoretical. Real people have ended up in hospitals after mixing the two. And yet, SAMe is sold right next to multivitamins on store shelves, with no warning labels that match the danger.
SAMe, or S-adenosylmethionine, is a compound your body makes naturally. It helps produce brain chemicals like serotonin, dopamine, and norepinephrine-the same ones antidepressants target. That’s why some people think adding SAMe to their meds might boost results. But here’s the problem: SAMe doesn’t just gently nudge these chemicals up. It pushes them hard. And when you stack it on top of an SSRI or SNRI, you’re turning up the volume on serotonin too far, too fast.
How SAMe Works (And Why It’s Not a Gentle Supplement)
SAMe doesn’t just act like a vitamin. It’s a methyl donor-meaning it directly fuels the chemical reactions that make serotonin and other mood-regulating neurotransmitters. In clinical trials, SAMe increased serotonin production by 20-30% compared to placebo. That’s not minor. That’s the same level of effect as adding a low-dose antidepressant.
It also inhibits monoamine oxidase, the enzyme that breaks down serotonin. That’s the same mechanism as older antidepressants like MAOIs, which are already known for dangerous interactions. So SAMe isn’t just helping your brain make more serotonin-it’s also slowing down how fast your body clears it out. Double the serotonin, half the clearance. That’s a recipe for trouble.
And it works fast. While SSRIs take weeks to kick in, SAMe can raise serotonin levels within hours. Peak concentrations hit your bloodstream in 3-5 hours. That’s why some people feel a lift within days-but why others suddenly feel off, anxious, or even terrified within 48 hours of starting it.
The Real Risk: Serotonin Syndrome
Serotonin syndrome isn’t a myth. It’s a life-threatening condition caused by too much serotonin in the brain. Symptoms include:
- Racing heart
- High blood pressure
- Muscle rigidity or twitching
- Confusion or hallucinations
- High fever
- Sweating or shivering
One Reddit user, u/DepressionWarrior2020, started 400mg of SAMe with 20mg of Prozac. Three days later, he was in the ER with muscle rigidity, a heart rate over 130, and confusion. His doctors confirmed serotonin syndrome. He wasn’t alone. Between 2000 and 2022, only 12 published case reports existed. But the FDA’s adverse event database shows 32 SAMe-related incidents involving antidepressants between 2018 and 2022-with 9 classified as serious. Two of those were confirmed serotonin syndrome cases.
And here’s the scary part: doctors don’t always catch it. SAMe is a supplement. Most prescribers don’t ask about it. Patients don’t think to mention it. The Natural Medicines Database rates this interaction as “Major-Use Caution” with a severity score of 7.3 out of 10. That’s the same level as mixing alcohol with benzodiazepines.
Who’s Actually Using SAMe With Antidepressants?
According to the 2022 National Health Interview Survey, 68% of Americans who take SAMe for depression are already on prescription antidepressants. That’s not a small group-it’s millions of people. Many believe they’re being smart: “If my Zoloft isn’t working, maybe adding something natural will help.”
Some do report success. One user on Healthline shared that after six months of partial response to Zoloft, her doctor added 800mg of SAMe. Her PHQ-9 score dropped from 16 to 7. No side effects. She’s been fine for eight months.
But here’s the catch: her case is the exception, not the rule. The data shows SAMe works best as an add-on for mild-to-moderate depression, not severe cases. In severe depression, remission rates with SAMe are only 18%, compared to 42% with venlafaxine. And its effectiveness varies wildly-some people absorb 50% of the dose, others barely 15%. That’s why two people on the same dose can have totally different outcomes.

The Quality Problem You’re Not Being Told About
Not all SAMe is created equal. ConsumerLab.com tested 20 popular brands in 2022. One in three failed potency tests. Some contained only 75% of the SAMe listed on the label. That’s not just misleading-it’s dangerous. If you’re taking a low-dose product thinking you’re safe, but it’s actually delivering more than you expect, you’re playing Russian roulette with your brain chemistry.
And the labeling? Terrible. Only 37% of SAMe products include any warning about antidepressant interactions, according to a 2021 JAMA Internal Medicine analysis. Amazon reviews show 28% of negative feedback mentions stomach upset. But only a fraction mention the real danger: serotonin syndrome.
