
SSRI Hyponatremia Risk Calculator
Risk Assessment
Risk Assessment Results
More than 1 in 5 older adults in the U.S. are taking an SSRI for depression or anxiety. But for many, the medication that helps their mood may be quietly increasing their risk of a dangerous fall-or worse. Hyponatremia, a drop in blood sodium levels, is one of the most common and overlooked side effects of SSRIs in people over 65. And it doesn’t always come with obvious symptoms. Sometimes, the first sign isn’t nausea or headache-it’s a stumble on the stairs, a trip to the ER after a fall, or a hospital admission for confusion that no one could explain.
Why Older Adults Are at Higher Risk
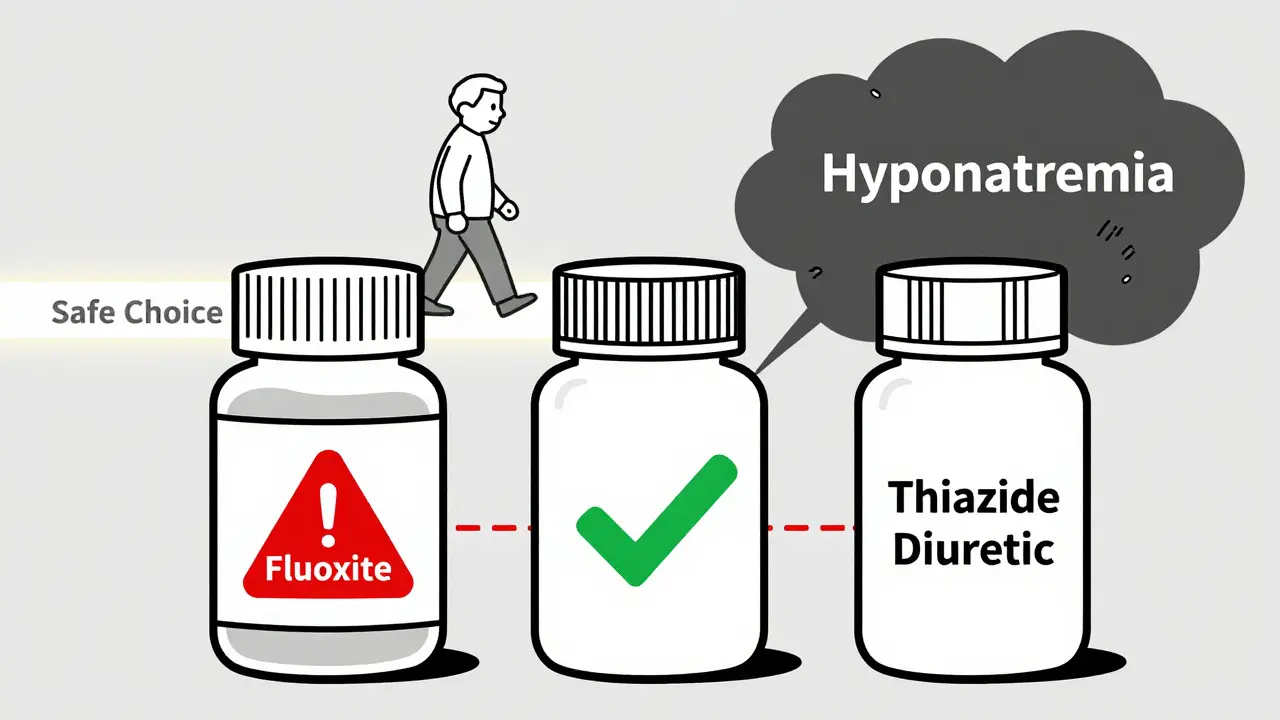
As we age, our bodies change in ways that make us more sensitive to medications. Our kidneys don’t filter as well. We have less total body water. Our hormones, like antidiuretic hormone (ADH), start to behave unpredictably. These changes mean that even small shifts in fluid balance can throw off sodium levels-and SSRIs make this worse. SSRIs cause something called SIADH: the syndrome of inappropriate antidiuretic hormone secretion. Normally, ADH tells your kidneys when to hold onto water. But when SSRIs overstimulate this system, your body holds onto too much water. That water dilutes your sodium. Your blood sodium drops below 135 mmol/L-and that’s hyponatremia. The risk isn’t the same for everyone. Older adults with a low body weight (BMI under 25), women, and those already taking thiazide diuretics (common for high blood pressure) are at highest risk. People with sodium levels starting below 140 mmol/L are also more likely to drop into dangerous territory. One study found that combining an SSRI with a thiazide diuretic increases hyponatremia risk by 24% to 27%. That’s not a small bump-it’s a red flag.Which SSRIs Are Riskiest?
