Biologics: What They Are, How They Work, and What You Need to Know
When you hear biologics, medicines made from living organisms like cells or proteins, not chemically synthesized like traditional pills. Also known as biologic drugs, they’re engineered to target specific parts of your immune system—unlike older drugs that blanket the whole body. These aren’t your average tablets. They’re injectable or infused treatments that changed the game for autoimmune diseases, cancer, and severe asthma. If you’ve been told you need one, you’re not alone—millions use them every year.
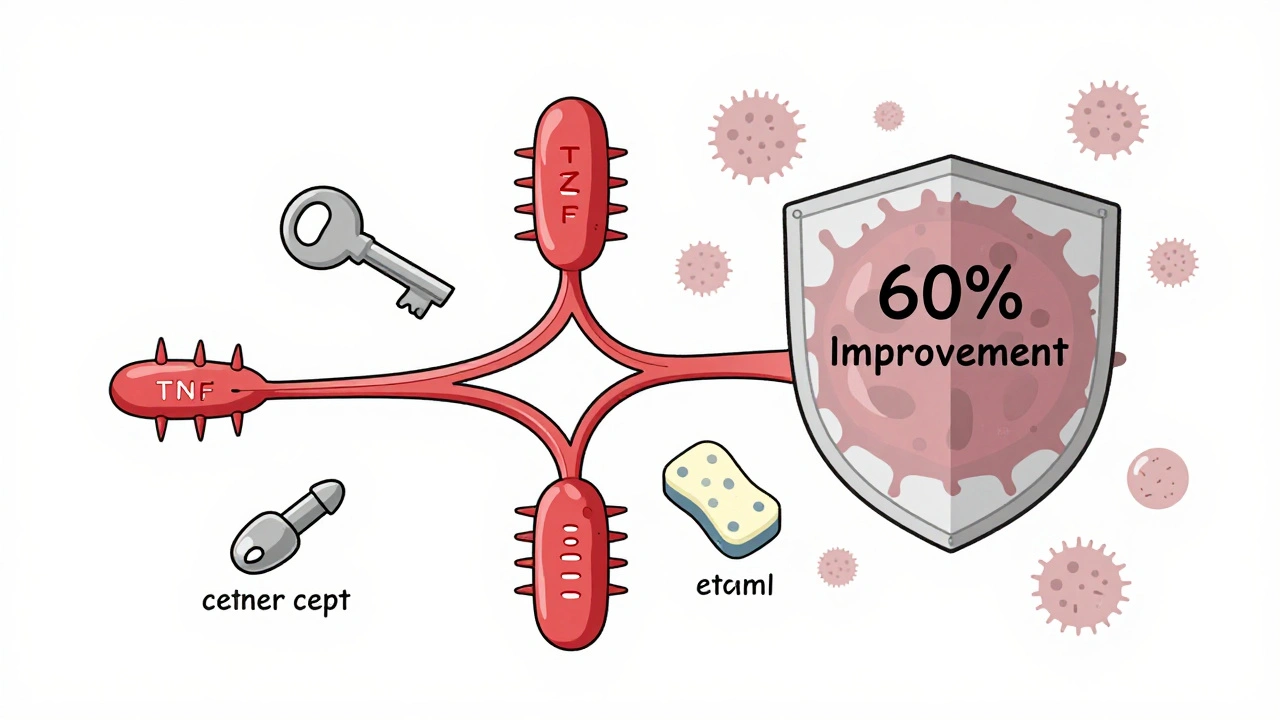
Biologics work by blocking specific proteins or cells that cause inflammation or overactive immune responses. For example, in rheumatoid arthritis, a chronic condition where the immune system attacks joints, biologics stop TNF-alpha or IL-6 from triggering swelling and pain. In Crohn’s disease, a type of inflammatory bowel disease, they shut down the immune signals that wreck the gut lining. But they’re not magic. They can increase infection risk, require regular monitoring, and cost thousands per month. Some people respond amazingly; others don’t respond at all. That’s why doctors often try older drugs first.
These treatments are closely tied to immunosuppressants, drugs that calm the immune system to prevent it from attacking the body. But unlike general immunosuppressants like prednisone, biologics are precision tools. They don’t weaken your whole defense system—just the part causing trouble. That’s why they’re preferred for long-term use, even though they come with their own side effects. You’ll need blood tests to check for liver stress, infections, or even rare nerve issues. And if you’re planning surgery or traveling, your doctor will likely pause them.
What you won’t find in most ads is how often biologics are used alongside other treatments. Many patients take them with methotrexate or low-dose steroids to boost effectiveness. Others switch between different biologics when one stops working. And while they’re often linked to autoimmune diseases, they’re also used in psoriasis, ulcerative colitis, and even some types of lung disease. The real question isn’t just whether they work—it’s whether they work for you, given your health history, lifestyle, and budget.
Below, you’ll find real-world stories and data on how biologics fit into daily life—what works, what doesn’t, and what you should ask your doctor before starting one. From cost hurdles to unexpected side effects, these posts cut through the hype and give you what matters.
Future Biosimilars: Upcoming Patent Expirations and Market Entry
Biosimilars are set to transform healthcare as major biologics like Keytruda and Eylea lose patent protection between 2025 and 2030. Learn how these complex, lower-cost alternatives are entering the market, what’s holding them back, and what it means for patients and providers.
read moreTNF Inhibitors and Cancer Risk: What You Need to Know About Biologics and Immunosuppression
TNF inhibitors like Humira and Enbrel are powerful treatments for autoimmune diseases, but concerns about cancer risk persist. Latest studies show no overall increase in cancer risk, with important differences between drugs and personal risk factors that guide safe use.
read more