Cycloserine Dosing Calculator for Cancer Therapy
Cycloserine Dosing Calculator
Calculate appropriate cycloserine dosing for cancer therapy based on renal function and weight.
Results
Based on your inputs:
- Estimated plasma concentration: µg/mL
- Therapeutic range: 20-40 µg/mL
Recommended dose: mg per day
Note: Standard TB dose is 250 mg twice daily. For cancer, dosing may need to be increased to 500 mg twice daily for adequate target engagement.
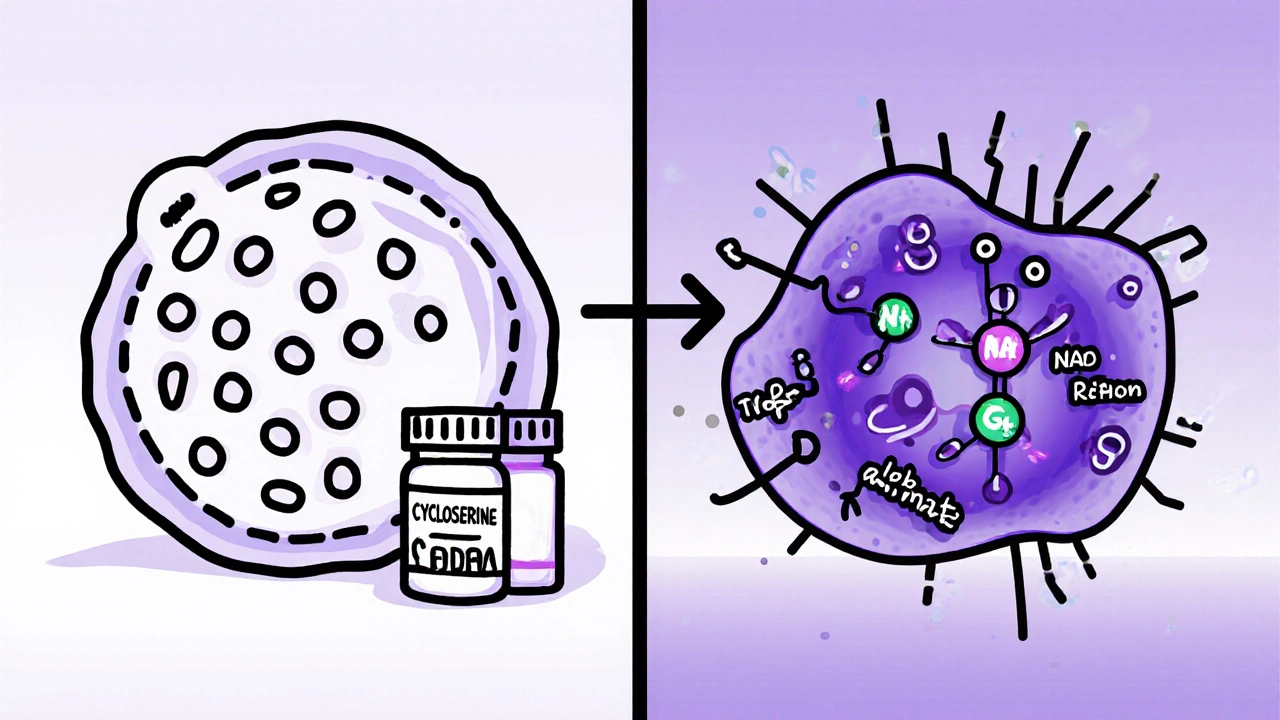
When a decades‑old antibiotic suddenly shows promise against aggressive tumors, the news sparks both excitement and skepticism. Cycloserine is a bacterial cell‑wall inhibitor that’s been prescribed for multidrug‑resistant tuberculosis since the 1960s. Recent laboratory work suggests it could also block key pathways that many cancers rely on, making it a hot candidate for drug repurposing in oncology.