Not all SSRIs are created equal when it comes to hyponatremia. Fluoxetine (Prozac) carries the highest risk among this class, with an event rate of over 6.5%. Sertraline and citalopram follow closely. Paroxetine and escitalopram have slightly lower rates, but still pose a real danger. Even SNRIs like venlafaxine (Effexor) are riskier than many doctors realize. While not SSRIs, they’re often prescribed alongside them-and carry a similar or even higher risk of sodium drops. On the flip side, some antidepressants have much lower hyponatremia risk. Mirtazapine (Remeron) is consistently flagged as one of the safest options for older adults. Bupropion (Wellbutrin) is another alternative, though it doesn’t work as well for everyone, especially those with severe anxiety. If someone has a history of falls, low sodium, or kidney issues, switching to one of these alternatives may be the smartest move.Hyponatremia Doesn’t Always Show Up in Blood Tests
Here’s the tricky part: many older adults with hyponatremia don’t feel sick. In fact, 30% to 40% of cases show no symptoms at all-until they fall. The subtle signs are easy to miss: slight dizziness when standing, unsteady walking, confusion that comes and goes, or just feeling "off" for no reason. These aren’t signs of dementia. They’re signs of low sodium. And that’s why falls happen. When sodium drops, brain cells swell. That affects balance, coordination, and judgment. A person might not even realize they’re at risk. They might think, "I’m just getting older," when really, their medication is silently destabilizing them. A 2024 review found that hyponatremia increases the risk of falls in older adults-but it didn’t quantify the exact number. That’s because no one has run a perfect study yet. But we know this: people with hyponatremia are more likely to fracture a hip, end up in the hospital, or die. And many of those cases could have been prevented.
What Should Doctors Do?
The American Geriatrics Society says SSRIs can be "potentially inappropriate" for older adults with a history of low sodium or fall risk. That’s a strong warning. But here’s the contradiction: some experts say you must check sodium before starting an SSRI and again at two weeks. Others say that even with testing, hospitalizations don’t drop. Why? Because checking sodium isn’t enough. You need a plan. If the test comes back low, what happens next? Is the medication stopped? Is fluid intake adjusted? Is the patient monitored daily? Too often, the test is done, the result is filed, and nothing changes. Best practice? Start with a baseline sodium test before prescribing. Then retest at 10 to 14 days. If sodium drops below 135, don’t wait. Talk about alternatives. If it’s below 130, stop the SSRI immediately and refer for medical evaluation. Mild cases (125-134) can often be managed with fluid restriction and close follow-up. Severe cases (below 125) need hospital care-too-fast correction can cause brain damage.What Can Patients and Families Do?
You don’t need to be a doctor to protect yourself or a loved one. Here’s what you can do:- Ask: "What’s my sodium level?" before starting any new antidepressant.
- Ask: "Is there a safer option for someone my age?" If you’ve had a fall or feel dizzy, say so.
- Watch for subtle changes: Is Mom walking slower? Is Dad forgetting where he put his keys more than usual? Is he drinking more water than normal?
- Check all medications. Are they on a diuretic? That combo is dangerous with SSRIs.