Even worse, the FDA has issued warning letters to three manufacturers for claiming SAMe treats depression-a claim that’s never been approved. That means you’re buying a product that’s not regulated for safety, efficacy, or interaction risks. It’s sold as a supplement, but it acts like a drug.
What If You’re Already Taking Both?
If you’re currently taking SAMe and an antidepressant, don’t stop either cold. Sudden withdrawal from antidepressants can cause brain zaps, dizziness, and worsening depression. Stopping SAMe abruptly can cause a rebound in low mood.
Here’s what to do instead:
- Call your doctor or psychiatrist. Tell them exactly what you’re taking, including dose and brand.
- Ask if your combination has been monitored before. If not, get a plan.
- Watch for symptoms: racing heart, muscle stiffness, confusion, fever, sweating. If any appear, go to urgent care immediately.
- Don’t increase your SAMe dose without medical supervision. Even going from 400mg to 800mg can tip the balance.
Some psychiatrists do use SAMe as an add-on-but only under strict rules. The American Society of Clinical Psychopharmacology recommends starting at 200mg twice daily, increasing by 200mg every 5-7 days, with weekly check-ins. They also advise avoiding SAMe entirely if you have bipolar disorder, because it can trigger mania.
Who Should Avoid SAMe Altogether?
SAMe isn’t safe for everyone. Avoid it if you:
- Are on any antidepressant (SSRI, SNRI, MAOI, tricyclic)
- Have bipolar disorder
- Are pregnant or breastfeeding
- Have a history of serotonin syndrome
- Take migraine meds like triptans
- Take pain meds like tramadol or dextromethorphan
Even if you’re not on antidepressants, SAMe can cause side effects. About 22% of users report increased anxiety in the first week. Others get nausea, insomnia, or headaches. Taking it with food helps reduce stomach upset in 65% of cases. Splitting doses (morning and afternoon) can prevent sleep issues.
The Bottom Line: It’s Not Worth the Risk
SAMe isn’t a magic bullet. It’s a powerful biochemical agent with real, documented dangers when mixed with antidepressants. The fact that it’s available without a prescription doesn’t make it safe-it makes it dangerous.
The European Food Safety Authority banned it in 2015. The American Psychiatric Association says there’s not enough evidence to recommend it routinely. And yet, 4.7 million Americans are using it for depression-with most combining it with prescription drugs.
If you’re struggling with depression and your current treatment isn’t working, talk to your doctor about evidence-based options: switching meds, adding psychotherapy, trying TMS, or exploring ketamine therapy. These have data behind them. They’re monitored. They’re regulated.
SAMe doesn’t belong on the same shelf as your vitamins. It belongs in a doctor’s office, under supervision, with clear protocols. Until then, the safest choice is simple: don’t mix it.


Comments
soorya Raju
bro the FDA is just in the pocket of big pharma anyway why do u think they let this stuff on shelves? they WANT us to get serotonin syndrome so we go back to pills lol. i took sam e with cipralex for 3 months and felt like a god. then my heart started beatin like a drum machine but i was too high to care. they call it syndrome i call it enlightenment.
Kshitij Shah
so let me get this straight - you're mad that a compound your body makes naturally is sold next to gummy vitamins? bro it's like getting mad that apples are next to candy bars. if you don't know how to use it, that's on you. not the store. not the FDA. you.
Priyam Tomar
you people are hilarious. SAMe is not a supplement - it's a biochemical weapon disguised as a wellness trend. if you're dumb enough to stack it with SSRIs without lab monitoring, you deserve the ER visit. i've seen 3 cases in my clinic. one guy thought he was "biohacking". ended up in ICU with a 104 fever and muscle spasms that looked like he was doing the robot. stop pretending natural = safe. your liver doesn't care about your vibes.