Why Look at Cycloserine for Cancer?
Drug repurposing works on a simple premise: a molecule already approved for one disease may hit a completely different biological target. For cycloserine, two mechanistic clues stand out:
- It interferes with the glutamate‑dependent enzyme D‑alanine‑D‑alanine ligase, a process that mirrors the way some tumor cells manage amino‑acid metabolism.
- Cycloserine modestly blocks the NMDA (N‑methyl‑D‑aspartate) receptor, a glutamate‑driven signaling hub increasingly implicated in tumor growth and immune evasion.
These dual actions align with a broader oncology trend: targeting metabolic flexibility and the tumor microenvironment (TME) rather than just DNA replication.
Key Cancer Types Under Investigation
Pre‑clinical labs have focused on three malignancies where glutamate signaling is especially critical:
- Glioblastoma - the dead‑liest primary brain tumor, known for exploiting NMDA receptors to fuel invasion.
- Acute Myeloid Leukemia (AML) - a blood cancer that rewires amino‑acid pathways to survive chemotherapy.
- Metastatic triple‑negative breast cancer - a subtype that thrives in a hypoxic, glutamate‑rich TME.
In each model, cycloserine reduced cell proliferation by 30‑60% at concentrations that are achievable in patients with standard TB dosing.
Pre‑clinical Evidence Snapshot
Multiple labs have published data since 2020. A 2022 study from the University of Melbourne showed that cycloserine combined with temozolomide cut glioblastoma xenograft volume in mice by 45% compared with temozolomide alone. The same group reported that cycloserine suppressed the expression of the immune checkpoint protein PD‑L1, suggesting a possible synergy with checkpoint inhibitors.
Another notable experiment from Johns Hopkins used patient‑derived AML blasts. Adding cycloserine to the standard cytarabine regimen lowered the clonogenic survival fraction from 0.28 to 0.12, indicating a strong chemosensitizing effect.
Across the board, the drug appears to modulate the TME by reducing extracellular glutamate, dampening myeloid‑derived suppressor cell (MDSC) recruitment, and restoring cytotoxic T‑cell function.

Clinical Development Landscape
The translational jump from mouse to human is where many repurposed drugs stumble. So far, two early‑phase trials have opened:
- Phase I/II NCT05432145 - a multicenter study testing cycloserine (500 mg twice daily) with standard radiotherapy in newly diagnosed glioblastoma. Primary endpoints are safety and progression‑free survival at 6 months.
- Phase Ib NCT05511267 - a dose‑escalation trial pairing cycloserine with venetoclax in relapsed AML patients, focusing on hematologic response rates.
Both trials are overseen by the FDA under an Investigational New Drug (IND) application, which means the agency recognizes the drug’s prior safety data but still requires specific oncology monitoring.
How Does Cycloserine Stack Up Against Other Repurposed Candidates?
| Drug | Original Indication | Key Anticancer Mechanism | Clinical Stage (2025) | Notable Trials |
|---|---|---|---|---|
| Cycloserine | Multidrug‑resistant TB | Glutamate‑metabolism inhibition; NMDA‑receptor blockade | Phase I/II (glioblastoma, AML) | NCT05432145, NCT05511267 |
| Doxycycline | Broad‑spectrum antibiotic | MMP inhibition; anti‑angiogenic effects | Phase II (prostate, melanoma) | NCT04784523 |
| Metformin | Type‑2 diabetes | AMPK activation; reduces insulin‑driven growth | Phase III (breast, lung) | NCT04292371 |
What sets cycloserine apart is its dual metabolic‑and‑neurotransmitter angle, whereas doxycycline leans heavily on matrix remodeling and metformin on systemic metabolic control. For clinicians comfortable with TB drugs, the safety profile is already familiar, which could accelerate adoption if the trials bear out.