- If you’re on an SSRI and feel unsteady, don’t brush it off. Tell your doctor. Get a sodium test.
The Bigger Picture
SSRI use in older adults has jumped 34% since 2015. That’s good news for depression treatment-but bad news if we’re not watching for side effects. Hyponatremia-related hospitalizations now cost over $1.2 billion a year in the U.S. alone. New tools are emerging. Hospitals are using AI systems to flag high-risk combinations-like SSRIs plus thiazides-and automatically prompt sodium tests. Some clinics have cut emergency visits by 22% just by adding routine sodium checks and patient education. But the real breakthrough will come when we stop treating depression and fall risk as separate problems. They’re connected. A medication that helps mood can also break balance. And if we don’t connect those dots, we’re not helping-we’re harming.What Comes Next?
The National Institutes of Health just launched a $2.8 million study to figure out the best way to monitor sodium in older adults on antidepressants. Until we have those answers, stick to what we know:- Test sodium before and two weeks after starting an SSRI.
- Choose safer antidepressants like mirtazapine or bupropion for high-risk patients.
- Never ignore dizziness, confusion, or unsteadiness in an older adult on an SSRI.
- Don’t assume it’s just aging. It might be your medication.
Depression is real. It’s debilitating. But so are falls. So is brain swelling from low sodium. The goal isn’t just to treat the mind-it’s to protect the whole person. That means thinking beyond the prescription pad. It means asking the right questions. And sometimes, it means choosing a different path.
Can SSRIs cause falls in older adults?
Yes. SSRIs can increase fall risk in older adults, mainly through a side effect called hyponatremia-low blood sodium. This condition causes dizziness, confusion, and unsteady walking, which can lead to falls. Many people don’t realize their symptoms are medication-related, mistaking them for normal aging or dementia.
How do I know if my elderly parent has hyponatremia from an SSRI?
Symptoms are often subtle: mild confusion, dizziness when standing, weakness, nausea, or a recent fall without clear cause. Some people have no symptoms at all. The only sure way to know is a blood test for serum sodium. If they’ve been on an SSRI for less than a month and show any of these signs, ask their doctor for a sodium test immediately.
Which antidepressant is safest for older adults?
Mirtazapine (Remeron) is generally considered the safest antidepressant for older adults regarding hyponatremia risk. It has minimal impact on sodium levels. Bupropion (Wellbutrin) is another low-risk option, though it may not help anxiety as much. Avoid fluoxetine (Prozac) and venlafaxine (Effexor) if possible-both carry higher risks.
Should I stop my SSRI if I feel dizzy?
Don’t stop abruptly. Dizziness could be a sign of hyponatremia, but stopping suddenly can cause withdrawal symptoms. Call your doctor. Get a sodium test. If your sodium is low, your doctor may advise switching medications, reducing fluid intake, or adjusting your dose. Never make changes without medical guidance.
Is it necessary to check sodium levels before starting an SSRI?
Yes. Major guidelines recommend checking serum sodium before starting an SSRI in older adults-and again at 10 to 14 days after starting or increasing the dose. Even if the person feels fine, early detection can prevent serious complications like falls, seizures, or hospitalization. Skipping this step is a common oversight that puts lives at risk.
Can thiazide diuretics make SSRI side effects worse?
Absolutely. Thiazide diuretics (like hydrochlorothiazide) lower sodium on their own. When combined with SSRIs, the risk of hyponatremia jumps by 24% to 27%. This is one of the most dangerous drug combinations for older adults. If someone is on both, they should have their sodium checked every two weeks until stable-and consider switching either the diuretic or the antidepressant.


Comments
Steven Destiny
This is the kind of info that should be plastered on every pharmacy shelf. SSRIs aren't harmless candy-they're chemical levers that can flip your electrolytes like a switch. I've seen grandpas stumble because their doc just scribbled a script and called it a day. Time to stop pretending aging is just about wrinkles and creaky knees. It's about toxic drug combos nobody talks about.
