Blood Sugar During Pregnancy: What You Need to Know About Risks, Management, and Safe Medications
When you're pregnant, your body changes how it handles blood sugar, the level of glucose in your bloodstream that fuels your cells and your growing baby. Also known as glucose, it’s not just a number—it’s a signal that tells you if your body is keeping up with the extra demands of pregnancy. Around 6 to 9% of pregnant people develop gestational diabetes, a type of diabetes that starts during pregnancy when hormones interfere with insulin’s ability to regulate glucose. It’s not your fault. It’s not because you ate too much sugar. It’s because pregnancy naturally makes your body more resistant to insulin to ensure your baby gets enough energy. But when that resistance goes too far, your blood sugar climbs—and that’s where problems start.
Untreated high blood sugar during pregnancy doesn’t just affect you. It can lead to a larger baby, which raises the risk of birth injuries, C-sections, and future obesity or type 2 diabetes for your child. For you, it increases the chance of preeclampsia, preterm labor, and developing type 2 diabetes later in life. The good news? Most cases are manageable with diet, movement, and, when needed, safe medications like insulin during pregnancy, a treatment that doesn’t cross the placenta and is considered the gold standard for controlling glucose when lifestyle changes aren’t enough. Unlike some oral diabetes pills, insulin is trusted because it doesn’t reach the baby. Other options like metformin are sometimes used, but insulin remains the most predictable and safest choice for many.
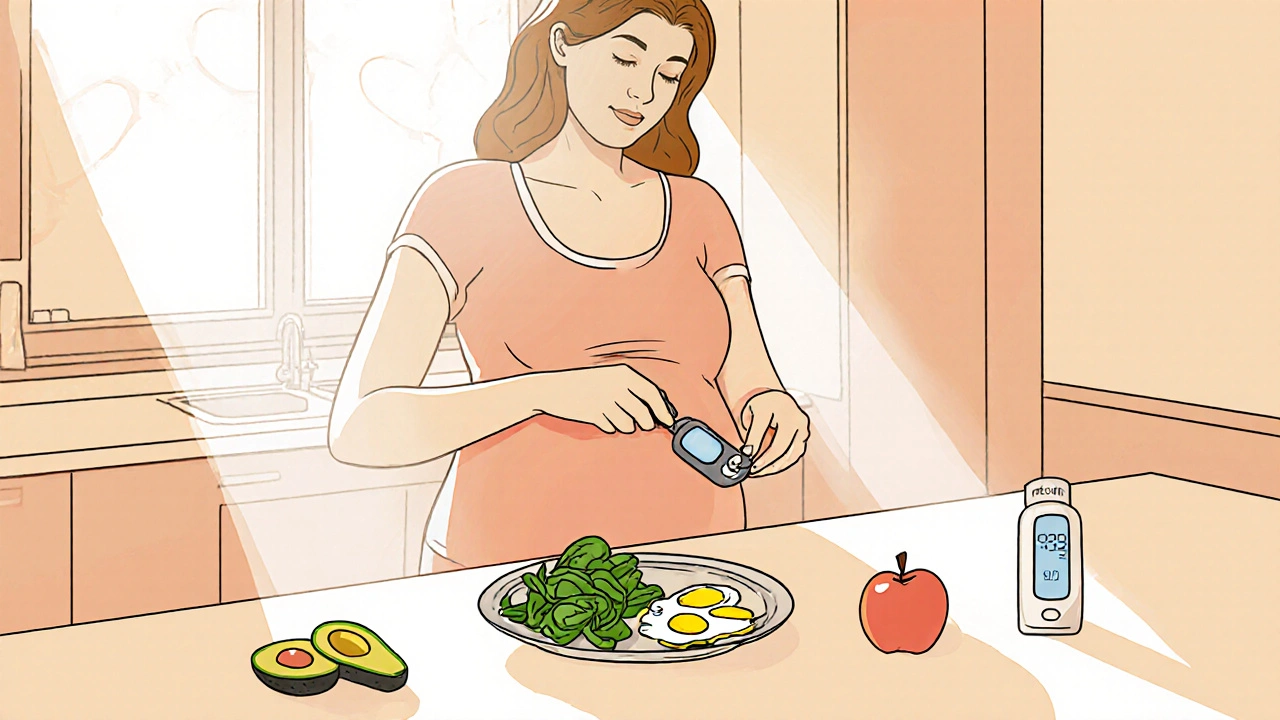
Monitoring is key. You won’t always feel high blood sugar. That’s why checking your levels with a glucometer—often four times a day—is standard practice. You’ll learn how your meals, activity, and even stress affect your numbers. Many people find that eating smaller, balanced meals with more fiber and less refined carbs helps keep things steady. Walking after meals is one of the most effective, natural ways to lower post-meal spikes. And if your doctor suggests insulin, don’t panic. It’s not a failure. It’s a tool. Think of it like wearing a seatbelt—you’re not in an accident yet, but you’re protecting both of you just in case.
The posts below cover what really matters: how to interpret your glucose readings, which medications are safe and why, how gestational diabetes connects to thyroid health and other conditions, and what happens after delivery. You’ll find practical advice from real experiences, not just textbook definitions. Whether you’re newly diagnosed or trying to understand your next lab result, these guides help you take control without overwhelm.
Gestational Diabetes: How to Manage Blood Sugar During Pregnancy
Learn how to manage gestational diabetes through diet, exercise, and blood sugar monitoring to ensure a healthy pregnancy and reduce long-term risks for both mother and baby.
read more