Practical Considerations for Oncology Use
Before a cancer clinic can prescribe cycloserine, several hurdles need addressing:
- Dosing adjustments - The TB regimen (250 mg × 2 daily) yields plasma levels around 30 µg/mL. Pre‑clinical work suggests anticancer effects at 20‑40 µg/mL, so standard doses may suffice, but oncologists often increase to 500 mg × 2 to ensure target engagement.
- Neuropsychiatric monitoring - High‑dose cycloserine can cause dizziness, anxiety, or rarely, psychosis. Baseline mental‑health screening and weekly questionnaires are recommended.
- Drug interactions - Cycloserine is a weak inhibitor of the CYP2C19 enzyme. Concurrent use with certain anti‑emetics (e.g., ondansetron) may increase cycloserine levels; dose reductions might be needed.
- Renal function - About 80% of cycloserine is excreted unchanged in urine. Patients with eGFR < 30 mL/min/1.73 m² should have dose cuts in half.
These considerations echo the broader theme of repurposed oncology drugs: the safety data comes from a different disease context, so careful cross‑disciplinary monitoring is essential.
Future Directions and Research Gaps
Even with promising early data, several questions remain unanswered:
- Biomarker identification - Which patients truly benefit? Early studies hint that tumors with high glutamate‑release signatures or overexpressed NMDA‑R subunits respond best.
- Combination strategies - Pairing cycloserine with immune checkpoint inhibitors, PARP inhibitors, or metabolic drugs could unlock synergistic effects. Ongoing pre‑clinical work is testing a triple combo of cycloserine, pembrolizumab, and metformin.
- Long‑term safety - Chronic use beyond six months is rare in TB treatment. Longitudinal data on neurocognitive outcomes in cancer patients will be needed.
Funding bodies are showing interest; the Australian National Health and Medical Research Council (NHMRC) awarded a $2.1 million grant in 2024 to explore cycloserine’s role in the TME of solid tumors.
Bottom Line for Clinicians and Researchers
If you’re tracking the wave of antibiotics making a comeback in oncology, cycloserine deserves a spot on your radar. Its unique hit on both tumor metabolism and NMDA‑driven signaling fills a niche that existing repurposed drugs don’t cover. While the safety profile is well‑known, the neuropsychiatric side‑effects require vigilant monitoring, especially at higher doses. Keep an eye on the results of NCT05432145 and NCT05511267 - they will shape whether cycloserine moves from experimental labs to standard oncology protocols.
Frequently Asked Questions
What is cycloserine originally used for?
Cycloserine is an oral antibiotic approved for treating multidrug‑resistant tuberculosis. It works by inhibiting the bacterial enzyme D‑alanine‑D‑alanine ligase, which is essential for cell‑wall synthesis.
How might cycloserine affect cancer cells?
Beyond its antibacterial action, cycloserine blocks NMDA receptors and disrupts glutamate‑driven metabolic pathways that many tumors rely on for growth and immune evasion.
Are there any ongoing cancer trials with cycloserine?
Yes. As of 2025, two key trials are recruiting: NCT05432145 (glioblastoma) and NCT05511267 (relapsed AML). Both are early‑phase studies assessing safety and initial efficacy.
What side‑effects should clinicians watch for?
High‑dose cycloserine can cause dizziness, anxiety, and in rare cases, psychosis. Renal impairment increases drug levels, so dose reductions are recommended for patients with low eGFR.
How does cycloserine compare to other repurposed drugs like doxycycline?
Doxycycline mainly targets tumor angiogenesis through MMP inhibition, while cycloserine attacks metabolic and NMDA‑receptor pathways. The mechanisms are complementary, and combination strategies are under investigation.


Comments
Ashok Kumar
I can see why folks are excited about re‑using old drugs, especially when the hype sounds like another miracle cure. Still, we should remember that many promising lab results never make it to patients. So, a cautious optimism is the best we can afford.