Rajni Jain
my mom was on sertraline and kept falling but we thought it was just old age 😔 then one day she got confused and we got her sodium checked-128. they switched her to mirtazapine and she’s been walking like a new person. pls tell your dr to test sodium. it’s so simple but no one does it. i’m so glad i found this post.
Sandeep Jain
same here. my dad was on prozac and hydrochlorothiazide. he kept saying he felt "weird"-like his legs were heavy. we ignored it. then he fell and broke his hip. turns out his sodium was 124. the hospital doc said "this is classic". why didn't his psych doc know? why didn't the pharmacist flag it? this needs to be mandatory testing. not optional.
Brittany Fuhs
It's tragic, really. We live in an era where we medicate away every discomfort instead of addressing root causes-loneliness, lack of purpose, social isolation. SSRIs are a Band-Aid on a severed artery. And now we're surprised when the patient bleeds out from hyponatremia? The system is broken. We need holistic care, not pharmacological bandwagons.
Nikki Brown
OMG I KNEW IT 😭 My aunt was on citalopram and kept "forgetting" where her keys were... turns out she was hyponatremic. They told her it was "early dementia." I screamed at the doctor. Now she's on mirtazapine and she remembers my birthday again. 🙏 Stop normalizing brain fog. It's not aging-it's poisoning.
Peter sullen
Based on the current literature, the pathophysiological cascade initiated by SSRI-induced SIADH is clinically significant in geriatric populations, particularly those exhibiting diminished renal perfusion, reduced total body water, and concomitant diuretic usage. The clinical imperative necessitates baseline and serial electrolyte monitoring, with a threshold of 135 mmol/L serving as a critical intervention point. Failure to adhere to these evidence-based protocols constitutes a deviation from the standard of care.
Becky Baker
USA needs to stop letting foreign drug companies push these meds like candy. We’re the only country that lets ads sell antidepressants on TV. Meanwhile, grandma’s falling because some pharma rep told her doctor to prescribe Prozac. We need real healthcare-not corporate profit.
Erwin Asilom
This is exactly why we need better geriatric training in medical schools. I've reviewed dozens of charts where sodium levels were checked but never acted upon. The system isn't broken-it's asleep. Someone needs to own the follow-up. Not the nurse. Not the patient. The prescriber.
Sumler Luu
I appreciate the depth here. My mom’s on escitalopram and I’ve been watching her closely. She’s been a little off-balance lately. I’m scheduling the sodium test this week. Thanks for reminding me not to assume it’s just "getting older."
sakshi nagpal
As someone from India, I see this all the time. Elders are given SSRIs without any baseline tests. Families assume the doctor knows best. But when the elderly start wandering or forgetting meals, we blame memory loss. Not the pills. This article is a wake-up call for global geriatric care.
roger dalomba
Wow. A medical article that doesn't sound like a pharmaceutical ad. Shocking.
Sophia Daniels
SSRIs are the silent killers of the elderly. They don’t kill with overdoses-they kill with a stumble. A fall. A fractured hip. A hospital bed. A funeral. And the worst part? The doctor smiles and says, "It’s just aging." No. It’s negligence wrapped in a prescription bottle. 🚨
Fabio Raphael
What’s the data on mirtazapine and weight gain in older adults? I’ve heard it causes appetite spikes. Is that a bigger risk than hyponatremia? Just wondering if there’s a trade-off we’re not talking about.
Amy Lesleighter (Wales)
my grandma took wellbutrin after a fall. no dizziness. no confusion. just calm. she still cries sometimes but she walks without a cane. maybe the answer isn’t more drugs-it’s the right one.
Natasha Sandra
So glad I read this before my mom started a new med! 💕 I’m printing this out and taking it to her appointment. She’s gonna be so mad I’m being "overprotective"... but I’d rather be annoying than bury her. 💔❤️