Kay Lam
I think what's really concerning here is how little education there is around supplements in general. People see something labeled natural and assume it's harmless. But the truth is the body doesn't distinguish between synthetic and natural chemicals - it just responds to the molecular structure. SAMe is a potent methyl donor and monoamine oxidase inhibitor. That's not a vitamin. That's pharmacology. And if you're not talking to a prescriber who understands neurochemistry, you're playing with fire. I've had patients come in with tremors and confusion thinking they were just being "proactive". It's heartbreaking. We need better labeling. We need better public education. And we need to stop treating supplements like they're candy.
Adrian Barnes
The data is clear. The risk is severe. The regulatory failure is egregious. The fact that this compound is sold without prescription, without mandatory interaction warnings, and with inconsistent potency is a systemic failure of public health policy. The FDA's inaction is not negligence - it is complicity. This is not about individual responsibility. This is about corporate capture of regulatory bodies. The supplement industry operates as a legal loophole for pharmaceutical-grade compounds. And the public is the lab rat.
Linda Migdal
America lets this stuff fly under the radar while Europe bans it? That says everything. We're the land of the free and the home of the dumb. If you can't trust your own government to protect you from snake oil, what's next? Selling cyanide as "energy boosters"? This isn't about health. It's about capitalism eating its own children.
Tommy Walton
SAMe = serotonin turbo button 🚀💥 SSRIs = slow drip SAMe + SSRIs = 🤯🤯🤯 I'm not saying don't do it - I'm saying do it with a therapist, a heart monitor, and a backup plan. Also, get a dog. Dogs calm your soul.
James Steele
The irony is palpable. We live in a post-Enlightenment world where biochemical manipulation is normalized via pharmaceuticals, yet any attempt to augment that system with endogenous compounds is vilified as "unregulated". SAMe isn't dangerous because it's natural - it's dangerous because it's *effective*. The system fears efficacy without profit margins. The real conspiracy isn't the supplement - it's the medical-industrial complex's refusal to acknowledge non-patentable interventions.
Louise Girvan
I'm not saying you're wrong... but... I'm also not saying you're right... and I'm terrified... what if I'm already having it and don't know it? I've had racing heart for weeks... is it SAMe? Is it anxiety? Is it... is it... the end? I need to know... I need to know NOW... I'm shaking...
Dennis Jesuyon Balogun
In Nigeria, we have a saying: "If the medicine is sold beside bread, it must be treated like bread." But here, they sell it beside multivitamins and call it wellness. This is not about science. This is about colonial capitalism - selling dangerous biochemistry to the masses as self-care. The West has turned healing into a consumer product. And the price? Your nervous system.
Grant Hurley
i just took 400mg of sam e last week with my zoloft and honestly? felt way better. no side effects. maybe im just lucky? my doc said "eh its fine" so idk. maybe everyone else is just overreacting? also i ate a burrito yesterday so i guess everything is fine lol
Lucinda Bresnehan
I just want to say - if you're reading this and you're on SAMe and antidepressants - please don't panic. But please, please, please talk to someone. Your pharmacist, your doctor, a friend who's been there. You're not alone. I was on 800mg SAMe with Lexapro for 11 months. I had mild nausea and a weird energy buzz for the first 48 hours - then it just... settled. My mood improved. My sleep got better. But I had blood tests every 6 weeks. I tracked my symptoms. I didn't just wing it. You can do this safely - but you have to be intentional. This isn't about fear. It's about responsibility.
Shannon Gabrielle
So let me get this straight - you’re mad because people are using a compound that actually works, instead of waiting 6 weeks for a pill that makes them feel like a zombie? Congrats. You just described every single antidepressant ever made. If SAMe gives someone their life back, who are you to take that away because it’s not FDA-approved? The real crime is that we’ve normalized chemical sedation over natural biochemistry. Wake up.
ANN JACOBS
I just want to take a moment to say that mental health is deeply personal, and everyone's journey is different. I've seen people struggle for years with depression, and for some, SAMe has been the turning point - not a miracle, but a bridge. I understand the risks, and I understand the data, and I understand the fear. But I also understand that when someone has tried everything and still feels broken, they will grasp at anything that offers even a sliver of hope. And maybe - just maybe - if we had better education, better labeling, better access to medical guidance, we wouldn't need to fear this so much. We could guide it. We could harness it. We could turn this from a dangerous gamble into a legitimate tool. That’s not conspiracy. That’s compassion.