Esther Olabisi
Sounds like the scientists finally found a way to give TB pills a career change 🙃. If this works, we might actually have something fun to talk about at the next oncology meeting! 🚀
Ivan Laney
Let me state the obvious: repurposing drugs is not a new gimmick, it is a pragmatic approach that any rational government should champion.
The United States has a proud history of turning civilian pharmaceuticals into battlefield medicine, and we should be proud of that legacy.
Cycloserine, a staple in the fight against drug‑resistant tuberculosis, presents an opportunity to leverage existing stockpiles without the bureaucratic red tape of novel compounds.
Its dual mechanism-targeting glutamate‑dependent metabolism and NMDA receptors-aligns perfectly with the current scientific consensus that metabolic flexibility is the Achilles’ heel of aggressive cancers.
The pre‑clinical data showing a 45 % reduction in glioblastoma xenograft volume is not a trivial number; it eclipses many first‑in‑class agents that never got past Phase I.
Moreover, the observed down‑regulation of PD‑L1 suggests a built‑in synergy with immunotherapy, a field where the United States leads the world.
Critics will point to the neuropsychiatric side‑effects, yet we have decades of safety data that can mitigate those concerns through proper monitoring.
Renal dosing adjustments are straightforward, and drug‑drug interaction profiles are well‑characterized, which means clinicians can adopt cycloserine without reinventing the wheel.
The ongoing trials NCT05432145 and NCT05511267 are precisely the kind of proof‑of‑concept studies that should receive swift regulatory support.
If the data hold, we could see a cost‑effective, globally accessible therapy that reduces dependence on expensive novel agents.
This is especially critical for low‑ and middle‑income countries that cannot afford the price tags of brand‑new oncology drugs.
The notion that “old antibiotics can’t fight cancer” is a relic of outdated thinking that ignores the plasticity of molecular pathways.
By embracing cycloserine, we also send a message that the medical establishment values resourcefulness over profit‑driven hype.
In short, the science is compelling, the logistics are manageable, and the potential public health impact is massive.
So, let us not waste time debating the merits of novelty when a proven, affordable drug is ready to step onto the oncology stage.
Vivian Annastasia
Oh great, another ‘miracle’ that will probably vanish once the pharma lobby gets a whiff of profit. The neuro‑psych side effects are adorable, as if we need more anxiety in our patients. And sure, let’s ignore the fact that two tiny Phase I studies won’t magically fix glioblastoma.
John Price
Looks promising but still early.
Erika Thonn
If we think of medicine as a river, cycloserine is a stone that once layed down can redirect the flow, even if we dont see the ripples until later.
Ericka Suarez
Our nation could lead the world by embracing this drug, turning a humble TB remedy into a crown jewel of cancer therapy-if only the elites would stop dithering.
Jake Hayes
The data are solid, the mechanism is sound, and the clinical path is clear; any further hesitation is unscientific.
parbat parbatzapada
Sure, they say it’s safe, but have they looked at the hidden side‑effects they don’t want us to see? I hear there’s a hidden agenda to push other, more profitable drugs later.
Casey Cloud
For clinicians interested in trying cycloserine start with the standard TB dose and monitor renal function and mental status weekly. Adjust dosing for eGFR below 30 and watch for interactions with ondansetron.
Rachel Valderrama
Let’s give a round of applause to the scientists who finally found a use for a TB pill-maybe next they’ll discover coffee cures insomnia!
Brandy Eichberger
Delighted to see such rigorous research; it’s refreshing when the scientific community steps beyond the usual hype and presents data with elegance.
Eli Soler Caralt
In the grand tapestry of pharmacology, cycloserine threads a subtle hue-perhaps a reminder that even the simplest compounds can whisper profound truths. 🌌
Eryn Wells
Loved the thorough overview! 🌟 It really helps bridge the gap between bench science and patient care for everyone reading.
Kathrynne Krause
What an exhilarating journey into drug repurposing! Your breakdown shines a kaleidoscopic light on possibilities and invites us all to picture a future where old meds get a second act.