Gestational Diabetes: What You Need to Know About Risks, Management, and Safe Medications
When you’re pregnant, your body changes in ways you can’t always control—and one of the most common is gestational diabetes, a type of diabetes that develops during pregnancy when the body can’t make enough insulin to handle rising blood sugar levels. Also known as pregnancy diabetes, it usually goes away after birth but raises your risk for type 2 diabetes later. About 1 in 10 pregnant women get it, and it’s not your fault—it’s biology, not lifestyle. The good news? With the right care, most women with gestational diabetes have healthy babies.
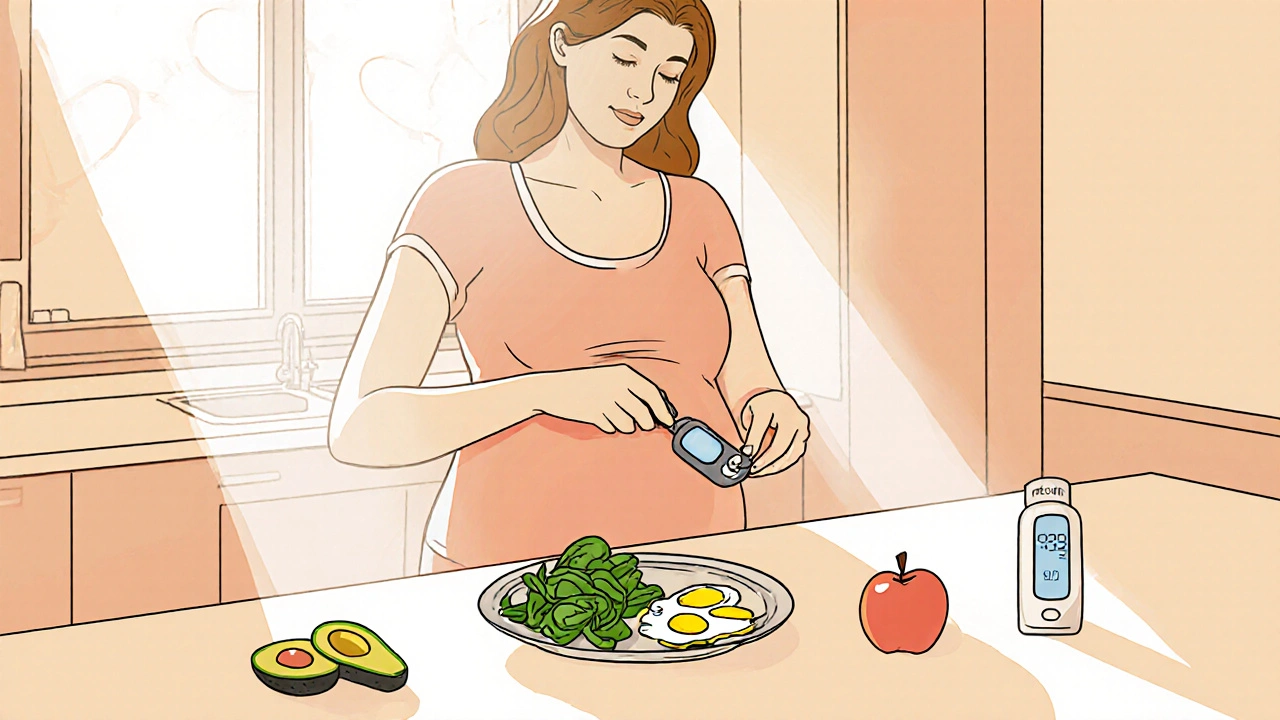
What makes gestational diabetes tricky is that it often has no symptoms. That’s why routine screening between 24 and 28 weeks is standard. If your blood sugar is high, your doctor might recommend changes to your diet, daily walks, or even insulin in pregnancy, a safe, non-oral treatment that doesn’t cross the placenta and won’t harm the baby. Unlike some oral diabetes pills, insulin is the go-to when food and exercise aren’t enough. You might also hear about metformin, an oral medication sometimes used off-label for gestational diabetes, though insulin remains the gold standard in the U.S.. The goal isn’t to eliminate sugar completely—it’s to keep your levels steady so your baby doesn’t grow too large or face other complications like low blood sugar at birth.
Managing gestational diabetes isn’t just about numbers on a glucose meter. It’s about understanding how your body reacts to food, stress, and sleep—all of which affect blood sugar. Many women find that eating smaller, balanced meals every few hours helps. Carbs aren’t the enemy; it’s the type and timing that matter. And while some worry about taking meds during pregnancy, the real danger is uncontrolled blood sugar. Studies show that babies of mothers with poorly managed gestational diabetes are more likely to need NICU care, have jaundice, or develop obesity and diabetes later in life.
You’ll also see how this connects to other pregnancy-related health topics. For example, if you’re managing gestational diabetes, you might also be monitoring thyroid levels—since thyroid function changes during pregnancy and affects insulin sensitivity. Or you might be using a CGM, a continuous glucose monitor that gives real-time trends, helping you adjust meals and activity to stay in range, just like people with type 1 diabetes do. Some of the same principles apply: watch your trends, don’t wait for highs or lows to hit before acting, and work with your care team to find what works.
There’s no one-size-fits-all plan, and that’s why the posts below cover everything from how to adjust your diet without feeling deprived, to what medications are safe (and which ones to avoid), to how to read your glucose logs like a pro. You’ll find real advice from people who’ve been there, backed by clinical data—not guesswork. Whether you’ve just been diagnosed or you’re preparing for your next pregnancy, this collection gives you the tools to take control—without fear or confusion.
Gestational Diabetes: How to Manage Blood Sugar During Pregnancy
Learn how to manage gestational diabetes through diet, exercise, and blood sugar monitoring to ensure a healthy pregnancy and reduce long-term risks for both mother and baby.
read more