Hypertension Guidelines: What You Need to Know About Blood Pressure Management
When it comes to hypertension guidelines, official recommendations from medical groups that define how to diagnose, treat, and monitor high blood pressure. Also known as blood pressure management protocols, these guidelines are updated every few years based on new data from large studies like SPRINT and ACCORD. They’re not just for doctors—they’re your roadmap to avoiding heart attacks, strokes, and kidney damage. If your blood pressure is consistently above 130/80, you’re in the range where guidelines say action is needed, even if you feel fine.
These guidelines don’t just say "take a pill." They tie treatment to your overall cardiovascular risk, your chance of having a heart attack or stroke in the next 10 years, based on age, cholesterol, diabetes, smoking, and other factors. Someone with diabetes and high blood pressure gets different advice than a healthy 45-year-old with just elevated numbers. The goal isn’t to hit a number—it’s to protect your organs. That’s why lifestyle changes like cutting salt, losing weight, and moving more come first, even before meds. And if you do need medication, the guidelines push for combinations that work better and have fewer side effects than old-school single-drug approaches.
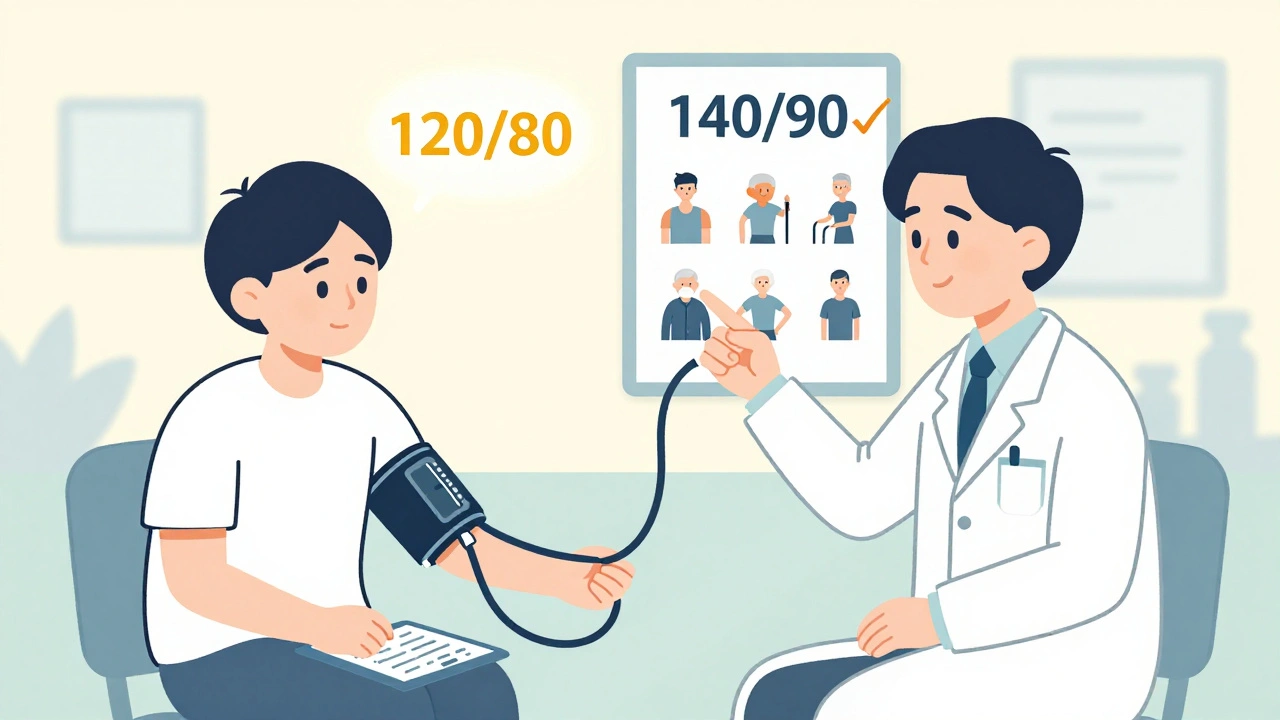
One big shift in recent guidelines is how aggressively we treat older adults. Ten years ago, doctors were told to aim for 140/90 in people over 60. Now, studies show lowering it to 120/80 cuts stroke risk by nearly a third—but only if you can do it safely. That’s why antihypertensive drugs, medications like ACE inhibitors, ARBs, calcium channel blockers, and thiazide diuretics used to lower blood pressure are chosen carefully. Some work better for Black patients, others are safer if you have kidney disease or heart failure. There’s no one-size-fits-all. And the guidelines warn against overtreating: going too low can cause dizziness, falls, or kidney problems, especially in older people.
You’ll also notice that guidelines now focus more on home monitoring than clinic visits. A single reading at the doctor’s office can be misleading—white coat hypertension is real. That’s why they recommend tracking your numbers at home with a validated device. If your average home reading is above 135/85, that’s just as concerning as a high reading in the office. And they’re clear: if your blood pressure stays high despite meds, don’t just crank up the dose. Look for hidden causes—sleep apnea, kidney issues, or even too much salt in your diet.
What you’ll find in the posts below isn’t just a list of drug names or numbers. It’s real-world context: how certain meds affect your kidneys, why some blood pressure drugs make you dizzy, what happens when you mix them with common painkillers, and how to tell if your treatment is actually working. These aren’t theory pieces—they’re based on what patients actually experience, what pharmacists see daily, and what the latest studies confirm. You’ll learn how to talk to your doctor, spot red flags in your meds, and avoid common mistakes that make hypertension harder to control.
Blood Pressure Targets: 120/80 vs. Individualized Goals for Better Heart Health
Should your blood pressure target be 120/80 or something higher? New guidelines show individualized goals often work better than rigid numbers. Learn what's right for your age, health, and lifestyle.
read more