Corticosteroid-Responsive Dermatoses: What They Are and How They’re Treated
When your skin turns red, itchy, or flaky, and nothing seems to help—until you use a steroid cream and it clears up—that’s often a corticosteroid-responsive dermatoses, a group of skin conditions that improve significantly with topical or systemic corticosteroids. Also known as steroid-sensitive rashes, these aren’t one single disease but a category of inflammatory skin disorders that respond predictably to anti-inflammatory treatment. This includes common issues like eczema, contact dermatitis, and some forms of psoriasis. The key clue? If a steroid cream makes it better, it’s likely in this group.
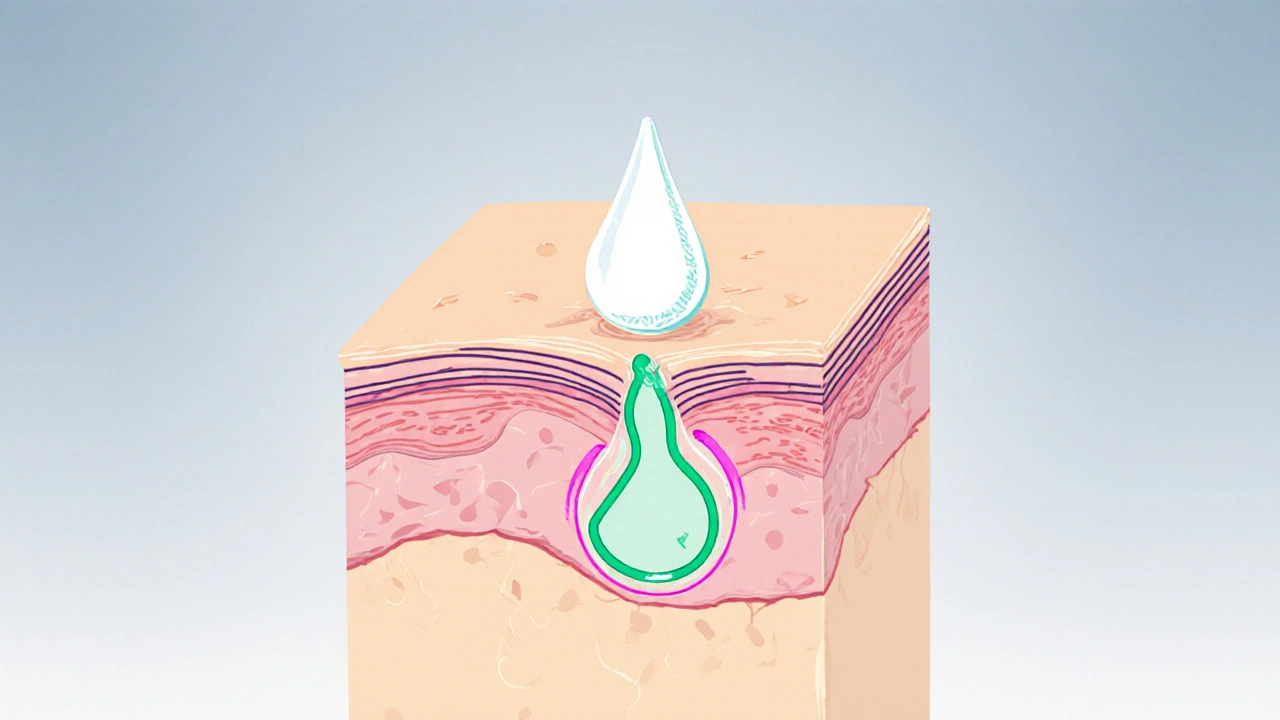
What makes these conditions different from other rashes? Many skin problems—like fungal infections, viral outbreaks, or allergic reactions—won’t budge with steroids. But with corticosteroid-responsive dermatoses, the inflammation is driven by your immune system overreacting to something harmless, like soap, dust, or even your own skin’s natural barrier breaking down. That’s why steroids work: they quiet that overactive immune response. You’ll often see these in people with a history of allergies, asthma, or sensitive skin. And while they can show up anywhere, they favor the folds of the elbows, behind the knees, on the face, and around the eyes.
Not all steroid creams are the same. Mild ones like hydrocortisone 1% are fine for short-term use on the face or sensitive areas. Stronger versions—like clobetasol or betamethasone—are reserved for thicker plaques or stubborn patches on the body, and only for limited periods. Overuse can thin the skin, cause stretch marks, or even make the rash worse over time. That’s why treatment isn’t just about slathering on cream—it’s about knowing when to start, when to stop, and how to maintain results with moisturizers, gentle cleansers, and avoiding triggers. Some people need to use steroids intermittently, like a fire extinguisher for flare-ups, while others benefit from combining them with non-steroid options like calcineurin inhibitors or barrier repair creams.
Looking at the posts here, you’ll find real-world examples of how these conditions overlap with other skin issues. One article breaks down how to pick makeup that won’t trigger flare-ups—critical for anyone with eczema or contact dermatitis. Another explains how nickel allergy leads to contact dermatitis, a classic corticosteroid-responsive condition. You’ll also see guides on managing side effects from other medications that can worsen skin inflammation, like certain blood pressure drugs or antidepressants. There’s even a piece on how stress affects your skin’s barrier, which can make these rashes worse. This isn’t just about creams—it’s about understanding the whole picture: what sets off the flare, how to calm it, and how to keep it from coming back.
Whether you’re dealing with a stubborn rash that keeps returning, or you’ve been told your skin condition responds to steroids and want to know why, this collection gives you the practical, no-fluff info you need. You’ll find what works, what doesn’t, and how to use steroids safely without falling into common traps. The goal isn’t just to treat the rash—it’s to understand your skin well enough to prevent the next one.
Halobetasol: How It Works for Corticosteroid‑Responsive Skin Conditions
Learn how halobetasol works, its approved uses, safety profile, and practical tips for treating corticosteroid‑responsive skin conditions effectively.
read more